An observational study was conducted on patients with pre-existing coronary heart disease who were re-admitted to an acute district general hospital with a further acute coronary event. Their demographics, admission drug therapies and cardiovascular risk factor parameters were recorded and analysed. Of the 100 patients admitted over a nine-month period, more than a quarter of them were taking suboptimal secondary prevention drug therapies. Furthermore, a proportion of patients were not achieving adequate cholesterol, blood pressure and heart rate targets, which, in turn, may be a major contributory factor for their re-presentation to hospital.
Introduction
Over 90 people die from myocardial infarction (MI) every day in the UK.1 Cardiac rehabilitation, which incorporates cardioprotective drug therapies as one of its core components,2 has been shown to be associated with a reduction in recurrent MI.3 The National Service Framework (NSF) for Coronary Heart Disease (CHD) set out a strategy in 2000 to change CHD services over the next 10 years.4 Improvements have been delivered in most standards of cardiac services but uptake and adherence to cardiac rehabilitation programmes following MI, coronary angioplasty or coronary artery bypass (CABG) surgery are still below the 85% target set for each of these diagnostic groups.5
Studies have demonstrated prognostic benefits from effective management of cardiovascular (CV) risk factors in patients with established CHD. Clinical guidelines by the National Institute for Health and Clinical Excellence (NICE),6 American Heart Association (AHA)/American College of Cardiology (ACC)7,8 and European Society of Cardiology (ESC)9 emphasise risk factor modification through optimisation of drug therapies for secondary prevention following MI. All include treatment targets for blood pressure and lipid control, in addition to recommendations on diet, smoking cessation, physical activities and weight management. Failure of adherence to these guidelines could potentially increase the risk of recurrent coronary events and hospital re-admission rates. Although there is no guideline recommendation on post-MI heart rate target, elevated heart rate has been shown to be associated with increased risk of further cardiac events in those with established cardiovascular disease (CVD),10,11 and recent trials have shown benefits in patients with resting heart rate of <70 beats per minute and reduced left ventricular function.12,13
Aim
To determine the extent of secondary prevention drug therapies and effects on CV risk factor targets in patients with pre-existing CHD who presented with a further acute coronary event in a busy London district general hospital. To our knowledge, this is the first study that has explored pharmacological secondary prevention and CV risk targets in such a specific cohort of patients in the UK.
Methods
In this single-centre, prospective, observational study, the admission details, drug therapies and CV risk factors (cholesterol level, blood pressure and heart rate) were recorded on consecutive patients admitted during unselected acute medical takes with an acute coronary syndrome (ACS) (defined as unstable angina or non ST-elevation myocardial infarction [NSTEMI] or ST-elevation myocardial infarction [STEMI]) over a nine-month period between January 2011 and October 2011. Patients with an established diagnosis of CHD were identified from this group and included into the study. This included patients who had a previous NSTEMI or STEMI, and patients who had undergone coronary revascularisation (either percutaneous coronary intervention [PCI] or CABG). Additionally, patients with sole coronary artery disease (CAD) as determined on a previous coronary angiogram were also included. Any reasons for suboptimal drug therapy, such as allergy, adverse reaction, contraindication and patient’s refusal, were also noted but still included in this study to avoid selection bias.
Results
A total of 100 patients (61% male, mean age 65.1 ± 1.9 years; 39% female, mean age 65.5 ± 2.2 years) were included. Of these, n=38 (38%) were non-smokers, n=26 (26%) current smokers and n=36 (36%) ex-smokers.
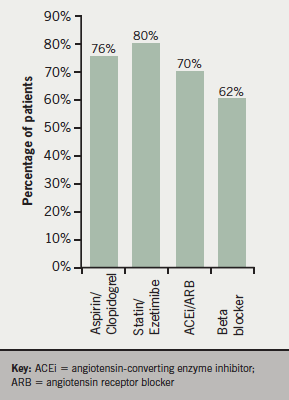
Of those medications used for secondary prevention, 47 (47%) patients were on aspirin alone, seven (7%) on clopidogrel alone and 22 (22%) on dual antiplatelet therapy. Seven (7%) patients were on lone moderate-intensity warfarin therapy. Regarding lipid-regulating medication, 76 (76%) were receiving a statin, three (3%) receiving ezetimibe and one (1%) was on two anti-lipid drugs. For blood pressure control, 70 (70%) were on an angiotensin-converting enzyme inhibitor (ACEi) or angiotensin receptor blocker (ARB), and 62 (62%) were on a beta blocker; with seven (7%) taking diltiazem as the alternative to beta blocker due to intolerance or contraindications (figure 1).
