Atrial fibrillation (AF) is a dangerous, prevalent condition whose first presentation may be ischaemic stroke. Anticoagulation dramatically reduces stroke risk if patients are first identified. While screening enhances AF detection, it is unclear whether opportunistic pulse palpation or systematic electrocardiogram (ECG) screening is superior.
Patients across 15 general practices in the Bradford and Airedale primary care trust aged over 65 years were invited for a limb-lead ECG. A total of 6,856 patients were subjected to an ECG. This study aimed to determine if screening improved AF detection and the prevalence of cardiac rhythms that may cause an irregular radial pulse.
There were 248 patients diagnosed with AF (3.6%): 153 out of 207 traceable patients were previously diagnosed, hence, screening increased AF detection by 26.1%. Further abnormalities capable of causing an irregular pulse (i.e. ectopy) were highly prevalent at 18.3%. Overall, 99.0% of recorded ECGs were interpretable.
In conclusion, limb-lead ECG screening improved detection rates in a simple and feasible screening strategy, avoiding the need for more costly and cumbersome 12-lead ECG screening. Furthermore, the high prevalence of ectopy suggests systematic ECG screening is more specific than opportunistic screening. This study demonstrates simple ECG models may have a promising potential role in improving AF detection, particularly if asymptomatic.
Introduction
 Screening has been proposed as a method to detect patients with undiagnosed atrial fibrillation (AF) as it is a dangerous, prevalent condition that may be easily diagnosed with a simple low-cost test, an electrocardiogram (ECG), and the risk of serious sequelae such as ischaemic stroke can be effectively reduced with anticoagulation.1
Screening has been proposed as a method to detect patients with undiagnosed atrial fibrillation (AF) as it is a dangerous, prevalent condition that may be easily diagnosed with a simple low-cost test, an electrocardiogram (ECG), and the risk of serious sequelae such as ischaemic stroke can be effectively reduced with anticoagulation.1
Hence, it fulfils the Wilson Jungner criteria for a screening programme.2 The potential benefits of AF screening are far reaching, as reducing stroke prevalence has massive implications for both patients and health services in the UK, where stroke consumes approximately 5% of total National Health Service (NHS) expenditure, with an estimated 1,000 new cases of stroke per year in a typical health authority of 500,000 people.1
Previous research has demonstrated that AF screening can increase detection rates. The Screening for Atrial Fibrillation in the Elderly (SAFE) study, a large, multi-centred, randomised-controlled trial involving 50 UK primary care centres comparing routine care with screening for those aged 65 years and above, identified an additional third of AF cases with active screening.3 Although there is much support for an AF screening programme, the optimal screening strategy is less clear. In the SAFE study, opportunistic and systemic screening methods were used. Opportunistic screening comprised of pulse taking and ECG if an irregular pulse was detected, as opposed to inviting all participants for an ECG as seen in the systematic screening method. Here, it was found that opportunistic screening identified a similar number of patients with AF as the systematic strategy, but for considerably less effort. However, it is worth noting the opportunistic method led to a sizeable figure of false-positive results because AF is not the sole cause of an irregular pulse. Furthermore, it is essential that a high level of coverage is maintained with the opportunistic method in order to identify all those with AF, particularly in those who have lone or asymptomatic AF, as these patients are more likely to remain undetected.
If this is not possible, then systematic screening may be superior. This was demonstrated in a study where systematic 12-lead ECG screening identified almost three times that of opportunistic case-finding.4 Finally, ECG screening has the added advantage of detecting other serious conductive disorders, such as bundle branch and heart block.
Aim
To identify whether ECG screening using limb-lead ECG increases detection rates of AF and determine the prevalence of other cardiac abnormalities that may cause an irregular radial pulse.
