The 2010 UK National Institute of Health and Care Excellence (NICE) guidelines for assessing patients with ‘chest pain of recent onset’ recommend coronary artery calcium scoring (CACS) to assess patients with a low risk of coronary artery disease (CAD) according to defined criteria. This study aims to evaluate the implementation of these guidelines in an area with a prevalence of CAD higher than the national average.
Consecutive patients with recent onset stable chest pain were assessed by cardiologists in outpatient clinics at University Hospital Aintree, Liverpool, between January and December 2011. A total of 186 patients with a low risk of CAD underwent CACS and follow-on computed tomography coronary angiography (CTCA) if CACS <400.
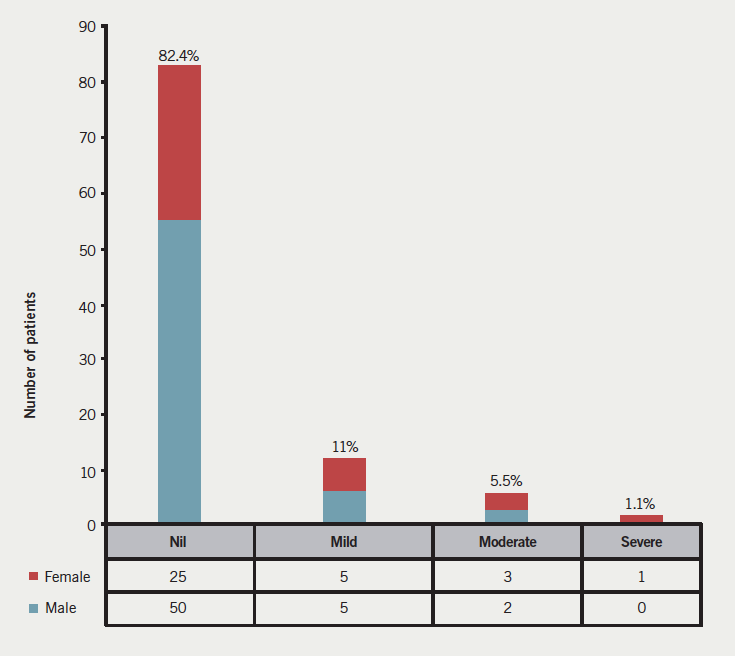
A CACS of zero was found in 94 patients and three of these were excluded due to motion artefacts. Of the remaining 91 patients, 75 (82.4%) had no visible atheroma, 10 (11%) had minor plaque, five (5.5%) had moderate disease and one (1.1%) had apparent severe disease, which was shown to be a false-positive result on subsequent invasive coronary angiography.
This study shows a negative predictive value for severe disease of 99% for a CACS of 0 in stable patients with a low pre-test probability of CAD. This supports the NICE guidelines, with CACS being the investigation of choice in the UK to rule out significant CAD in selected patient populations. The fact that almost half of all the patients referred for CTCA had a CACS of zero makes this a good quick rule-out tool and, hence, avoids the need for follow-on CTCA.
Introduction
The North West Health Authority has the third highest prevalence of coronary artery disease (CAD) in England at 4.0%.1 The average for the prevalence of CAD in England, as of 2010, is 3.4%, and this makes the prevalence of CAD in the northwest region higher than the national average.1 The investigation of new-onset stable chest pain by a non-invasive and safe test in low-risk symptomatic individuals is highly relevant. To this effect, the recent National Institute for Health and Care Excellence (NICE) guidelines2 have highlighted a need for calcium scoring as an alternative to exercise treadmill testing to rule out CAD in stable, symptomatic low-risk individuals. Raggi et al.3 showed a substantial cost benefit of the use of coronary artery calcium scoring (CACS) over the use of exercise testing in this very population. In the light of the new UK guidelines, exercise treadmill testing has become obsolete in diagnosing CAD and has been removed from the latest iteration of the guidelines.2 Indeed, Lamont et al.4 did show that coronary calcium had lower false-positive results than the exercise treadmill test as compared to the gold-standard invasive angiography.
The NICE guidelines use table 12,5 to attribute a risk profile to patients presenting with chest pain, which will then guide the choice of investigation options in patients with new-onset and stable chest pain syndromes.
