Direct current cardioversion (DCCV) to restore sinus rhythm (SR) in patients with persistent atrial fibrillation (AF) remains a therapeutic option, though recent studies have questioned its need and value in the longer term.
Having set up a new DCCV service at this Trust, it was appropriate to assess the short- and longer-term success rates in restoring SR in patients undergoing the procedure of cardioversion for persistent AF. Over a period of just over four years, 110 AF patients were cardioverted, and SR was immediately restored in 80 (73%). At a median of six weeks later, 54 (49%) of the successfully cardioverted patients remained in SR. In the longer term, we were able to confirm that just 22 (20%) of the patients we successfully cardioverted were still in SR, a mean of 47 weeks after the procedure. Thus, despite a high initial success rate, the relapse rate appears to be considerable and brings into question the value of performing this procedure electively in patients with persistent AF.
Introduction
We previously described a new service for the provision of day-case direct current cardioversion (DCCV) for patients with atrial fibrillation (AF) consisting of monthly dedicated DCCV lists in an operating theatre, with an anaesthetist and an operating department assistant providing anaesthesia, and cardiology medical staff performing the cardioversion.1 Our new service considerably reduced the delay to DCCV, which is known to be more successful the earlier it is undertaken after the onset of AF. Recent studies have suggested that the benefits of restoring sinus rhythm (SR; a strategy known as ‘rhythm control’) are not particularly advantageous over merely accepting the AF and improving symptoms by efforts to reduce the heart rate (a strategy called ‘rate control’).2,3 However, the National Institute for Health and Clinical Excellence (NICE)4 still recommends that it would be reasonable to try to restore SR in certain patients, such as those who are symptomatic, younger patients, those presenting for the first time with lone AF, those with AF secondary to a treated/corrected precipitant and those with congestive heart failure. This report details the immediate and longer-term success rates at restoring and maintaining SR in consecutive AF patients sent to our new service for DCCV.
Methods
The hospital case notes of all patients listed for our elective DCCV service between December 2004 and January 2009 were studied during March 2009. Demographic information was obtained for each patient, together with details of the DCCV undertaken, or reasons for cancellation or delay. Our initial cardioversion protocol was for sequential synchronised monophasic shocks of 50 J; 100 J; 200 J; 300 J and 360 J, until SR was restored or all shocks were delivered, after which the procedure was terminated. In summer 2007, we moved to biphasic defibrillators and the protocol changed to 50 J; 100 J; 150 J (up to twice). For those in whom DCCV was undertaken, note was made of the number of shocks delivered, and whether sinus rhythm (SR) was restored by the end of the procedure, by the time patients went home from the day-case unit, and at first follow-up visit. The last contact the patient had had with the hospital was also determined, and note of whether SR persisted at that time. At each of these contacts, details of the type and number of anti-arrhythmic drugs prescribed was recorded.
Results
Planned DCCV lists, initially for four patients per list though more recently for up to six patients (which depended on availability of beds on the day-case unit), were undertaken on a monthly basis from December 2004 until October 2005. Then, because of a reduction in referrals, the lists reduced to bi-monthly from December 2005 until demand increased in February 2008, when lists became monthly once again until January 2009. During this period, 153 DCCV admissions were scheduled, for 120 men (mean age 62 years, range 42–85 years) and 33 women (mean age 68 years, range 58–81 years). The AF had been present for a mean of eight months (median five months, range one to 96 months).
Of these planned procedures, 43 (28%) had to be cancelled for the following reasons: the dose of warfarin, as measured by the International Normalised Ratio (INR), was too low (INR below 2.0) on the day before the procedure in 26 cases (60% of the cancellations); 13 patients (30% of the cancellations) were in SR on an electrocardiogram (ECG) done the day before the procedure; three patients cancelled their procedure for personal reasons; and one patient refused informed consent to the procedure.