Methods
From October 2009 to April 2010, a limb-lead ECG screening programme was evaluated in primary care. Letters of invitation for a standard limb-lead ECG were sent to patients across 15 general practices in the Bradford and Airedale primary care trust (PCT). Limb-lead ECG was preferred to 12-lead ECG for ease, simplicity and speed, while also maintaining the ability to provide information for AF detection. The limb-lead ECGs were performed using an ECG machine with four limb leads applied to both arms and both legs. Invitation letters included a barcode containing basic demographic data, such as NHS number and NHS Practice ID, enabling patient details to be entered using a barcode reader attached to a networked ECG machine. This recorded a 10-second limb-lead ECG at a sampling frequency of 1,000 Hz with the patient sitting in a chair with their legs supported, after electrodes were applied to ankles and wrists. Each ECG was analysed centrally by a cardiac physiologist. Measurements included PR and QT intervals, and P-wave and QRS duration. Their interpretations consisted of commenting on rhythm, degree of atrioventricular (AV) block and QRS duration. This report was uploaded on a web-based system that was accessible in primary care. A consultant cardiologist audited the ECGs that had been interpreted by the cardiac physiologists, in order to maintain quality control.
We used the data to compare the prevalence of AF using limb-lead ECG screening with the prevalence of
existing AF.
Results
The study was undertaken in 15 practices covering a total of 146,495 patients. Patients aged over 65 years old were invited for ECG, resulting in 22,360 invites and producing 6,856 unique limb-lead ECGs. Hence, the take up rate was 30.7% (6,856/22,360). Overall, 248 patients from 6,856 were diagnosed with AF using limb-lead ECG, a prevalence of 3.6% (figure 1).
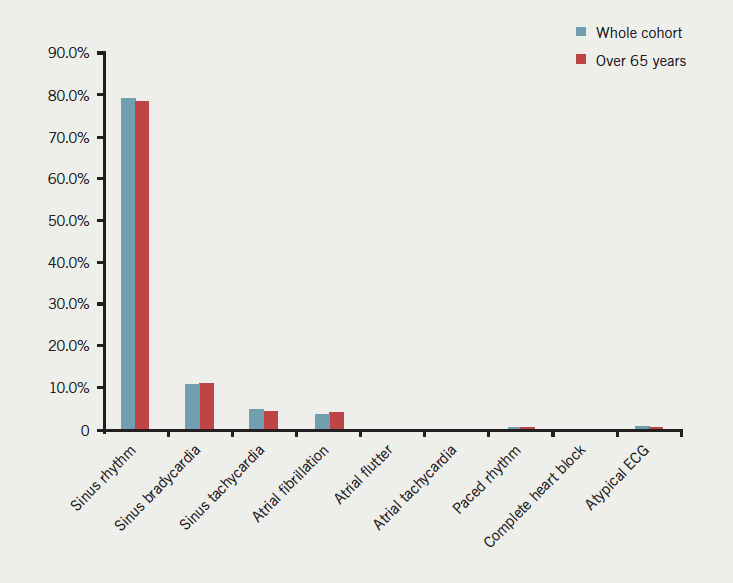
Of patients that took part in the study, 6,036 were aged over 65 years. Of these, 5,859 were screened using limb-lead ECG while the rest used 12-lead ECG. There were 237 patients aged over 65 found to have AF using limb-lead ECG. Therefore, the proportion of patients with AF in this age group rose to 4.1%, when compared with the whole cohort. The gender distribution of patients that took part in this study was 55.6% female and 44.4% male.
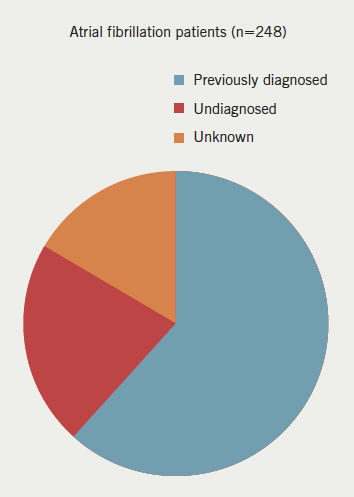
Of the 248 patients detected with AF, 207 were traceable to identify whether they had previously been diagnosed with AF: 153 patients were known to have AF, therefore, ECG screening had identified a further 54 that were previously unknown. Thus, 26.1% of traceable AF patients were detected through this study and were previously unknown (figure 2). Additionally, 14 cases of atrial flutter were also detected, of which all were in the over-65 population.
