Transradial access for coronary procedures is associated with less vascular access site complications. Occasionally, radial access fails and makes conversion to a transfemoral route inevitable. In this paper, which updates UK radial experience, we report the outcomes in a single UK centre in developing a transradial access programme.
We analysed 3,225 consecutive patients who underwent transradial coronary procedures over a five-year period. The primary outcome measure was rate of conversion from transradial to transfemoral access route. Of 3,225 radially approached cases, conversion from radial to femoral access route occurred in 148 patients (4.6%). With experience after the learning curve, the conversion rate fell to 2.0%.
In conclusion, after an initial learning curve, procedural success rate is high with low cross-over rate from radial to femoral entry site.
Introduction
Arterial access through the transradial approach was described in the late 1980s.1 Radial approach in coronary interventions has advantages over the femoral approach with less vascular complications, less access site bleeding and earlier discharge post-procedure.2-4 In the PREVAIL (Prospective REgistry of Vascular Access in Interventions in Lazio region) study, patients who underwent coronary procedures through the radial artery had a statistically significant reduction in both major and minor bleeding (4.2% vs. 1.96%, p=0.03) and death or myocardial infarction (3.1% vs. 0.6%, p=0.005).5
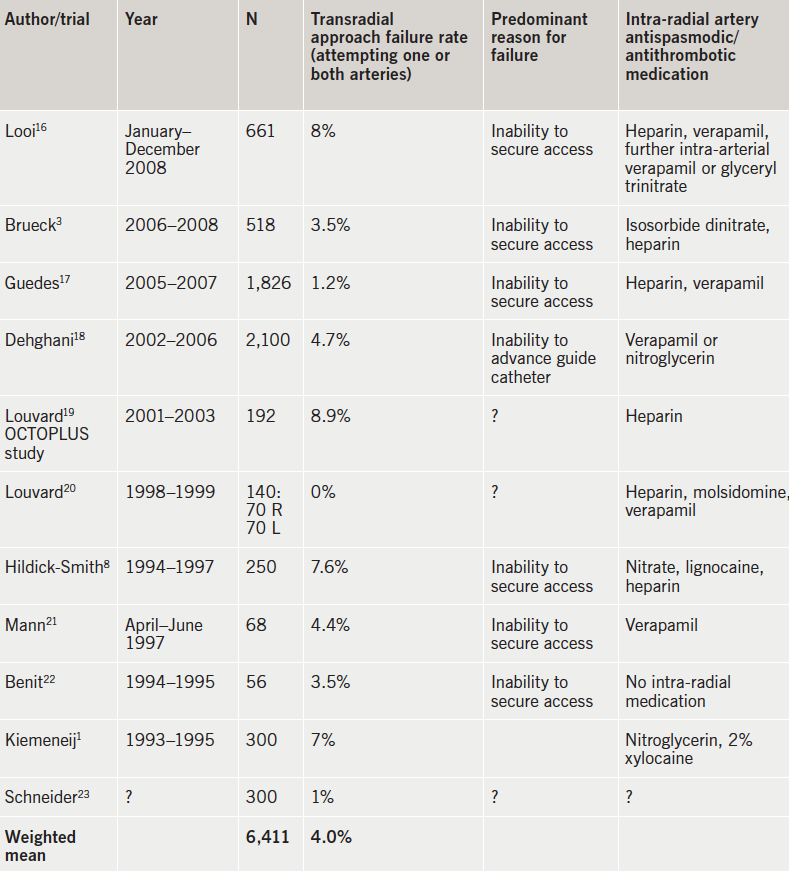
Despite the multiple advantages of the transradial access route, many cardiologists remain unconvinced and unwilling to change practice, as the radial access procedure is technically more challenging, with a steep learning curve. Multiple studies have reported various rates of transradial approach failure, varying from 0 to 8.9% (table 1).
The number of coronary procedures performed via the radial artery access route is increasing, but unfortunately, radial access still accounts for less than 10% of procedures worldwide. In the US, the overall rate of radial use remains at 10–16% of percutaneous coronary intervention (PCI) procedures.6,7
UK literature on this subject is limited. The purpose of this retrospective study is to report a UK single-centre experience developing a transradial approach. High success rate with low radial to femoral cross-over rate are described.
