Three abstracts of outstanding quality were presented for the Young Investigators’ Award at the British Society of Heart Failure’s 15th Annual Autumn Meeting.
Multipolar left ventricular pacing to optimise acute haemodynamic response to cardiac resynchronisation therapy
SY Ahsan (presenting author), B Sabberwal, C Hayward, P Lambiase, M Thomas, GG Babu, S Aggarwal, MD Lowe, AWC Chow
The Heart Hospital, Institute of Cardiovascular Science, University College Hospitals NHS Foundation Trust, London
Purpose: Cardiac resynchronisation therapy (CRT) reduces morbidity and mortality in a sub-group of patients with heart failure, though up to 30% of patients have no benefit. CRT patients are heterogeneous and an individualised approach to CRT may be needed to increase response rate. We evaluated the impact of different left ventricular (LV) pacing sites and configurations on the acute haemodynamic response (AHR) to CRT.
Methods: 28 patients (male 75%, female 25%, age 66.4±11.5 years, dilated cardiomyopathy 50%, ischaemic heart disease 50%, NYHA class 2.7±0.4, left ventricular ejection fraction 24.6±6.5% and QRS 149±31 ms) referred for CRT underwent an acute study to analyse the AHR with CRT, using single- and multi-site pacing from within a coronary sinus (CS) branch. Electrophysiology catheters were positioned in the right atrium and ventricle. An octapolar catheter was introduced to one or more branches of the CS.
15 pre-determined biventricular pacing configurations stimulating single and multiple sites within each CS branch were analysed in all patients. AV intervals were optimised invasively in all patients. For each pacing configuration, a pressure-sensor tipped guidewire was passed to the LV cavity to measure dP/dt max. Acute trans-thoracic echo data (aortic velocity time integral and tissue Doppler measurements to assess dysynchrony) were acquired simultaneously.
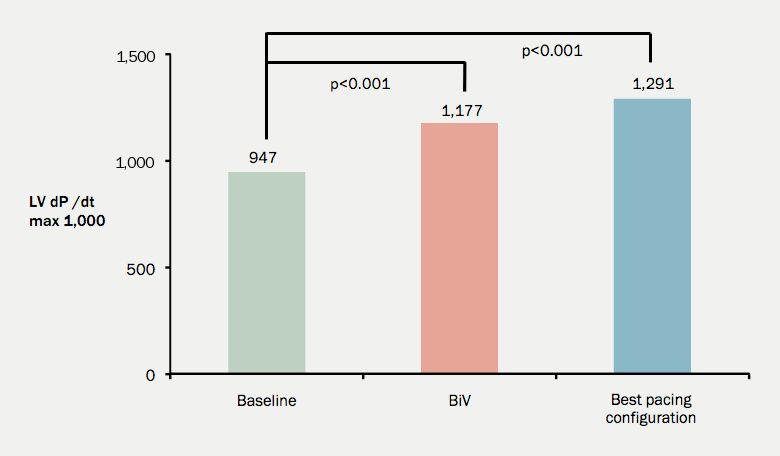
Results: Major intra- and inter-individual variations in the AHR were noted. The mean dp/dt max during sinus rhythm was 947±221. When using a conventional biventricular configuration, this increased to 1177±306 (an increase of 24.3%; p<0.001). Selecting the best LV pacing configuration for each patient (either single or multi-site) led to a further increase in dP/dt max to 1291±333 (figure 1). This represents an increase in dP/dt max of 9.9% compared to conventional biventricular pacing (p<0.001) and an absolute increase of 36.3% from baseline (p<0.001). Compared to standard biventricular pacing, significant improvements in dP/dt max were also observed using either the best single LV site (6.8%; p<0.002) or LV multi-site (5.8%; p=0.005) configurations.
Conclusions: Significant improvements in the AHR to CRT, over and above that observed with conventional biventricular pacing, can be achieved by selecting the best single or multisite LV pacing configuration tailored individually to each patient.