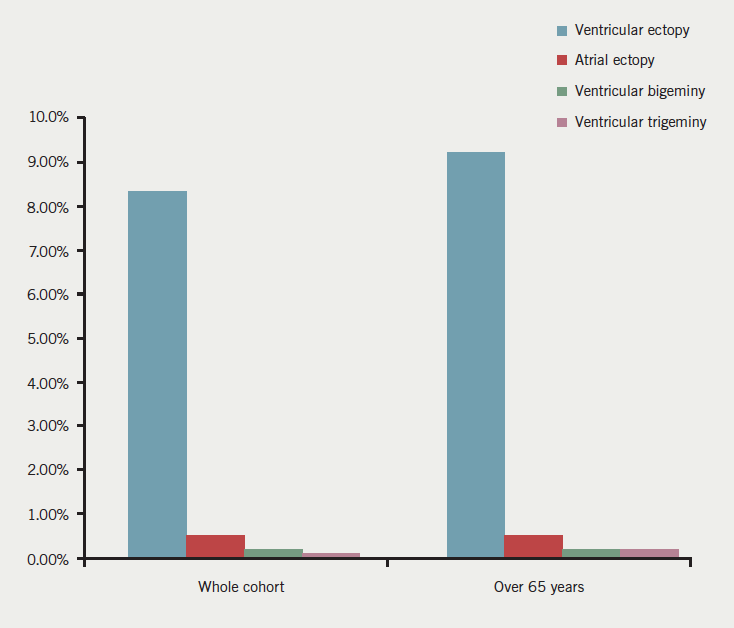
There were 570 cases of ventricular ectopy detected, 537 of these presenting in the over-65 population, a prevalence of 8.3% and 9.2%, respectively. This is significantly higher than the prevalence of AF. However, both abnormalities are capable of presenting as an irregular radial pulse. Additionally, other conditions were detected that may also present as an irregular pulse. These included atrial ectopy, ventricular bigeminy and trigeminy (figure 3). These accounted for a total of 624 cases (9.1%).
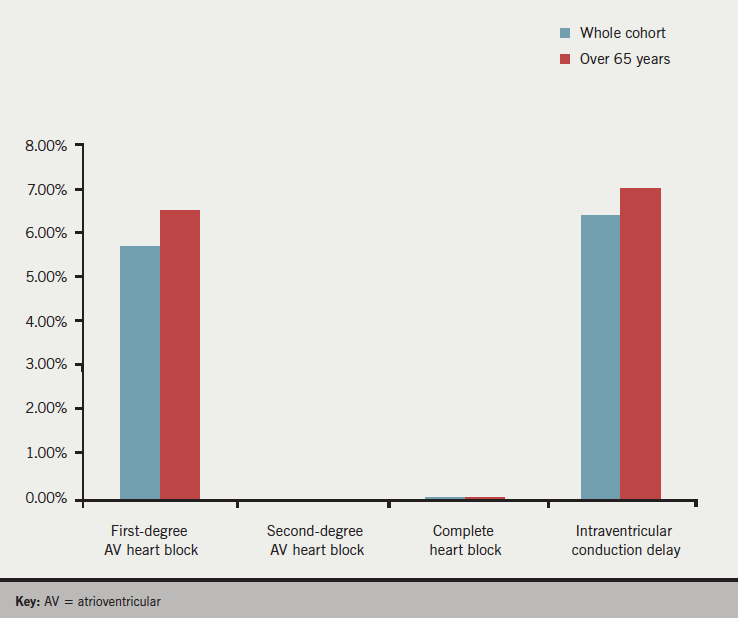
Limb-lead ECG screening identified patients with AV heart block, some of which were isolated and others accompanied with abnormalities such as rhythm disorders. There were 396 cases of first-degree AV heart block identified (5.8%), while 447 (6.5%) patients showed intraventricular conduction delay. The prevalence of both increased in the over-65 population. Smaller numbers of second degree (n=2, 0%) and complete AV heart block (n=4, 0.1%) were detected (figure 4).
