Heart disease is the leading cause of death in pregnancy. Although women with high-risk cardiac conditions can be identified, the majority of deaths occur without such pre-existing severe cardiac disease. Coronary artery disease is an increasing cause. Previous reports on heart disease in pregnancy have focused on tertiary-centre and non-UK populations. We report a UK District General Hospital (DGH) experience. We recorded all pregnant women referred to a dedicated DGH cardiology service in Bromley between August 2004 and August 2007. One hundred and three women were referred, including 37 with murmurs or known valve disease, 31 palpitations or arrhythmias, 13 congenital heart disease and eight hypertension. Of the women presenting with a murmur, only one, a recent immigrant, had a significant cardiac condition requiring treatment. Three women with arrhythmias required admission but none were life-threatening. Four women required admission for heart failure, two with peri-partum cardiomyopathy and two with previous hypertension. Only two women were referred with chest pain, neither had ischaemia. Tertiary referral was required in cases of heart failure, an increased risk of aortic rupture or severe mitral stenosis, but all other women were managed safely in a DGH. Seventy per cent of women only needed one clinic visit.
In conclusion, the majority of pregnant women referred to a DGH cardiology service are in the previously defined low-risk group. Cardiac symptoms or signs in UK-born pregnant women without known heart disease are unlikely to represent high-risk cardiac disease but recent immigrants may have significant undiagnosed disease. Chronic hypertension is a risk factor even if controlled at the start of pregnancy. Ischaemia is an increasing problem.
Background
Heart disease is the leading cause of death in pregnant women and, despite advances in cardiology, maternal deaths from cardiac disease have increased over the past 20 years.1 Cardiac conditions such as pulmonary hypertension, severe valve disease, cyanotic and complex congenital heart disease carry a high mortality2 and need specialist care.3 It has been recommended that pregnant women with cardiac disease should be managed in tertiary centres,4 and many cardiologists caring for pregnant women have a background in congenital heart disease, necessary for the management of complex congenital heart disease.
Previously reported series of women with heart disease in pregnancy have focused on the experience in a tertiary setting,5,6 in women with congenital heart disease7 or in countries with a high prevalence of rheumatic valvular disease.8,9 However, the majority of women in the UK have their obstetric care outside the tertiary setting, without an on-site multi-disciplinary team of obstetricians, cardiologists, anaesthetists and obstetric physicians with experience of such conditions. Most cardiac deaths related to pregnancy are not in women with previously identified high-risk congenital or valve disease. The leading causes of maternal death in the latest Confidential Enquiry into Maternal and Child Health (CEMACH) report1 were ischaemic heart disease, cardiomyopathy and aortic dissection, conditions commonly presenting to District General Hospitals (DGHs), which may not be apparent at the start of pregnancy.
The aims of this study were to determine the spectrum of cardiac conditions in pregnant women presenting to a DGH, to assess the ability to triage their risk effectively in this setting and to assess the impact on a DGH cardiology department of setting up a dedicated obstetric cardiac service.
Methods
A dedicated cardiology service for women with known or suspected heart disease in pregnancy was set up and run by a single cardiologist at Bromley Hospitals NHS Trust, a DGH in South East London, serving a population of 300,000 with 3,400 deliveries per annum. A prospective survey was carried out of all women referred over a three-year period from August 2004–2007. For all women, the principal reason for referral was recorded, as was the final diagnosis and the risk status at presentation. As an indicator of morbidity, the number of women requiring admission to hospital for cardiac reasons was noted. The number of women for whom tertiary referral was made was also recorded. As a measure of the impact on the cardiac department, the number of women requiring more than one out-patient visit and the number of cardiac investigations carried out were also noted.
Results
A total of 103 women were referred to the service. The most frequent reasons for referral were murmurs or known valve disease (n=37) and palpitations or known arrhythmias (n=31). There were 13 women with congenital heart disease, eight with hypertension and five with shortness of breath. Others included hypertrophic cardiomyopathy, syncope and collagen disease.