Microvolt T-wave alternans testing has no prognostic value in patients recently hospitalised with decompensated heart failure
Colette E Jackson (presenting author),1* Rachel C Myles,1 Ioannis K Tsorlalis,1 Jonathan R Dalzell,1J Paul Rocchiccioli,1 John R Rodgers,2 Richard J Spooner,3 Nicola Greenlaw,4 Ian Ford,4 Roy S Gardner,5 Stuart M Cobbe,1 Mark C Petrie,5 John JV McMurray1
1British Heart Foundation Cardiovascular Research Centre, University of Glasgow 2Department of Cardiology, Glasgow Royal Infirmary
3Department of Biochemistry, Gartnavel General Hospital
4Robertson Centre for Biostatistics, University of Glasgow
5Scottish National Advanced Heart Failure Service, Golden Jubilee National Hospital, Glasgow
Purpose: Ventricular arrhythmias contribute to the high risk of sudden cardiac death in heart failure (HF). Microvolt T-wave alternans (MTWA) testing identifies beat-to-beat fluctuations in T-wave morphology, which have been linked, mechanistically, to ventricular arrhythmias. Observational studies in highly selected populations have suggested that MTWA testing may identify individuals likely to benefit from a primary prevention implantable cardioverter-defibrillator. However, clinical studies in HF have been limited and produced conflicting results. The aims of this study were to determine the prevalence and incremental prognostic value of MTWA testing in an unselected cohort of patients recently hospitalised with HF.
Methods: Consecutive admissions with confirmed HF (typical clinical findings and BNP >100 pg/ml) were recruited in three hospitals from 1/12/06–12/01/09. Survivors were invited to attend one month post-discharge for MTWA testing and followed-up until death or censoring at 31st August 2011.
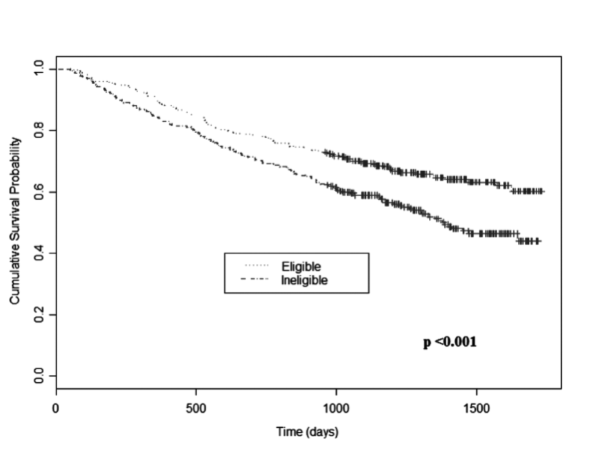
Results: Some 648 of 1003 enrolled patients returned for MTWA testing (58% male, mean age 71 years). 49% were ineligible due to atrial fibrillation, pacemaker-dependency or inability to exercise. Of the 330 MTWA test results, 30% were positive, 24% negative and 46% indeterminate. Overall, 268 deaths occurred during a median follow-up of 3.1 [IQR 1.9–3.9] years. 48% of ineligible patients died versus 35% of eligible patients (p<0.001, see figure 2). 27%, 35% and 40% of patients with positive, negative and indeterminate tests, respectively, died (p=0.12). Even when analysed as non-negative (positive/indeterminate) versus negative, there was still no between-group difference in mortality (p=0.95). MTWA results categorised as positive, negative or indeterminate showed no incremental prognostic value in a multivariable mortality model, which included B-type natriuretic peptide (BNP). Paradoxically, when compared in a binary fashion with a non-negative result, a negative test was an independent predictor of death, as was ineligibility for MTWA testing.
Conclusion: MTWA testing was not widely applicable in typical patients with HF and failed to predict mortality. Established clinical variables for prognostication in HF, including BNP, identified the patients at greatest risk in this study. At present MTWA cannot be endorsed as a risk stratification tool in HF.
Does chronic kidney disease adversely impact on secondary prevention in the era of primary percutaneous coronary intervention (PPCI)?