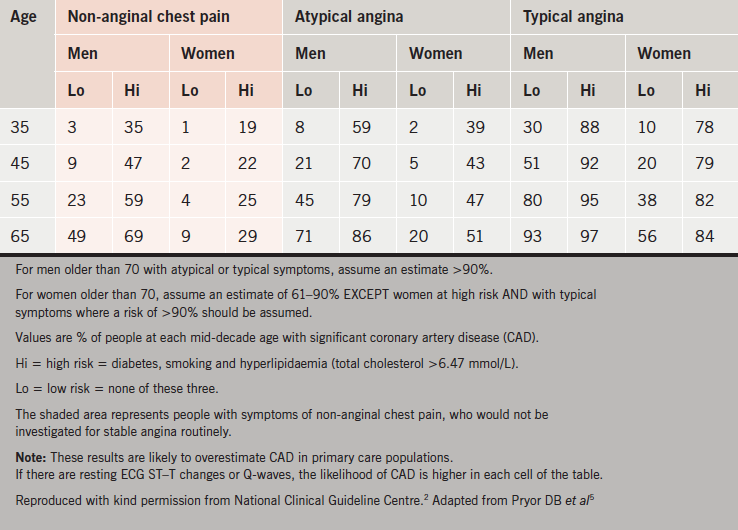
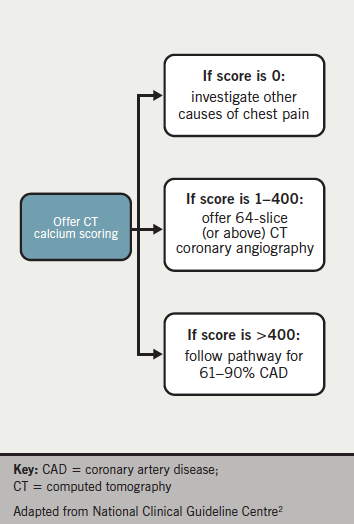
The table uses the character and typicality of the pain, together with age, sex and risk factors, to attribute a pre-test probability of CAD. If the pre-test likelihood of having CAD is 10–29%, then the flowchart (figure 12) is used and a CACS is performed.
Using CACS to screen low-risk symptomatic individuals before proceeding to computed tomography coronary angiography (CTCA) has numerous advantages. If the CACS is zero, as per the above flowchart, then there would be no need to proceed to CTCA. Therefore, the risk of stochastic and deterministic injury is reduced due to lower radiation exposure, as compared with CTCA and invasive angiography.6 With new algorithms, better detectors and improved software, the radiation exposure can be kept as low as 1.0 mSv.7 Additionally, there is no use of iodinated contrast in calcium scoring and, hence, no risk of adverse reactions to contrast agents.8 Another major advantage of CACS is that it takes half of the time to perform a CACS as compared with a CTCA.
Methods
This prospective observational registry study included consecutive patients who were referred to the cardiology outpatient department of Aintree University Hospital, Liverpool, by primary care physicians for assessment of non-acute, stable chest pain syndromes between January and December 2011. They were risk stratified in clinic using the NICE guidelines, as above, and suitability for CACS and CTCA was assessed. The exclusion criteria were known allergy to iodinated contrast media or history of contrast-induced nephropathy, history of multiple myeloma or previous organ transplantation, calculated creatinine clearance of <60 ml/min, atrial fibrillation or uncontrolled tachyarrhythmia, second- or third-degree atrioventricular block, evidence of New York Heart Association (NYHA) functional class III or IV heart failure, known or suspected moderate or severe aortic stenosis, known CAD, known or suspected intolerance to beta blockers, body mass index >40 kg/m2, and pregnancy.
All consecutive patients with a low probability of CAD (10–29%), and who did not have any of the exclusion criteria above, underwent a CACS followed by CTCA. This was in line with the recommendation from the British Society of Cardiovascular Imaging.9 Imaging was performed on a Toshiba Aquilion 160-slice CT scanner and analysed by a consultant cardiologist and consultant radiologist as per Society of Cardiovascular Computed Tomography guidelines.10,11 The reports were collated and analysed by calcium scores derived from the Agatston calculation.12 The different levels of stenoses, as reported on the CTCA, were split into mild, moderate and severe. Mild stenosis was defined as 1–49%, moderate stenosis as 50–69% and severe stenosis as ≥70%. Mild and moderate stenoses were termed non-obstructive, whereas severe stenosis was defined as being obstructive and, hence, significant.
