Syncope, a transient loss of consciousness, can present to the clinician in a variety of ways. The most important tool for the clinician is the history, not only from the patient but also from a witness of the collapse, if available. Clinicians should be aware of the possibility that a patient or carer may unwittingly lead him or her in the wrong direction in attempting to describe falls or fits.
Misdiagnosis of epilepsy in the syncopal patient is well recognised. Data brought before Parliament have indicated at least 74,000 cases of misdiagnosis of epilepsy in England alone, at a cost of £184 million to the National Health Service (NHS), and incalculable cost to patients. The All-Party Report from 2007 only refers to patients misdiagnosed and mistreated with anticonvulsants, there are many more patients in whom epilepsy is ‘equivocal’, but who often have to bear the stigma of diagnosis.
In discussions about syncope, definitions are important. Syncope is a sudden, brief loss of consciousness due to a reduction in blood flow to the brain and, thus, of its oxygenation. With loss of consciousness there is collapse that may or may not be associated with jerking of the limbs. This can lead to confusion in the separation of epilepsy from syncope and we know that approximately 10% of patients diagnosed as having epilepsy probably suffer from syncope.
Syncope is a frightening symptom, which renders the sufferer, and those who are close, concerned about the diagnosis. In particular they will be worried about continuing the activities of normal life without social isolation due to the embarrassment and stigma of collapsing in public. Throughout the clinical pathway keeping the patient central to the process and supported remains vital. Support for both the patient and the professional can be sought at www.stars.org.uk
1. Is this syncope?
 On the initial presentation the patient will not mention syncope but will use terms of common speech. They may say that they have ‘fallen’, ‘fainted’ or ‘had a blackout’. A witness may state that they have fitted. It is important to assist the patient to change these general terms into more exact medical language. Start at the point where they felt normal and take them through what happened from the onset of symptoms to full recovery. When did they realise that they were not well, why was this, were there disturbances of vision, sound or smell? Did they ‘fall’; do they remember the fall or just being on the floor? How quickly did they come round? How did they feel? Did they hurt themselves? Were they incontinent? Were there witnesses? Did they comment on duration, movement during unconsciousness and pallor?
On the initial presentation the patient will not mention syncope but will use terms of common speech. They may say that they have ‘fallen’, ‘fainted’ or ‘had a blackout’. A witness may state that they have fitted. It is important to assist the patient to change these general terms into more exact medical language. Start at the point where they felt normal and take them through what happened from the onset of symptoms to full recovery. When did they realise that they were not well, why was this, were there disturbances of vision, sound or smell? Did they ‘fall’; do they remember the fall or just being on the floor? How quickly did they come round? How did they feel? Did they hurt themselves? Were they incontinent? Were there witnesses? Did they comment on duration, movement during unconsciousness and pallor?
2. Maybe this is not syncope?
 Through the history there may be points that suggest that this is not syncope but a loss of consciousness due to another cause. The distinction between syncope and epilepsy is a difficult process and will influence the route of referral. If movements are tonic–clonic, continue for more than 15 seconds and involve the whole of a limb or limbs, this would suggest epilepsy. In comparison, irregular movements of short duration affecting only the distal parts of the limbs might suggest only cerebral hypoxia. If confusion following the attack lasts over 5–10 minutes, this may also be suggestive of an epileptic seizure.
Through the history there may be points that suggest that this is not syncope but a loss of consciousness due to another cause. The distinction between syncope and epilepsy is a difficult process and will influence the route of referral. If movements are tonic–clonic, continue for more than 15 seconds and involve the whole of a limb or limbs, this would suggest epilepsy. In comparison, irregular movements of short duration affecting only the distal parts of the limbs might suggest only cerebral hypoxia. If confusion following the attack lasts over 5–10 minutes, this may also be suggestive of an epileptic seizure.
In older people with falls a clear history may not be available. There may have been no witness of the incident and poor memory may mean events leading to the incident are unclear. Without a history of a stumble or fall then there should be a suspicion of syncope.
Older people can experience syncope without realising that it has happened. This renders the history unreliable without a witness. A full falls assessment in the patient’s own environment is essential.
People can collapse without losing consciousness due to other causes, such as paroxysmal benign positional vertigo and drop attacks. If there is a suspicion of collapse without loss of consciousness specialist consultation will be necessary with either an ear, nose and throat (ENT) surgeon or a neurologist. Careful definition of the term dizziness, meaning light-headedness, and giddiness, implying rotation, is important in assessment of these conditions.
3. What did the witness see?
The evaluation of a patient with syncope is greatly enhanced by a witness of the collapse. They need to be questioned about what happened from the onset of the attack to full recovery from it. What did they see, did the person become pale or confused before that attack. Were there no signs of problems until the attack? Did they jerk or move during the attack? What were these movements like? When did consciousness return? In this era of the mobile phone, filming of the attack can be encouraged so a more experienced eye can consider the situation.
When discussing the situation with the witness, remember they are affected by the event. Often they have seen a relation or close friend collapse with all the concern of sudden death or disabling illness. They may have drawn their own conclusions about what has happened, the diagnosis and what intervention is needed. Careful discussion is required to identify clearly what was seen and avoid the interpretation of events by the witness.
In repeated episodes of collapse the regular witness, friends and family need to be aware of simple first aid and safety. Although, as professionals, we may feel that these basic steps are understood, there should be no assumption made. Inform the witnesses to allow the person to lie down with their legs elevated and remove potential hazards.
4. What has gone before?
 Syncope needs to be put in the context of previous medical history. Is there known structural heart disease such as valvular disease or heart failure? Has the patient a past history of angina or myocardial infarction?