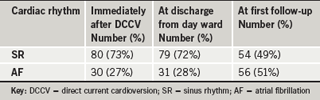
A total of 110 patients underwent a cardioversion. At the time of their DCCV, 27 patients were taking digoxin, 74 were on beta blockers, 11 on rate-limiting calcium channel blockers, 12 on amiodarone and one on flecainide. Thirteen patients were prescribed no anti-arrhythmic medication, 71 patients were on one, 24 were on two and two patients were on three anti-arrhythmic drugs. At cardioversion a mean of 3.3 shocks were delivered (range 1–5) with a mean total energy delivery of 485 J (range 50 –1,070 J). The cardiac rhythm immediately after anaesthesia, at the point of discharge later that day, and at first clinical follow-up after the DCCV for all patients is shown in table 1.
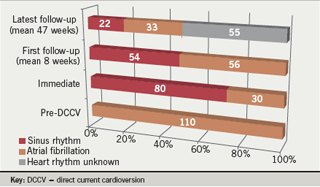
The time to the first post-DCCV clinic follow-up was a mean of eight weeks (median six weeks, range 3–36 weeks). For 55 (50%) of the patients who underwent DCCV, a further, later contact with the hospital allowed a determination of their rhythm. All 12 with a failed cardioversion were still in AF at this long-term follow-up visit. Of the 43 who had been successfully cardioverted to SR, just 22 remained in SR. Thus, of the original 110 patients undergoing DCCV, only 22 (20%) were known to be in SR at a mean of 47 weeks (range 6–160 weeks) after the DCCV (figure 1).
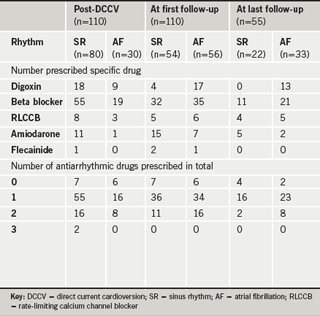
Table 2 shows the use of anti-arrhythmic drugs (both for the individual drugs and the total number of anti-arrhythmic drugs being used) in each of the 110 cardioverted patients at the time of cardioversion and at their first hospital follow-up after the procedure, and includes data for the 55 patients who had later contact with the hospital sometime after their first follow-up consultation. Of the cardioverted patients still in AF at first follow-up, 11 of the 17 patients receiving digoxin were not receiving any other anti-arrhythmic drug. At longer-term follow-up, seven of the 13 patients receiving digoxin were on no other anti-arrhythmic medication for their permanent AF.
Discussion
Studies have shown that the long-term success rates of maintaining sinus rhythm in AF patients undergoing cardioversion are not high, with between 42% and 53% still in SR at one year and 27% in SR after four years, respectively.5,6 These facts, together with the trials that show little improvement in quality of life for those undergoing a ‘rhythm control’ strategy as opposed to a rate control strategy,2,3 may have been responsible for fewer patients being referred for DCCV as a treatment of AF. We certainly noticed a reduction in referrals to our service during 2006 and 2007, causing us to respond by reducing the DCCV lists to bi-monthly, though there has been an upsurge in referrals during 2008, allowing us to restore monthly DCCV lists.
Our initial success rate of 73% immediately after the procedure is in accord with other published figures of a 70–90% immediate success rate at restoring SR, but it is said that ‘the majority’ of patients revert to AF within a year.7 Our study demonstrated that only 21% of those successfully cardioverted were definitely found to be in SR at a mean of 47 weeks post-procedure, a similar outcome to other published figures. However, our figure may have underestimated the long-term success of cardioversion, as not all successfully cardioverted patients had had a further hospital check up after their initial follow-up visit yet may still be in SR.