Results
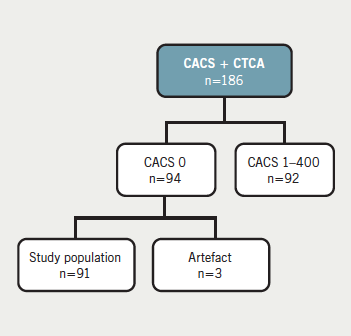
In total, 186 patients had a CACS with corresponding CTCA performed. Of these, 94 had a CACS of zero. However, three patients had significant motion artefacts on the CTCA that made interpretation difficult and were, hence, excluded from the study. The distribution of the patients with CACS with corresponding CTCA is shown in figure 2.
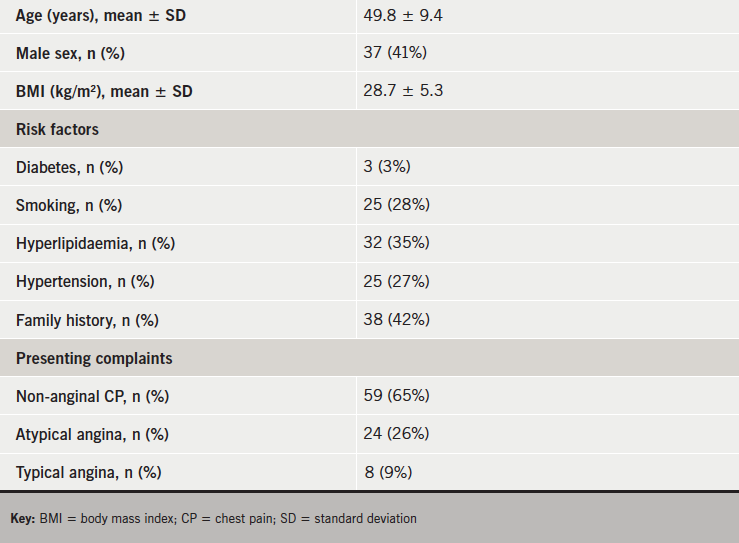
This study compares the value of a zero calcium score with findings of significant luminal narrowing on CTCA. The 91 patients included in this study had baseline characteristics as shown in table 2.
The degrees of stenoses as determined by CTCA are summarised in figure 3.
The single case of severe stenosis was reported in a 45-year-old woman with no pre-existing medical conditions who was referred to the cardiology clinic with atypical chest pain. Due to her low-risk profile, she was referred on for CACS and CTCA. Although there was an absence of calcification, the CTCA suggested a severe left main stem lesion. She proceeded to have formal invasive coronary angiography, which showed angiographically normal coronary circulation. The CTCA pictures were retrospectively reviewed, and the apparent stenosis was deemed to be a result of motion artefact.
The single severe stenosis case picked up by the CTCA would amount to a negative predictive value of 99% (95% confidence interval [CI] 94–100%) for significant stenosis in low-risk patients with a calcium score of zero. Unfortunately, sensitivity and specificity cannot be calculated from this data set as only the test negative patients, i.e. CACS zero, have been reported in this study.
Discussion
There is a sizeable body of evidence with respect to CACS and stenosis on CTCA in chest pain syndromes,13–15 and in asymptomatic patients, as a screening tool.16–18 There are, however, not much published UK data supporting the recent NICE guidelines2 for patients referred to secondary care with stable chest pain. In this observational study, CTCA was used as a measure of coronary artery stenosis in symptomatic low-risk, stable patients with a CACS of zero. It shows a negative predictive value of 99% for significant stenosis in low-risk patients with absent calcium in their coronary arteries. However, one must be cautious in interpreting such results as, although no significant stenoses were detected on either CTCA or coronary angiogram in this patient population, 16.5% did have non-calcified stenosis as measured by CTCA.
Meta-analyses have revealed that the sensitivity and specificity of CTCA to determine significant luminal narrowing compared with the gold standard of invasive angiography can be up to 97% and 90%, respectively.19,20 In a more specific context of CACS of zero, an Italian study of 279 patients quoted sensitivity, specificity, and positive and negative predictive values of CTCA versus coronary angiography as high as 100%, 95%, 76% and 100%, respectively.21 The use of CACS to determine the absence of coronary artery stenosis as compared with invasive coronary angiography has also been validated by numerous studies as highlighted by Sarwar et al.’s seminal meta-analysis.16 It shows a negative predictive value for significant CAD, as compared with invasive coronary angiography, of 93% in the pooled data of 10,335 patients. This highlights the fact that CTCA can be an alternative measure
of luminal stenosis as compared to
formal angiography.