Syncope needs to be put in the context of previous medical history. Is there known structural heart disease such as valvular disease or heart failure? Has the patient a past history of angina or myocardial infarction?
Has there been a previous history of blackout, especially in youth? When was this and was a diagnosis established at the time? What steps were taken? Has there been a previous diagnosis of epilepsy made? If so, how was this diagnosis made?
5. Where did the symptoms come from?
Not only does the sufferer need to be considered but family history also needs to be considered. Is there a history of sudden cardiac deaths? These can masquerade as unexpected deaths that have been explained away, drowning or road traffic accidents. Is there a known family history of an inherited cardiac condition?
It is also of interest to know if their parents or other family members are fainters. It has been observed that people who faint are more likely to have come from parents who were also fainters.
6. Carry out an examination
A clinical examination is always vital and should be comprehensive.
Starting at the pulse, this should be assessed by manual palpation for rhythm and rate. Is there a bradycardia? Is the rhythm regular?
A full assessment of blood pressure both supine and erect is necessary. The blood pressure should be taken after lying for 10 minutes and then several times in the few minutes after standing, where a fall of 20 mmHg in systolic or to <90 mmHg, or a fall in diastolic of 10 mmHg are considered abnormal and strongly suggestive of orthostatic hypotension.
The cardiovascular examination should involve a detailed auscultation of the heart to identify valvular lesions or signs of heart failure.
A general neurological assessment should be undertaken, seeking gross neurological deficit. The gait should be observed to see if there are abnormalities that make falls likely.

If there is a rotational or vertiginous element in the history, a simple Dix-Hallpike assessment should be performed to check for benign paroxysmal positional vertigo. If this is positive, then assessment may be required from an ENT specialist. It is important to note that benign paroxysmal positional vertigo is not associated with loss of consciousness, and if the history is suggesting blackout, then these findings may be coincidental.
7. Undertake investigations
Any patient presenting with syncope or a disturbed period of consciousness should undergo simple investigations. These may include blood chemistry and blood count.

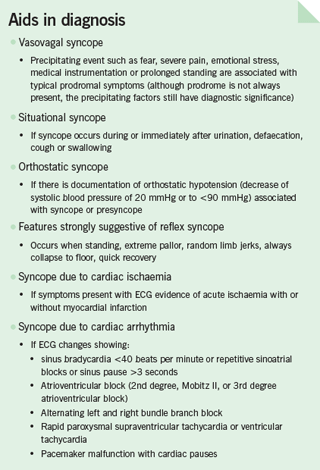
An electrocardiogram (ECG) is a vital part of the assessment. A normal ECG is an excellent prognostic feature. Changes that should raise concern include:
- Bradycardia: <40 beats per minute (except in athletes) or pauses >3
seconds - Mobitz II, 2nd, 3rd degree atrioventricular (AV) block
- Alternating right and left bundle branch block
- Rapid supraventricular tachycardia
- Ventricular tachycardia
- Cardiac ischaemia
- Myocardial infarction
- Wolff-Parkinson-White syndrome
- Long QT interval
- Brugada syndrome.
Unless the attacks are happening on a daily or very frequent basis, 24-hour ECG monitoring reveals nothing. A normal 24-hour ECG without symptoms does not further the diagnosis at all and should not be seen as reassuring.
8. What is the prognosis?
 Patients presenting with any problem want to know if they will come to any harm. This is such a complex area that it can be difficult to give assurances. However, in young healthy people with a normal ECG and a suggestion of neurally mediated (vagal) or rarely orthostatic hypotension the prognosis is excellent. The presence of structural heart disease, independent of the cause of syncope, reflects a poor prognosis.
Patients presenting with any problem want to know if they will come to any harm. This is such a complex area that it can be difficult to give assurances. However, in young healthy people with a normal ECG and a suggestion of neurally mediated (vagal) or rarely orthostatic hypotension the prognosis is excellent. The presence of structural heart disease, independent of the cause of syncope, reflects a poor prognosis.
9. Offer support
No individual chooses to become a patient. When they become involved in medical services for blackouts they can feel isolated and alone. Syncope does not have the general public awareness of other cardiac problems, such as myocardial infarction, or neurological complaints, such as stroke and epilepsy. Patients can often feel embarrassed by their symptoms and choose not to go out for fear of collapsing in public.
Support should be offered. Further support is available to the patient from the Syncope Trust at www.stars.org.uk who have published information regarding causes of collapse, interventions and patient checklists to assist the patient in assessing their own history of events and give detailed information to the clinician. The information on Syncope and Falls in the Elderly (SaFE) series of patient information leaflets gives easy accessible information to assist in symptom management.
10. To whom to refer?
Clearly syncope is a complex mix of possible diagnoses. There are people who have infrequent collapses of a neurally mediated pattern who may need no further assessment. However, it does not sit comfortably in any of the traditional specialties. From the carefully collected history it may be suggestive of a referral to a particular traditional speciality.
Chapter 8 of the National Service Framework (NSF) in cardiology specifically stated the need for specialist syncope services, however, these are still not widely available. When available these services are generally multi-disciplinary teams including cardiologists, elderly care specialists and neurologists.
The investigation is well suited to the general practitioner with special interest (GPwSI), with the generalist knowledge of the general practitioner enhanced by further specialist training. With support from local hospitals for the provision of tilt-table testing and rapid access to pacemaker services, if required, this model has been demonstrated to be effective.
The widespread availability of implantable loop recorders (ILRs) can greatly enhance the likelihood of diagnosis, and this procedure will soon also be possible in primary care, with the potential to improve patient care.
Conflict of interest
None declared.