Total cholesterol was <5 mmol/L (audit target level) in 82% and <4 mmol/L in 55% of patients; 49% of patients had low-density lipoprotein (LDL)-cholesterol <2 mmol/L. The mean total cholesterol level was 3.98 mmol/L (95% confidence interval [CI] 3.7–4.3 mmol/L) and mean LDL cholesterol was 2.24 mmol/L (95% CI 2.0–2.5 mmol/L).
Overall, 34% of patients had systolic blood pressure (BP) <130 mmHg and 54% had diastolic BP <80 mmHg. The mean presenting systolic BP was 139.1 ± 26.6 mmHg, and mean presenting diastolic BP was 78.5 ± 15.9 mmHg.
Resting heart rate was <70 bpm in 43% of patients and 14% of patients had a resting heart rate of <60 bpm.
Discussion
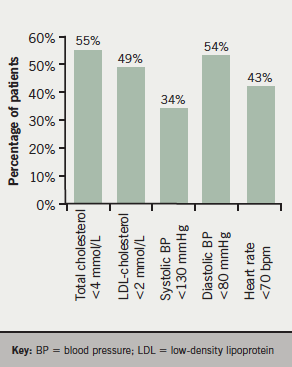
We detected a significant proportion of CHD patients were on suboptimal secondary prevention drug therapies at the point of their re-admission to hospital with an ACS. In our cohort of 100 patients, 24% were not on antiplatelet therapy (although 7% were on moderate-intensity warfarin therapy), 20% were not receiving any lipid-regulating drug, and 30% were not on treatment with either an ACEi or ARB. While 38% of patients were not on a beta blocker, 7% were taking a suitable alternative treatment in the form of a non-dihydropyridine calcium channel blocker. Treatment targets for total cholesterol level, systolic BP and heart rate were reached in only 55%, 34% and 43% of patients, respectively (figure 2).
Possible reasons for the suboptimal management of secondary prevention drug therapy lie in the ineffective communication between the discharging hospital team, primary care and patient. Insufficient or imprecise information conveyed to patients’ general practitioners (GPs) by hospital doctors following hospital discharge may mean repeat prescriptions are not correctly provided for patients, or discharge medication not titrated upwards to evidence-based dosage in order to achieve BP, lipid and heart rate goals following hospital discharge. Inadequate explanation to patients and/or poor understanding on the patient’s behalf regarding the indications and importance of his/her prescribed drugs increases non-compliance to medications. Lack of appropriate follow-up in post-MI/CHD clinic or by a GP may compound the problem further.
Hence, better strategies are required to ensure that management of secondary prevention in CHD patients is improved. Attaining good communication channels between the hospital and GPs deserves more attention. It is important to provide GPs with clearer and more precise instructions on hospital discharge documents in regards to patients’ drug therapies, their indications, doses and treatment duration, if any. Second-line drugs should be recommended if the patient has to discontinue first-line therapy due to intolerance or side effects.
Reiterating the key points on CV treatment goals on patients’ discharge documents, or dissemination of CV prevention guidelines/practices to the GPs, may be useful. Continued and close monitoring of lipids, BP and heart rate in CHD patients should be encouraged – both in GPs and the patients. For the patients, clear explanation by the discharging physician or pharmacist, including providing written instructions to patients before discharge, is central to good drug compliance.
Early referral to, and engagement of CHD patients in, a comprehensive cardiac rehabilitation programme will not only provide them with appropriate lifestyle risk-factor management, such as smoking cessation, increased physical activities and weight control, but may also provide an important channel to ensure necessary drug treatments are not overlooked and strengthen patients’ adherence to medications.
We acknowledge that only a relatively small cohort of patients from a single district general hospital were assessed in our study and results might be influenced by local factors, such as accessibility to cardiac rehabilitation services and the effectiveness of communication between our doctors and local GPs. However, the findings do support other studies highlighting that secondary prevention and/or risk factor modification in CHD patients is often not optimally achieved in clinical practice.14-17 Our study does have potential implications in the current National Health Service (NHS) climate. It emphasises the importance of needing to focus on evidence-based interventions, patient communication/compliance and close liaison among health professionals. Our results reinforce the idea of concentrating on pathways that can potentially avoid hospital re-admissions and provide cost-savings, priorities related to primary-care commissioning strategies and effective inpatient bed management. Perhaps, replicating this study in other centres may provide a feel for the national picture.
Conflict of interest
None declared.