In asymptomatic patients, an absence of coronary artery calcification confers an excellent prognosis. This patient population has been shown to have a cardiovascular event rate of as low as 0.5% over four years.16 Hence, in the USA, there is a great drive to use CACS as a prognostic tool in asymptomatic individuals.17 In the UK, however, under the National Health Service (NHS), investigations are reserved for symptomatic individuals and CACS
has found a niche in excluding significant CAD in low-risk, stable individuals that
have been referred to secondary care for further assessment.
The current position in Europe22 is that absence of calcium cannot be used to rule out coronary artery stenoses in symptomatic individuals, especially when young and with acute symptoms. However, this statement is mostly based on a study23 that identified 21 consecutive patients from a patient population of 2,300 over a period of two years. These are very small numbers in a single retrospective study and more research is required in this emerging field.
In the Coronary Evaluation Using Multidetector Spiral Computed Tomography Angiography Using 64 Detectors (CORE 64) substudy, Gottlieb et al. discuss that CACS of zero “does not exclude obstructive stenosis or the need for revascularisation among patients with high enough suspicion of coronary artery disease”.24 The CORE 64 substudy does not fit in the UK context of assessing low-risk, stable patients. The patients selected for the trial were eligible for invasive coronary angiography within a month after a clinical assessment in the acute setting.
They were, hence, at an inherently intermediate-to-high risk of adverse cardiac events, regardless of their calcium scores. Although the CORE 64 study is against associating a CACS of zero with low risk of adverse events, it did also show that in the eight patients with CACS zero and low clinical probability of CAD, no obstructive CAD was detected. Moreover, in patients with CACS zero and intermediate (n=57) to high (n=7) CAD probability, 21% and 29%, respectively, had at least one significant coronary lesion.25 These numbers are too small to draw any meaningful conclusions but they do indicate that there is more value in having a CACS of zero in low-risk patients rather than high-risk ones, even in the presence of symptoms.
From the Coronary CT Angiography Evaluation For Clinical Outcomes International Multicenter (CONFIRM) registry, a recent study26 has shown that “the absence of measurable CAC significantly reduced, but did not fully exclude, the presence of obstructive CAD on current generation CCTA”. Again, in contrast to the UK approach, this study applies to stable all-comers who were referred by physicians with chest pain syndromes without a detailed risk assessment to identify the true low-risk patients. The authors do quote that absent calcium confers negative predictive values of 96% and 99% for stenoses of ≥50% and ≥70%, respectively. In terms of prognosis, Sarwar et al.16 found a 1.8% adverse cardiovascular event rate in a pooled sample of 921 symptomatic patients with no detectable calcium on CTCA, compared with an almost 9% event rate if coronary calcium was present. This does support the argument that detection of calcification by CTCA does predict significant stenosis and adverse cardiac events.
These two studies further emphasise the importance of a careful assessment of symptoms coupled with risk profiles in a clinical setting, as is alluded to by Greenland and Bonow.27 We cannot depart from the fact that a test is only rendered useful if specialist clinical judgement and evaluation is applied to the suitability and interpretation of the test in the right framework to answer the right questions.
Study limitations
This is a small, observational, prospective study, which does not assess prognostic significance of calcium scores in a clinical setting. Long-term morbidity and mortality data are needed in this evolving area of cardiac imaging. The level of stenosis was not assessed by the gold standard, which is invasive coronary angiography, and, ultimately, CACS and CTCA are anatomical tests with no functional elements.
Conclusion
In conclusion, this study lends support to the NICE guidelines with CACS being the investigation of choice in the UK to rule out significant CAD in patients with new-onset stable chest pain. There is even potential that cardiac risk stratification can be carried out in a primary care setting using calcium scoring.28 This may avoid the need for follow-on CTCA if the calcium score is zero. Not only is this a benefit to the patient in respect of low-risk individuals being subject to lower radiation levels in CACS as compared with CTCA, but this is also advantageous to the NHS in cost reduction and more efficient use of resources. However, the significance of calcium scores of zero in this population needs further follow-up in the view of outcome and adverse effects to validate prognosis in such patients, particularly the ones with non-obstructive, non-calcified CAD.