To our knowledge, since a discouraging paper published in 1998,8 this is the first large single-centre study that has assessed conversion rate from radial to femoral approach in a UK centre.
Methods
We studied all consecutive emergency, urgent and elective patients who underwent diagnostic coronary angiography and/or PCI procedures using an initial radial artery vascular access at Watford General Hospital, over five years from April 2009 to March 2014. From these data we identified all patients in whom the procedure was initially started using the radial artery vascular access, but were converted during the procedure to a femoral artery access route. The initial selection of the arterial access route was decided by the operator and the patients’ preference. The radial access site was routinely obtained using local anaesthetic, a 21-gauge needle, 0.018 inch guide wire and 11 cm 5Fr or 6Fr sheaths for diagnostic and PCI procedures, respectively. All cases who had an initial radial artery vascular access approach had routine pre-procedure sublingual glyceryl trinitate 400–800 µg. After introduction of the sheath, all patients also routinely received 50 µg/kg heparin, 200 µg isosorbide dinitrate and 5 mg verapamil by intra-arterial administration through the sheath.
Cardiac procedures in the catheterisation laboratory were reported by the primary operator using the McKesson Horizon Cardiology Medcon reporting module. Cardiac clinical physiologists also separately reported all procedures using the Siemens Sensis angiography reporting module. We reviewed all clinical and procedural data and the outcome of the procedures where more than one vascular access site was used from each database. Indication for the procedure, the type of procedure, operator (diagnostician or interventionalist, consultant or trainee), reason for conversion and any complications during conversion to another arterial access site were documented.
The outcome of this retrospective study was to analyse the conversion rate from radial to femoral arterial access, at our centre over a five-year period of time and over consecutive serial six-month periods. We also documented the reason for conversion and the relationship to the operators’ experience. Analysis of the data was performed using IBM SPSS statistics software. Our data contain categorical variables, which are reported as absolute values and actual percentages. Comparison between categorical variables was performed using Pearson Chi-square test.
Results
A total of 8,912 consecutive diagnostic and interventional coronary angiographic procedures were performed at Watford General Hospital over a five-year period, from April 2009 to March 2014. There were 3,225 cases (36%) done using the radial access route. Of these, 1,374 procedures (43%) were diagnostic angiography and 1,851 (57%) were PCI or potential PCI.
The primary operator in 2,422 (75%) cases was a consultant cardiologist. In 803 procedures (25%) the primary operator was a specialist registrar (trainee), directly supervised by a consultant cardiologist.
In 148 patients (4.6% of the radial cases), the initial vascular access site was changed from radial artery to femoral artery during the procedure. Of these cases, 89 had diagnostic angiography and 59 were interventional cases.
The conversion rate from radial access site to femoral access site was 4.3% in procedures performed by consultants, whereas this rate was 5.6% in procedures in which specialist trainees were the primary operators. This difference was not statistically significant (p=0.11).
The conversion rate from radial access site to femoral access site was 3.8% in procedures performed by interventionalists, and 6.1% in procedures performed by diagnosticians. This difference was not statistically significant (p=0.11).
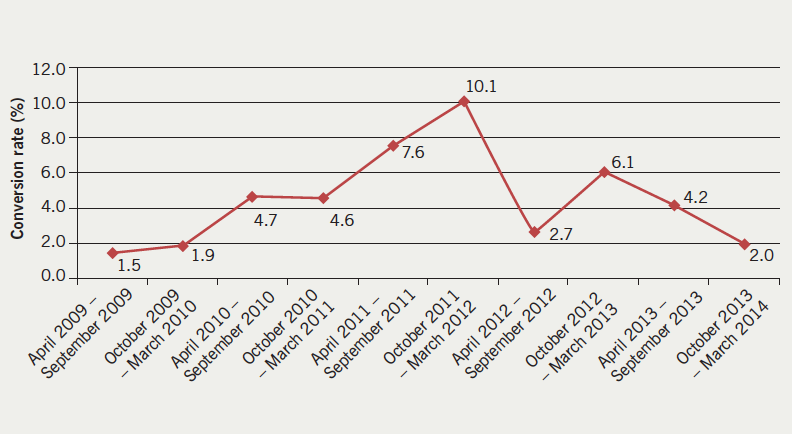
The conversion rate was also assessed over consecutive six-monthly periods (figure 1). The conversion rate was 1.5% (two of 133 cases) during the initial six months of starting the radial approach technique in our laboratories in 2009. The conversion rate increased to a maximum of 10.1% (27 of 267 cases) more than two years later. The most recent conversion rate was 2.0% (9 of 435 cases) between October 2013 and March 2014.