Valve disease
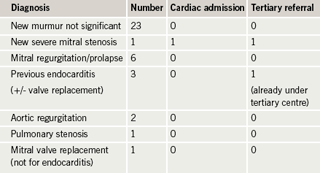
Of the 24 women referred with a newly diagnosed murmur, all but one had no significant abnormality (table 1). The only significant newly diagnosed valve disease was a case of severe mitral stenosis in a recent immigrant, who was admitted electively for initiation of beta blockers, and referred to a tertiary centre where she delivered with good outcome for mother and baby. Of those with known valve disease, all were mild or moderate and did not fall in the high-risk group. None required admission and the only woman seen in a tertiary centre was already under their care. Apart from the woman with mitral stenosis there were no cases of severe valve disease or significant left heart obstruction. The women with previous valve replacement did not have mechanical valves so anticoagulation was not an issue. The replacement valves were functioning well. Of the 37 women referred with murmurs or valve disease, only six required more than one out-patient visit and only one was in the high-risk category according to European Society for Cardiology (ESC) guidelines.3
Arrhythmias
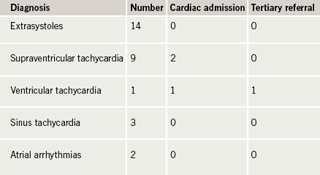
Palpitation was a common presenting symptom but only one of those presenting with palpitations without a previously known cardiac condition required admission (table 2). This was a woman who presented to Accident & Emergency (A&E) with a newly diagnosed nodal tachycardia. This was not haemodynamically compromising or life-threatening so would be classed as low risk.3 None required tertiary referral. One woman, with a previous atrial septal defect (ASD) repair and initially no significant left ventricular (LV) dysfunction or pulmonary hypertension, developed LV failure during pregnancy and was noted to have non-sustained episodes of ventricular tachycardia. With medical therapy she delivered in a tertiary centre with good outcome for mother and baby. One woman with known supraventricular tachycardia (SVT) attended A&E with an episode of re-entrant tachycardia, which was not haemodynamically compromising, therefore, low risk. This was treated and she had no further problems. Ten of the 31 women presenting with palpitations or arrhythmia required more than one out-patient visit. Only the woman with ventricular tachycardia (VT) and impaired LV function would classify as high risk, but initial evaluation early in pregnancy would have put her in a low-risk group.
Congenital heart disease
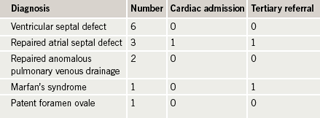
None of the women in our series had complex or cyanotic congenital heart disease, or pulmonary hypertension, and none had complications related to their congenital heart condition (table 3). The only woman requiring admission was the case mentioned previously under arrhythmias. One other, a woman with Marfan’s syndrome, was referred to a multi-disciplinary tertiary clinic in view of her potential risk for aortic rupture, and delivered with good outcome for mother and baby. Six out of 13 needed more than one out-patient visit during the pregnancy and nine required cardiac investigations, so their impact on the clinic was relatively high.
Hypertension/cardiomyopathy
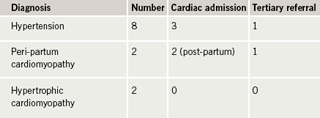
Of the eight women with hypertension, five had previously diagnosed hypertension, of whom two developed heart failure requiring admission (table 4). One woman was transferred to a tertiary centre in the second trimester, where the pregnancy was terminated. The other woman developed heart failure following delivery of a live baby and was treated successfully at the DGH. These women were referred to the cardiology service as in-patients after the onset of heart failure. Previous blood pressure control had not identified them as high risk.3 The three women without previously known hypertension had no heart failure, but one required admission for blood pressure control and subsequently mother and baby were well. Two women with no previous cardiac history, who had remained well during pregnancy, developed peri-partum cardiomyopathy after delivery, requiring admission. One was transferred to a transplant centre. The women with hypertrophic cardiomyopathy (HCM) in our study did not have significant LV outflow obstruction or arrhythmia, so were classified as low risk.
Other conditions
Two women presented with chest pain, which was found to be non-cardiac. No cases of ischaemic heart disease were diagnosed. Of the five women presenting with shortness of breath, apart from the two women with peri-partum cardiomyopathy, one case of pulmonary fibrosis was diagnosed. A woman with Ehlers-Danlos syndrome was referred directly to a tertiary centre.