Key messages
- Coronary artery calcium scoring (CACS) is a quick rule-out tool for low-risk populations, which has been validated in the USA and been implemented in the new National Institute for Health and Care Excellence (NICE) guidelines to be used in the UK
- In this small study, a negative predictive value of 99% was achieved within the first year of implementation of the NICE guidelines
- This study adds to the body of evidence that implementation of the guideline has been possible and feasible with promising results
Acknowledgement
The authors would like to thank Dan Lythgoe, Statistician at The University of Liverpool, for
help with statistical analysis.
Conflict of interest
None declared.
References
1. Townsend N, Wickramasinghe K, Bhatnagar P et al. Coronary heart disease statistics. A compendium of health statistics. 2012 edition. London: British Heart Foundation, 2012. Available from: http://www.bhf.org.uk/publications/view-publication.aspx?ps=1002097
2. National Clinical Guideline Centre. Chest pain of recent onset: assessment and diagnosis of recent onset chest pain or discomfort of suspected cardiac origin (CG95). London: National Clinical Guidelines Centre at the Royal College of Physicians, 2010.
3. Raggi P, Callister TQ, Cooil B, Russo DJ, Lippolis NJ, Patterson RE. Evaluation of chest pain in patients with low to intermediate pretest probability of coronary artery disease by electron beam computed tomography. Am J Cardiol 2000;85:283–8. http://dx.doi.org/10.1016/S0002-9149(99)00733-X
4. Lamont DH, Budoff MJ, Shavelle DM, Shavelle R, Brundage BH, Hagar JM. Coronary calcium scanning adds incremental value to patients with positive stress tests. Am Heart J 2002;143:861–7. http://dx.doi.org/10.1067/mhj.2002.120972
5. Pryor DB, Shaw L, McCants CB, et al. Value of the history and physical in identifying patients at increased risk for coronary artery disease. Ann Intern Med 1993;118:81–90.
6. Einstein AJ, Henzlova MJ, Rajagopalan S. Estimating risk of cancer associated with radiation exposure from 64-slice computed tomography coronary angiography. JAMA 2007;298:317–23. http://dx.doi.org/10.1001/jama.298.3.317
7. Newton TD, Mehrez H, Wong K et al. Radiation dose threshold for coronary artery calcium score with MDCT: how low can you go? Eur Radiol 2011;21:2121–9. http://dx.doi.org/10.1007/s00330-011-2159-6
8. Briguori C, Colombo A, Airoldi F et al. Nephrotoxicity of low-osmolality versus iso-osmolality contrast agents: impact of N-acetylcysteine. Kidney Int 2005;68:2250–5. http://dx.doi.org/10.1111/j.1523-1755.2005.00683.x
9. British Society of Cardiovascular Imaging. CT Coronary Angiography Service Specification from the British Society of Cardiovascular Imaging (BSCI). BSCI, 2012. Available from: http://www.bsci.org.uk/ctca-service-specification
10. Abbara S, Arbab-Zadeh A, Callister TQ et al. SCCT guidelines for performance of coronary computed tomographic angiography: a report of the Society of Cardiovascular Computed Tomography Guidelines Committee. J Cardiovasc Comput Tomogr 2009;3:190–204. http://dx.doi.org/10.1016/j.jcct.2009.03.004
11. Raff GL, Abidov A, Achenbach S et al. SCCT guidelines for the interpretation and reporting of coronary computed tomographic angiography. J Cardiovasc Comput Tomogr 2009;3:122–36. http://dx.doi.org/10.1016/j.jcct.2009.01.001
12. Agatston AS, Janowitz FWR, Hildner FJ et al. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol 1990;15:827–32. http://dx.doi.org/10.1016/0735-1097(90)90282-T
13. Budoff MJ, Dowe D, Jollis JG et al. Diagnostic performance of 64-multidetector row coronary computed tomographic angiography for evaluation of coronary artery stenosis in individuals without known coronary artery disease: results from the prospective multicenter ACCURACY trial. J Am Coll Cardiol 2008;52:1724–32. http://dx.doi.org/10.1016/j.jacc.2008.07.031