Causes of failed radial attempt
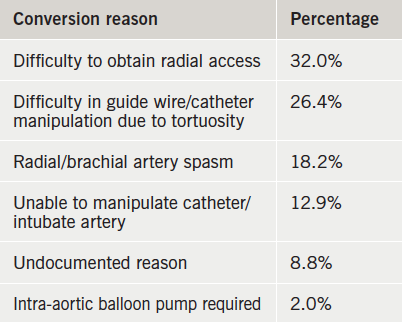
The reasons for conversion from radial to femoral access site in our laboratory are categorised in six main groups and listed in table 2. The most common reason was difficulty in securing radial access (31.8%). This includes inability to puncture the radial artery due to small size, inability to advance the wire through the needle into the artery, and inability to advance the sheath.
The second most common reason of failure was inability to advance the guide wire or catheter due to tortuosity of brachial or axillary artery (26.4%). Inability to advance or manipulate the guide wire and catheter due to radial or brachial spasm accounted for 18.2% of failures. In 12.9% of cases, intubation of the left or right coronary artery was not possible due to difficulty in advancing or manipulating the catheter. In 13 cases (8.8%), no reason for conversion was documented. A further 2% of patients required intra-aortic balloon pump (IABP).
There were no statistically significant differences between various groups of operators (consultants, trainees, interventionists, diagnosticians) in the reasons for conversion from radial access to a femoral one (p=0.76).
Complications
Complications occurred in six of the 148 conversion cases. Five patients developed a vasovagal reaction (3.4%). Dissection of radial artery, which required surgical intervention, occurred in one patient.
Discussion
In 2009, Watford General Hospital commenced a transradial vascular access programme. During early phases of adopting this technique, a relatively small proportion of patients were chosen for this approach. Over the first 12 months of initiating a radial vascular access technique the conversion rate was the lowest of these five years (1.5–1.9%). This high number of successful procedures with low conversion rate may well reflect that less complicated cases were chosen by operators, who were less experienced at the beginning of adopting the radial technique. With increasing experience, the volume of coronary procedures performed via the radial access route increased, including more difficult cases; the conversion rate increased for up to two years.
We believe the operators’ experience and proficiency increased with higher volumes of radial procedures. The concept of a learning curve, in which operators’ skills improve with increased number of procedures, was demonstrated in this observational study. With more experienced operators, the success rate has become more consistent. The conversion rate has fallen to about 2.0% in recent months.
Table 1 lists the conversion rates reported in the medical literature. The overall reported weighted conversion rate was 4.0%. We suggest that, as a clinical standard, an appropriate conversion rate for experienced operators should be approximately 2%, and less than 4%.
In 2013, a common consensus view on the technical, clinical and organisational implications of using the radial approach for coronary angiography and interventions was developed by the European Association of Percutaneous Cardiovascular Interventions (EAPCI).9 The goal of the association was to define the role of the radial approach in modern practice, and to provide a consensus on different aspects of the transradial procedure, such as learning curve and conversion rate. According to this consensus, the conversion rate in recent registries has been as low as 1.5%, which is due to improved technique and materials. In the published literature, however, it varies between zero and 8.9%. The learning curve for radially performed procedures is steep, with no significant difference in failure rate after 50 cases compared with that of experienced operators.7,10 The relationship between volume of procedures and failures demonstrates a high failure rate, with wide inter-operator variability for the first one to 50 radial cases, and a consistent reduction in failure rate with higher transradial volumes. It is agreed that a case-volume threshold of 50–80 transradial procedures is required to overcome the learning-curve threshold.11 This number, however, can be individual and vary from operator to operator.
One study, that has specifically analysed learning curve to assess radially approached coronary procedures, is based on single-centre data from Canada.10 In this study, authors showed that a case-volume threshold of at least 50 transradial procedures was required for new radial operators to achieve similar procedural outcomes as experienced radial performers.