Cardiac investigation
Sixty women (58%) underwent echocardiography and 25 (24%) 24-hour electrocardiogram (ECG) monitoring. Thirty-one (30%) required more than one out-patient visit.
Discussion
Women with a very high cardiac risk in pregnancy can be predicted by the presence of factors including prior cardiac events, arrhythmia, poor functional class, cyanosis, left heart obstruction and reduced LV function.2,6 The presence of more than one of these factors raises the risk of an adverse event to 75% compared with 5% in women with no risk factors.10 Conditions identified as carrying a high risk include pulmonary hypertension, previous peri-partum cardiomyopathy, Marfan’s syndrome with an aortic root dimension greater than 40 mm, mechanical valves, cyanotic heart disease and other complex congenital heart disease.2,3,6,10
In our study, the proportion of women with identified high risk was small, as may be expected in a DGH population, since women with very high-risk cardiac conditions are likely to be under the care of tertiary-centre cardiologists prior to pregnancy. Only four women required specialist referral during pregnancy for known or newly diagnosed pre-existing high-risk conditions, namely mitral stenosis, Ehlers-Danlos syndrome, pulmonary fibrosis and Marfan’s syndrome. Triage of these conditions was successful and no high-risk women were missed. The remaining 99 women would have been classified as low risk at the start of pregnancy. According to ESC guidelines, hypertensive women with blood pressure 140–160/90–110 mmHg are low risk, but, in our group, heart failure was the first presentation to cardiology in women with blood pressure levels that had not triggered referral for blood pressure control. Our women with peri-partum cardiomyopathy had no predictive risk factors. Thus, even apparently low-risk women may have significant morbidity.
Despite the ability to predict high-risk cases and the emphasis on identification of such women, it is interesting that in the latest CEMACH report the majority of deaths were not predictable by these criteria. Myocardial infarction or ischaemia caused 16 out of 47 deaths, plus four out of 34 late deaths. Aortic dissection caused 9/47 deaths, of these, three women probably had Marfan’s syndrome, but this was not diagnosed. Three women who died of aortic dissection were morbidly obese, which should also be considered a risk factor. Peri-partum cardiomyopathy caused 12/34 late deaths. In contrast, congenital heart disease was the cause of 3/47 deaths plus 2/34 late deaths, while pulmonary hypertension caused 3/47 deaths. Thus, most of the women who subsequently died would have fallen into the relatively low-risk group and may well have presented to a DGH.
DGH cardiologists have great experience of ischaemic heart disease, hypertension and heart failure, so may be better able to manage these common conditions occurring in an uncommon setting, but need a high index of suspicion and experience of what is normal in pregnancy. Although the majority of women in our study were managed successfully in the DGH, with no problems occurring due to lack of tertiary facilities, cases with high-risk features were referred to St Thomas’. This is a tertiary centre with a multi-disciplinary team, including an obstetrician with an interest in cardiology, obstetric physician, cardiologists and obstetric anaesthetists. Therefore, while we would suggest that the majority of pregnant women referred to DGH cardiac clinics are low risk and do not require referral to a tertiary centre, there are advantages for the few who require more intensive multi-disciplinary care, particularly out of hours, as well as the availability of interventional cardiologists and cardiothoracic surgeons. However, primary and secondary care clinicians need to be alert to the possibility of complications even in low-risk women.
Although arrhythmias are a recognised risk factor, in our group, the symptom of palpitations was generally benign and no arrhythmias causing significant morbidity occurred in women without known cardiac disease. The majority of women presenting with palpitations could be reassured after one visit. Similarly, the majority of women found to have a murmur could be reassured. This may not apply to populations with a high proportion born outside the UK in areas with a higher prevalence of rheumatic heart disease, particularly those who have not been under medical care here.