14. Hoffmann U, Bamberg F, Chae CU et al. Coronary computed tomography angiography for early triage of patients with acute chest pain: the ROMICAT trial. J Am Coll Cardiol 2009;53:1642–50. http://dx.doi.org/10.1016/j.jacc.2009.01.052
15. Greenland P, Bonow RO, Brundage BH et al. ACCF/AHA 2007 clinical expert consensus document on coronary artery calcium scoring by computed tomography in global cardiovascular risk assessment and in evaluation of patients with chest pain: a report of the American College of Cardiology. J Am Coll Cardiol 2007;49:378–402. http://dx.doi.org/10.1016/j.jacc.2006.10.001
16. Sarwar A, Shaw LJ, Shapiro MD et al. Diagnostic and prognostic value of absence of coronary artery calcification. JACC Cardiovasc Imaging 2009;2:675–88. http://dx.doi.org/10.1016/j.jcmg.2008.12.031
17. Budoff M, McClelland R. Cardiovascular events with absent or minimal coronary calcification: the Multi-Ethnic Study of Atherosclerosis (MESA). Am Heart J 2009;158:554–61. http://dx.doi.org/10.1016/j.ahj.2009.08.007
18. Greenland P, Alpert JS, Beller GA et al. 2010 ACCF/AHA guideline for assessment of cardiovascular risk in asymptomatic adults: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation 2010;122:2748–64. http://dx.doi.org/10.1161/CIR.0b013e3182051bab
19. Hamon M, Morello R, Riddell JW, Hamon M. Coronary arteries: diagnostic performance of 16- versus 64-section spiral CT compared with invasive coronary angiography – meta-analysis. Radiology 2007;245:720–31. http://dx.doi.org/10.1148/radiol.2453061899
20. Meijer AB, O YL, Geleijns J, Kroft LJM. Meta-analysis of 40- and 64-MDCT angiography for assessing coronary artery stenosis. Am J Roentgenol 2008;191:1667–75. http://dx.doi.org/10.2214/AJR.07.4022
21. Cademartiri F, Maffei E, Palumbo A et al. Diagnostic accuracy of computed tomography coronary angiography in patients with a zero calcium score. Eur Radiol 2009;20:81–7. http://dx.doi.org/10.1007/s00330-009-1529-9
22. Montalescot G, Sechtem U, Achenbach S et al. 2013 ESC guidelines on the management of stable coronary artery disease: the Task Force on the management of stable coronary artery disease of the European Society of Cardiology. Eur Heart J 2013;34:2949–3003. http://dx.doi.org/10.1093/eurheartj/eht296
23. Marwan M, Ropers D, Pflederer T et al. Clinical characteristics of patients with obstructive coronary lesions in the absence of coronary calcification: an evaluation by coronary CT angiography. Heart 2009;95:1056–60. http://dx.doi.org/10.1136/hrt.2008.153353
24. Gottlieb I, Miller J, Arbab-Zadeh A et al. The absence of coronary calcification does not exclude obstructive coronary artery disease or the need for revascularization in patients referred for conventional coronary angiography. J Am Coll Cardiol 2010;55:627–34. http://dx.doi.org/10.1016/j.jacc.2009.07.072
25. Truong QA, Kallianos KG, Cannon CP. Coronary artery disease. Calcium score of zero: not a gatekeeper to rule out coronary artery disease. Rev Cardiovasc Med 2010;11:271–3. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3083450/
26. Villines TC, Hulten EA, Shaw LJ et al. Prevalence and severity of coronary artery disease and adverse events among symptomatic patients with coronary artery calcification scores of zero undergoing coronary computed tomography angiography: results from the CONFIRM registry. J Am Coll Cardiol 2011;58:2533–40. http://dx.doi.org/10.1016/j.jacc.2011.10.851
27. Greenland P, Bonow RO. How low-risk is a coronary calcium score of zero? The importance of conditional probability. Circulation 2008;117:1627–9. http://dx.doi.org/10.1161/CIRCULATIONAHA.108.767665
28. Ashrafi R, Thwaite E, Lewis-Jones H, Wong P, Davis G. CT coronary calcium scoring: improving cardiac risk stratification. Prim Care Cardiovasc J 2012;published online. http://dx.doi.org/10.3132/pccj.2012.002