ECG interpretation was impossible in 79 ECGs due to 50 transmission errors (0.7%) and 19 (0.3%) poor quality recordings. Also, interpretation was limited but possible in 160 readings (2.3%). Therefore, interpretation was possible in 99% of ECGs and 96.7% of transmitted ECGs were of sufficient quality to allow full interpretation.
In total, 1,129 ECGs were audited by a consultant cardiologist: 52 errors (4.7%) were found in the cardiac physiologist’s interpretations. The most common error was involved in interpreting a PR interval and first-degree AV block. Another common error was failing to identify premature ventricular beats. There were nine significant errors (0.8%), the majority of these were missing intraventricular conduction delays when the QRS duration was prolonged. Also, two patients had rhythms, which may have required pacing, and one case of AF was described incorrectly.
Discussion
AF displayed a prevalence of 3.6%, rising to 4.1% in the over-65 population. As expected from the age group of the study population, 95.6% of patients with AF were aged over 65 years. The prevalence of AF was much lower than other screening studies, such as the SAFE study, where AF prevalence was found to be 8.6% on average. The large difference in AF prevalence between the studies can be explained by the difference in baseline AF prevalence, prior to screening. The baseline prevalence of AF in this study was 2.2% compared with 7.4% in the SAFE study. Hence, the detection rate of new AF cases was similar between the studies. This baseline difference may be due to several reasons. First, Bradford has a younger average population age compared with the rest of the UK. The mean age of participants in this study was 69.7 years compared with 75.3 years in the SAFE study. As AF prevalence exponentially increases with age, this is likely to have played a massive role in the lower baseline AF prevalence. Furthermore, the area is highly diverse with a high number of those with South Asian ethnicity. In fact, it has the largest proportion of people of Pakistani origin in the UK (20.3%). Previous studies have shown AF to have a lower prevalence in this racial group, whether that is due to a protective mechanism or simply because they are more likely to die younger from ischaemic heart disease remains unknown.5
ECG screening identified 248 cases of AF. More importantly, only 153 out of the 207 traceable patients were found to have a previous diagnosis of AF. Hence, screening identified 54 new cases of AF and increased the detection rate by around a third. These newly identified patients may benefit from anticoagulation treatment and, in turn, prevent stroke from occurring. This underlines the impact of screening in the community for AF, particularly given the strong association of AF with stroke, and the social, financial and personal burden that stroke carries.
ECG screening was able to detect various other cardiac abnormalities. Ectopy was a relatively frequent finding, especially in the over-65 age group. It was detected twice as many times as AF. Both ectopy and AF commonly present as an abnormal irregular pulse, therefore, this high rate of ectopy may provide an explanation for the low specificity attributed to pulse palpation screening. It may be argued that opportunistic screening creates unnecessary anxiety for these patients who will require an ECG, possibly at a later time or even in secondary care, hence, wasting valuable time and money when they could have a definitive, instant diagnosis. Superior specificity is one of the main advantages of using ECG screening over opportunistic pulse palpation screening, while limb-lead ECG is less cumbersome and time consuming than conventional 12-lead ECG, which is not necessary for identifying AF. Additionally, screening using limb-lead ECG is capable of detecting other abnormalities including atrial flutter, AV heart block and bundle branch block. The prevalence of first-degree AV heart block and intraventricular conduction delay was relatively high and totalled 11.4%. Such information could be useful in detecting and assessing cardiac dyssynchrony, particularly if there is
underlying heart failure.