Shortness of breath, to some degree, is almost universal in pregnancy, but in our group of women referred to cardiology it was an important indicator of disease. All of the women presenting with shortness of breath and found to have a significant cardiac or pulmonary cause had physical signs in the chest and/or a fall in oxygen saturations at rest or on exertion, in contrast to those in whom no significant cause was found. Women with a history of hypertension prior to pregnancy should be considered at risk, and cardiologists should have a low threshold for considering heart failure. In contrast, only two women in our study were referred with chest pain and neither of these had a cardiac cause. Given the increasing incidence of ischaemic heart disease in the pregnant population and its status now as the leading cause of death in pregnancy, doctors managing pregnant women need to retain a high index of suspicion, as the diagnosis of ischaemic heart disease may be overlooked in pregnancy. Previous estimates of myocardial infarction in pregnancy have been 1:16,000–36,000 deliveries. In addition to the usual risk factors for coronary artery disease, increased risk of myocardial infarction has been related to maternal age >30 years, multi-parity, non-Hispanic white or black race, pre-eclampsia, transfusion and post-partum infection.11,12
The impact on the resources of the cardiac department was not large. For this population, there was a mean of three women referred per month, 70% of whom could be discharged after the first clinic attendance. We had a high rate of referral for cardiac investigations and, with the findings of this study, the rate of requesting echocardiography and 24-hour ECG monitoring has reduced, with the reassurance that newly diagnosed murmurs and palpitations in our population are unlikely to represent significant disease.
Conflict of interest
None declared.
Key messages
- Most pregnant women presenting to a District General Hospital (DGH) cardiology clinic are low risk
- UK-born women presenting during pregnancy with murmurs or palpitations are unlikely to have significant cardiac disease
- Shortness of breath is common, but may indicate significant disease, particularly if associated with physical signs or a fall in oxygen saturation on exertion
- Ischaemic heart disease is an increasing cause of death in pregnancy
- Non-UK-born women, and those with previous hypertension, are at higher risk of cardiac complications
References
- Lewis G (ed). The Confidential Enquiry into Maternal and Child Health (CEMACH). Saving mothers’ lives: reviewing maternal deaths to make motherhood safer – 2003–5. The seventh report on confidential enquiries into maternal deaths in the United Kingdom. London: CEMACH, 2007.
- Thorne SA, Nelson-Piercy C, MacGregor A. Risks of contraception and pregnancy in heart disease. Heart 2006;92:1520–5.
- Oakley C, Child A, Iung B. Expert consensus document on management of cardiovascular disease during pregnancy. The task force on the management of cardiovascular disease during pregnancy of the European Society of Cardiology. Eur Heart J 2003;24:761–81.
- Ray P, Murphy GJ, Shutt LE. Recognition and management of maternal cardiac disease in pregnancy. Br J Anaesth 2004;93:428–39.
- Tan J, de Swiet M. Prevalence of heart disease diagnosed de novo in pregnancy in a West London population. Br J Obstet Gynaecol 1998;105:1185–8.
- Siu SC, Sermer M, Harrison DA et al. Risk and predictors for pregnancy-related complications in women with heart disease. Circulation 1997;96:2789–94.
- Khairy P, Ouyang DW, Fernandes S, Lee-Parritz A, Economy KE, Landzberg MJ. Pregnancy outcomes in women with congenital heart disease. Circulation 2006;113:517–24.
- Avila WS, Rossi EG, Ramires JA et al. Pregnancy in patients with heart disease: experience with 1,000 cases. Clin Cardiol 2003;26:135–42.
- Abdel-Hady ES, El-Shamy M, El-Rifai AA, Goda H, Abdel-Samad A, Moussa S. Maternal and perinatal outcome of pregnancies complicated by cardiac disease. Int J Gynaecol Obstet 2005;90:21–5.
- Siu SC, Sermer M, Colman JM et al. Prospective multicentre study of pregnancy outcomes in women with heart disease. Circulation 2001;104:515–21.
- James AH, Jamison MG, Biswas MS, Brancazio LR, Swamy GK, Myers ER. Acute myocardial infarction in pregnancy: a United States population-based study. Circulation 2006;113:1564–71.
- Ladner HE, Danielsen B, Gilbert WM. Acute myocardial infarction in pregnancy and the puerperium: a population-based study. Obstet Gynecol 2005;105:480–4.