D Zachariah (presenting author),1* R Brown,2 P Callan,2 P Kanagala,3 R Hendra,3 A Clark,2 I Squire,3 C Lang,4 PR Kalra1
1Portsmouth Hospitals NHS Trust
2University of Hull, Department of Academic Cardiology
3University Hospitals of Leicester NHS Trust
4Department of Cardiology Ninewells Hospital, Dundee
Purpose: Chronic kidney disease (CKD) is associated with development of chronic heart failure (CHF) or death post-myocardial infarction (MI). Previous studies have shown that patients with CKD receive suboptimal secondary prevention following MI and have less frequently been considered for revascularisation. Reasons may include the perception that such patients are too high risk for procedures and/or unlikely to benefit from interventions.
Optimisation of drugs post-MI is essential to minimise progression to CHF. The current standard treatment for ST-elevation MI (STEMI) is primary percutaneous coronary intervention (PPCI), irrespective of renal function. We evaluated the impact of CKD on secondary prevention following PPCI in a contemporary unselected cohort.
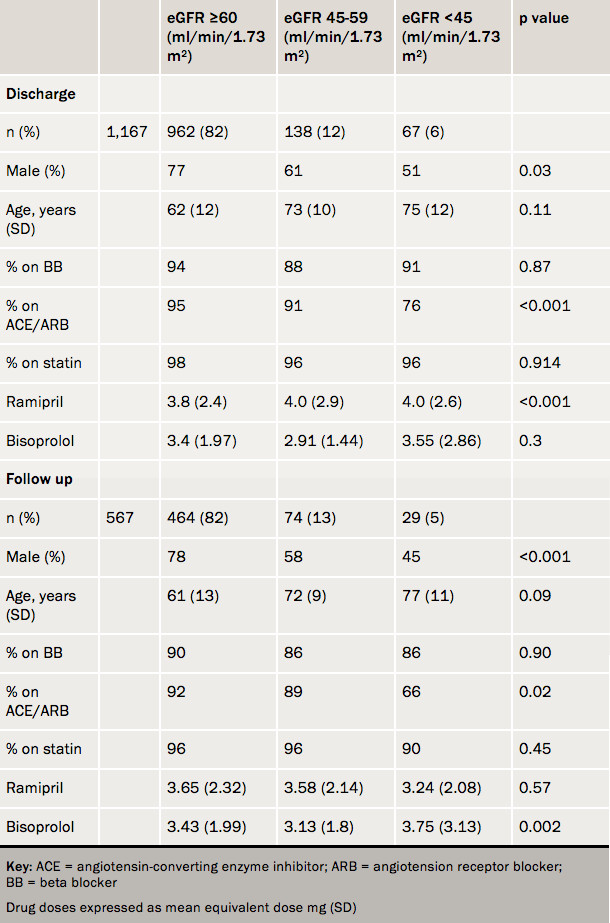
Methods: Retrospective study of 1,159 consecutive patients from five UK centres receiving PPCI for STEMI. The population was divided according to estimated glomerular filtration rate (eGFR, ml/min/1.73m2): eGFR ≥60, eGFR 45–59 and eGFR <45. Beta blocker, angiotensin-converting enzyme (ACE) inhibitor and statin use was evaluated at discharge and early follow-up (n=567). Drug dosages were compared between groups for beta blockers (expressed as bisoprolol equivalent) and ACE inhibitors (ramipril equivalent).
Results: See table 1. 18% had eGFR <60 ml/min/1.73 m2. Declining renal function was associated with age, gender and lower haemoglobin. Overall, at discharge, in the eGFR <60 ml/min/1.73 m2 cohort, 89.5% were on beta-blockers, 83.5% on ACE inhibitors and 96% on statins. By six weeks these were 86%, 77.5% and 93%, respectively. Advanced CKD (<45 ml/min/1.73 m2) was associated with lower use of ACE inhibitors at both discharge and follow-up (including a reduction in dose at 6 weeks).
Conclusions: Compared to historic data secondary prevention is very good post PPCI irrespective of CKD stage. However, the use of ACE inhibitors remains lower than beta blockers and statins for those with worst renal function. Whilst a small drop off in therapy is seen at early follow-up, the overall impression is that secondary prevention is relatively well tolerated. Immediate PPCI, irrespective of renal function, may reduce previous bias resulting from concerns regarding worsening renal function and potential complications of coronary intervention. Further evaluations are warranted to see if this translates into reduced risk of CHF development.
Online extra
This report is only available online.