The findings of this study are limited in a number of ways. This study was originally designed to test limb-lead ECG equipment by creating a large pool of data instead of being a conventional study with a prior hypothesis in mind. Hence, the data were analysed retrospectively and design faults were inevitable. For instance, 277 cases of AF were initially detected, but only the six-lead ECGs were able to be considered as unique records, therefore, reducing this number to 248. The detection rate of new AF could have been significantly affected if a notable number of these 29 excluded cases were either previously diagnosed with AF or not. This is also the case for the 41 untraceable patients who were unable to be classified as previously diagnosed with AF or not. Also, difficulties arose concerning ages in the data. This was due to some practices entering ‘zero’ as the age of patients. Therefore, these entries had to be removed in order to avoid skewing the data. It is likely that removal of these patients could have also impacted upon the number of AF cases found.
In a prospective study, it would be useful to obtain information such as the presence of symptoms and signs in AF patients in order to calculate prevalence of asymptomatic AF. This is also true for isolated AF by recording the presence of cardiovascular risk factors, such as hypertension, hyperlipidaemia and diabetes. This would provide a better idea of the extent of lone and asymptomatic AF prevalence, both of which are thought to be the main beneficiaries of a systematic screening project, as sufferers are more unlikely to undergo pulse palpation compared with symptomatic AF or those with cardiovascular comorbidity. Also, including information regarding previous dates of AF assessment in patients with newly discovered AF may give an insight into the onset age of AF, while recording ethnicity would allow us to determine if this affected the baseline AF prevalence. Recording ethnicity would also enable us to investigate the effect of ethnicity on AF prevalence. Finally, obtaining follow-up information on the rate of subsequent anticoagulation would provide the true worth of screening, while also identifying any negative impacts of this screening strategy. For example, unnecessary further investigations, such as echocardiography, in patients with prolonged QRS or multi-focal ectopy.
AF is a common condition in the elderly, which shows a strong association with stroke in this age group. This risk is significantly reduced with anticoagulation therapy. Asymptomatic and isolated AF are particularly difficult to diagnose, yet still carry a high risk of stroke. The results of this study confirmed the high rates of AF in the elderly. It demonstrated that limb-lead ECG can be useful as part of a systematic screening programme. It removes the disadvantageous false-positive results of opportunistic pulse palpation screening, while negating the need for a full 12-lead ECG, which is less convenient and requires greater technical ability to perform and interpret. In the future, a screening programme designed to detect new cases of asymptomatic AF may be useful and beneficial. The information it would provide may have far-reaching health, social and economic implications for stroke prevention.
Conflict of interest
MH is the managing director of Technomed who developed the ECG Cloud® system. This was operated by NHS Bradford and Airedale Information Technology Services to collect ECG data. WJ, MF, SL, MT, DF: none declared.
Key messages
- Atrial fibrillation is underdiagnosed, particularly if asymptomatic, leading to unnecessary and preventable strokes
- Screening has been shown to significantly increase detection rates of atrial fibrillation but the best method of screening is unclear
- This study shows systematic limb-lead electrocardiogram (ECG) screening increased atrial fibrillation detection rates by over a third
- A weakness of opportunistic pulse palpation screening was also highlighted by detecting a considerably high incidence of cardiac rhythmic disorders capable of causing an irregular pulse
References
1. Fitzmaurice DA. Routine screening for detection of atrial fibrillation. Future Cardiol 2009;5:213–14. http://dx.doi.org/10.2217/fca.09.3
2. Wilson J, Jungner G. The principles and practice of screening for disease. Public Health Papers 34. Geneva, Switzerland: WHO, 1968.
3. Fitzmaurice DA, Hobbs FDR, Jowett S et al. Screening versus routine practice in detection of atrial fibrillation in patients aged 65 or over: cluster randomised controlled trial. BMJ 2007;335:383–8. http://dx.doi.org/10.1136/bmj.39280.660567.55
4. Morgan S, Mant D. Randomised trial of two approaches to screening for atrial fibrillation in UK general practice. Br J Gen Pract 2002;52;373–80. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1314292/
5. Lip GYH, Bawden L, Hodson R, Rutland E, Snatchfold J, Beevers DG. Atrial fibrillation amongst the Indo-Asian general practice population. The West Birmingham Atrial Fibrillation Project. Int J Cardiol 1998;65:187–92. http://dx.doi.org/10.1016/S0167-5273(98)00125-9