Key messages
- NICE (National Institute for Health and Clinical Excellence), AHA/ACC (American Heart Association/American College of Cardiology) and ESC (European Society of Cardiology) clinical guidelines recommend risk factor modification by optimisation of drug therapies for secondary prevention in patients who have suffered a myocardial infarction
- We found that more than a quarter of patients with pre-existing coronary heart disease who were re-admitted to hospital with an acute coronary syndrome (ACS) were on suboptimal secondary prevention drug therapies
- Attainment of targets for cholesterol level, blood pressure and heart rate was low at the point of their re-admission
- Better strategies are required to ensure that patients with known coronary heart disease receive adequate drug therapies for secondary prevention
References
- Charles Rivers Associates. The burden of acute coronary syndromes in the UK. London: CRA, 2010. Available from: http://www.crai.com/Europe/ConsultingExpertise/listingdetails.aspx?id=13703&tID=1454&subtID=0&tertID=0&fID=34&SectionTitle=Life+Sciences
- British Association for Cardiovascular Prevention and Rehabilitation. The BACPR standards and core components for cardiovascular disease prevention and rehabilitation 2012 (2nd Ed.). London: BACPR, March 2012. Available from: http://www.bacpr.com/resources/15E_BACPR_Standards_FINAL.pdf
- Clark AM, Hartling L, Vandermeer B, McAlister F. Meta-analysis: secondary prevention programs for patients with coronary artery disease. Ann Intern Med 2005;143:659–72.
- Department of Health. Coronary Heart Disease: National Service Framework for Coronary Heart Disease – Modern Standards and Service Models. London: DoH, March 2000.
- British Heart Foundation. The National Audit of Cardiac Rehabilitation – Annual Statistical Report 2010. London: BHF, 2010.
- National Institute for Health and Clinical Excellence. MI: secondary prevention. NICE clinical guideline 48. Developed by the National Collaborating Centre for Primary Care. London: NICE, May 2007.
- Smith SC Jr, Allen J, Blair SN et al.; AHA/ACC; National Heart, Lung, and Blood Institute. AHA/ACC guidelines for secondary prevention for patients with coronary and other atherosclerotic vascular disease: 2006 update: endorsed by the National Heart, Lung, and Blood Institute. Circulation 2006;113:2363–72. http://dx.doi.org/10.1161/CIRCULATIONAHA.106.174516
- Sidney CS Jr, Benjamin EJ, Bonow RO et al. AHA/ACCF secondary prevention and risk reduction therapy for patients with coronary and other atherosclerotic vascular disease: 2011 update. Circulation 2011;124:2458–73. http://dx.doi.org/10.1161/CIR.0b013e318235eb4d
- The Fifth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice. European guidelines on cardiovascular disease prevention in clinical practice. Eur Heart J 2012;33:1635–701. http://dx.doi.org/10.1093/eurheartj/ehs092
- Fox K, Ford I, Steg PG, Tendera M, Robertson M, Ferrari R. Heart rate as a prognostic risk factor in patients with coronary artery disease and left ventricular systolic dysfunction (BEAUTIFUL): a subgroup analysis of a randomised controlled trial. Lancet 2008;372:817–21. http://dx.doi.org/10.1016/S0140-6736(08)61171-X
- Diaz A, Bourassa MG, Guertin MC, Tardif JC. Long-term prognosis value of resting heart rate in patients with suspected or proven coronary artery disease. Eur Heart J 2005;26:967–74. http://dx.doi.org/10.1093/eurheartj/ehi190
- Fox K, Ford I, Steg PG, Tendera M, Ferrari R. Ivabradine for patients with stable coronary artery disease and left ventricular systolic dysfunction (BEAUTIFUL): a randomised double-blind, placebo-controlled trial. Lancet 2008;372:807–16. http://dx.doi.org/10.1016/S0140-6736(08)61170-8
- Swedberg K, Komajda M, Bohm M et al. Ivabradine and outcomes in chronic heart failure (SHIFT): a randomised placebo-controlled study. Lancet 2010;376:875–85. http://dx.doi.org/10.1016/S0140-6736(10)61198-1
- Turley AJ, Roberts AP, Morley R, Thornley AR, Owens WA, de Belder MA. Secondary prevention following coronary artery bypass grafting has improved but remains sub-optimal: the need for targeted follow-up. Interact Cardiovasc Thorac Surg 2008;7:231–4.
- Kotseva K, Wood D, De Backer G, De Bacquer D, Pyörälä K, Keil U; EUROASPIRE Study Group. EUROASPIRE III: a survey on the lifestyle, risk factors and use of cardioprotective drug therapies in coronary patients from 22 European countries. Eur J Cardiovasc Prev Rehabil 2009;16:121–37. http://dx.doi.org/10.1097/HJR.0b013e3283294b1d
- Shakur R, Sathasivam S, Yu C et al. Optimizing secondary prevention: statin prescribing across East and West London in accordance with NICE guidelines. J R Soc Med 2011;2:63.
- Yusuf S, Islam S, Chow CK et al.; Prospective Urban Rural Epidemiology (PURE) Study Investigators. Use of secondary prevention drugs for cardiovascular disease in the community in high-income, middle-income, and low-income countries (the PURE Study): a prospective epidemiological survey. Lancet 2011;378:1231–43. http://dx.doi.org/10.1016/S0140-6736(11)61215-4