The learning curve experience at our centre was more than 200 cases per operator, considerably more than the literature suggests. Difficulty in obtaining access is one of the main concerns in radial technique. Compared with the transfemoral route, the radial artery is small in size with a tendency to develop spasm. Older, female, and shorter patients more often exhibit anatomic anomalies in the arms,12 as well as tortuous brachiocephalic arteries,13 small radial arteries,12 and radial spasm.14 The most difficult anatomical variations for transradial approach are the radiolunar loop and the presence of a lusoria subclavian artery.15
Difficulty in obtaining access was the main cause of failure of radial attempts in our centre. Difficult arterial puncture and radial artery spasm account for most failures during the first 50 cases.
With increasing transradial experience, operators can select more complex cases without sacrificing procedural success.
Strengths
This study is a large analysis with a low chance of selection bias. It provides contemporaneous data of radial access. Since 1998, when Hildick-Smith et al.8 published a UK experience of coronary angiography from the radial artery – and discouraged this technique due to its limitations – no further studies have assessed radial to femoral conversion rate in a UK centre.
Study limitations
This is a retrospective analysis of a large data set. In our department, consultant cardiologists supervise trainees very closely. This might reflect why any differences between the two groups of operators were not statistically significant.
Conclusion
This single-centre, large, retrospective analysis of all radially performed diagnostic coronary angiography and interventional procedures shows that after an initial learning curve, there is a high success rate with low cross-cover rate from radial to femoral entry site. This low failure rate matches the world literature.
Conflict of interest
None declared.
Key messages
- Transradial access is advantageous over transfemoral access, with fewer vascular complications
- The transradial approach is preferred in ST-elevation myocardial infarction (STEMI)
- After 50–80 cases, the learning-curve threshold will be overcome
- All radial-proficient team members should aim to maintain transfemoral competency
- Training in the procedure is safe when undertaken by trainees supervised by consultants
References
1. Kiemeneij F, Laarman GJ. Percutaneous transradial artery approach for coronary stent implantation. Cathet Cardiovasc Diagn 1993;30:173–8. http://dx.doi.org/10.1002/ccd.1810300220
2. Jolly SS, Yusuf S, Cairns J et al. Radial versus femoral access for coronary angiography and intervention in patients with acute coronary syndromes (RIVAL): a randomised, parallel group, multicentre trial. Lancet 2011;377:1409–20. http://dx.doi.org/10.1016/S0140-6736(11)60404-2
3. Brueck M, Bandorski D, Kramer W, Wieczorek M, Holtgen R, Tillmanns H. A randomized comparison of transradial versus transfemoral approach for coronary angiography and angioplasty. JACC Cardiovasc Interv 2009;2:1047–54. http://dx.doi.org/10.1016/j.jcin.2009.07.016
4. Jolly SS, Amlani S, Hamon M, Yusuf S, Mehta SR. Radial versus femoral access for coronary angiography or intervention and the impact on major bleeding and ischemic events: a systematic review and meta-analysis of randomized trials. Am Heart J 2009;157:132–40. http://dx.doi.org/10.1016/j.ahj.2008.08.023
5. Pristipino C, Trani C, Nazzaro MS et al. Major improvement of percutaneous cardiovascular procedure outcomes with radial artery catheterisation: results from the PREVAIL study. Heart 2009;95:476–82. http://dx.doi.org/10.1136/hrt.2008.150714
6. Feldman DN, Swaminathan RV, Kaltenbach LA et al. Adoption of radial access and comparison of outcomes to femoral access in percutaneous coronary intervention: an updated report from the national cardiovascular data registry (2007–2012). Circulation 2013;127:2295–306. http://dx.doi.org/10.1161/CIRCULATIONAHA.112.000536