It remains unclear as to whether the numbers maintained in SR can be safely and effectively increased by the use of anti-arrhythmic drugs before and after cardioversion. A Cochrane Database report of 45 good quality studies testing various anti-arrhythmic drugs in over 12,000 AF patients has been published.8 Though these studies showed several drugs were effective at preventing recurrence of AF, all of them increased adverse effects and, thus, it is recommended that we await more studies before reaching a conclusion about the routine addition of anti-arrhythmic treatment either before or after DCCV. Of the cardioverted patients in the present study, most were taking at least one anti-arrhythmic drug at the time of the procedure, including a beta blocker and/or rate-limiting calcium channel blocker in 77%, consistent with NICE recommendations on the treatment of AF.4 The use of anti-arrhythmic medication was high, even at longer-term follow-up, with 82% of the patients in SR and 94% of those remaining in AF taking at least one such drug. Although it was not always possible to determine the true reason for the medication, it may be that the drugs were for other cardiovascular indications, such as hypertension or cardiac secondary prophylaxis, at least for those in SR, although five of the longer-term SR patients were still on amiodarone, suggesting an attempt to keep them in SR.
It is interesting to see that digoxin was being used in a quarter of all the patients before DCCV, and in over half of those patients, it was being used as sole anti-arrhythmic. Digoxin was still being taken by 30% of those remaining in AF at first follow-up and by 39% of those in AF at longer follow-up. Also, it was the only anti-arrhythmic drug being prescribed for 65% AF patients at first follow-up and 54% AF patients at longer follow-up. This is despite the NICE guidance suggesting that digoxin not be used as first-line treatment for AF, but be added to first-line treatment only if control of the rate cannot be maintained by beta blockers or rate-limiting calcium channel blockers.
Conclusion
Our results demonstrate a high initial success rate for the procedure of elective DCCV in patients with AF, but over the subsequent weeks and months, we found that as few as a fifth of these patients may remain in SR. The question, thus, remains whether this is a procedure that is worth undertaking in the majority of AF patients.
Acknowledgments
I am most grateful to Christina Rollin, Sarah Wright and Caroline Beresford of the Clinical Audit Department for the speedy way in which they tracked down and provided the case notes for review.
Conflict of interest
None declared.
Editors’ note
An editorial ‘Routine cardioversion for patients with atrial fibrillation’ by David A Fitzmaurice can be found on pages 55–6.
Key messages
- Direct current cardioversion is a treatment option for persistent atrial fibrillation
- There is a high immediate success rate at restoring sinus rhythm
- However, a considerable proportion of patients relapse back into atrial fibrillation in the months after the cardioversion
- Consideration should be given to whether a strategy of ‘rate control’ rather than ‘rhythm control’ is more likely to have a sustained benefit for the patient in atrial fibrillation
References
- Walsh J, Sandler DA, Elliot C, Challands A. The introduction of a new service for direct current cardioversion (DCCV) for atrial fibrillation in a district general hospital. Br J Cardiol 2003;10:367–9.
- The Atrial Fibrillation Follow-up Investigation of Rhythm Management (AFFIRM) Investigators. A comparison of rate control and rhythm control in patients with atrial fibrillation. N Engl J Med 2002;347:1825–33.
- Hagens VE, Van Gelder IC, Crijns HJ. Rate control versus electrical cardioversion of persistent atrial fibrillation (RACE) study group. Card Electrophysiol Rev 2003;7:118–21.
- National Institute for Health and Clinical Excellence. Atrial fibrillation. NICE clinical guidelines 36. London: NICE, June 2006. Available from: http://www.nice.org.uk/nicemedia/pdf/CG036niceguideline.pdf
- Van Gelder IC, Crijns HJ, Tieleman RG et al. Chronic atrial fibrillation: success of serial cardioversion therapy and safety of oral anticoagulation. Arch Intern Med 1996;156:2585–92.
- Bertaglia E, D’Este D, Zerbo F et al. Success of serial external electrical cardioversion of persistent atrial fibrillation in maintaining sinus rhythm: a randomized study. Eur Heart J 2002;23:1522–8.
- Waktare JE, Camm AJ. Atrial fibrillation begets trouble. Heart 1997;77:393–4.
- Lafuente-Lafuente C, Mouly S, Longas-Tejero MA, Bergmann JF. Antiarrhythmics for maintaining sinus rhythm after cardioversion of atrial fibrillation. Cochrane Database Syst Rev 2007;(4):CD005049. DOI: 10.1002/14651858.CD005049.pub2