7. Hess CN, Peterson ED, Neely ML et al. The learning curve for transradial percutaneous coronary intervention among operators in the United States: a study from the national cardiovascular data registry. Circulation 2014;129:2277–86. http://dx.doi.org/10.1161/CIRCULATIONAHA.113.006356
8. Hildick-Smith DJ, Lowe MD, Walsh JT et al. Coronary angiography from the radial artery – experience, complications and limitations. Int J Cardiol 1998;64:231–9. http://dx.doi.org/10.1016/S0167-5273(98)00074-6
9. Hamon M, Pristipino C, Di MC et al. Consensus document on the radial approach in percutaneous cardiovascular interventions: position paper by the European Association of Percutaneous Cardiovascular Interventions and Working Groups on Acute Cardiac Care and Thrombosis of the European Society of Cardiology. EuroIntervention 2013;8:1242–51. http://dx.doi.org/10.4244/EIJV8I11A192
10. Ball WT, Sharieff W, Jolly SS et al. Characterization of operator learning curve for transradial coronary interventions. Circ Cardiovasc Interv 2011;4:336–41. http://dx.doi.org/10.1161/CIRCINTERVENTIONS.110.960864
11. Burzotta F, Trani C, Mazzari MA et al. Vascular complications and access crossover in 10,676 transradial percutaneous coronary procedures. Am Heart J 2012;163:230–8. http://dx.doi.org/10.1016/j.ahj.2011.10.019
12. Yoo BS, Yoon J, Ko JY et al. Anatomical consideration of the radial artery for transradial coronary procedures: arterial diameter, branching anomaly and vessel tortuosity. Int J Cardiol 2005;101:421–7. http://dx.doi.org/10.1016/j.ijcard.2004.03.061
13. Cha KS, Kim MH, Kim HJ. Prevalence and clinical predictors of severe tortuosity of right subclavian artery in patients undergoing transradial coronary angiography. Am J Cardiol 2003;92:1220–2. http://dx.doi.org/10.1016/j.amjcard.2003.07.038
14. Jia DA, Zhou YJ, Shi DM et al. Incidence and predictors of radial artery spasm during transradial coronary angiography and intervention. Chin Med J (Engl) 2010;123:843–7.
15. Valsecchi O, Vassileva A, Musumeci G et al. Failure of transradial approach during coronary interventions: anatomic considerations. Catheter Cardiovasc Interv 2006;67:870–8. http://dx.doi.org/10.1002/ccd.20732
16. Looi JL, Cave A, El-Jack S. Learning curve in transradial coronary angiography. Am J Cardiol 2011;108:1092–5. http://dx.doi.org/10.1016/j.amjcard.2011.06.009
17. Guedes A, Dangoisse V, Gabriel L et al. Low rate of conversion to transfemoral approach when attempting both radial arteries for coronary angiography and percutaneous coronary intervention: a study of 1,826 consecutive procedures. J Invasive Cardiol 2010;22:391–7.
18. Dehghani P, Mohammad A, Bajaj R et al. Mechanism and predictors of failed transradial approach for percutaneous coronary interventions. JACC Cardiovasc Interv 2009;2:1057–64. http://dx.doi.org/10.1016/j.jcin.2009.07.014
19. Louvard Y, Benamer H, Garot P et al. Comparison of transradial and transfemoral approaches for coronary angiography and angioplasty in octogenarians (the OCTOPLUS study). Am J Cardiol 2004;94:1177–80. http://dx.doi.org/10.1016/j.amjcard.2004.07.089
20. Louvard Y, Lefevre T, Allain A, Morice M. Coronary angiography through the radial or the femoral approach: the CARAFE study. Catheter Cardiovasc Interv 2001;52:181–7. http://dx.doi.org/10.1002/1522-726X(200102)52:2<181::AID-CCD1044>3.0.CO;2-G
21. Mann T, Cubeddu G, Bowen J et al. Stenting in acute coronary syndromes: a comparison of radial versus femoral access sites. J Am Coll Cardiol 1998;32:572–6. http://dx.doi.org/10.1016/S0735-1097(98)00288-5
22. Benit E, Missault L, Eeman T et al. Brachial, radial, or femoral approach for elective Palmaz-Schatz stent implantation: a randomized comparison. Cathet Cardiovasc Diagn 1997;41:124–30. http://dx.doi.org/10.1002/(SICI)1097-0304(199706)41:2<124::AID-CCD3>3.0.CO;2-9
23. Schneider JE, Mann T, Cubeddu MG, Arrowood ME. Transradial coronary stenting: a United States experience. J Invasive Cardiol 1997;9:569–74.
