A 79-year-old lady was taken to the emergency department by her carer, who had noticed an acute deterioration of her general condition. Unfortunately, it was difficult to obtain an accurate history from the patient due to cognitive impairment, and her carer was not aware of her past medical history. However, she had been observed clenching her hands to her chest. She was not previously known to the admitting hospital.
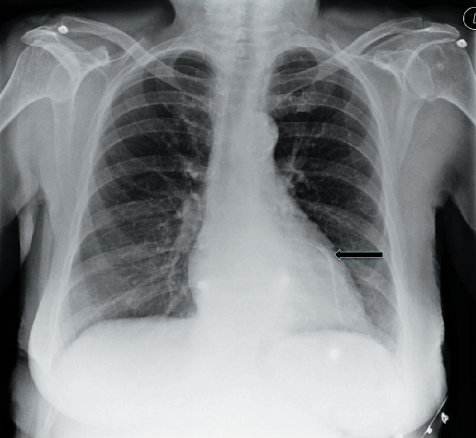
Her physical examination and vital signs were unremarkable. Routine blood tests had been requested. Resting 12-lead electrocardiogram (ECG) showed left bundle branch block; no previous ECGs were available for comparison. A chest X-ray was performed, which gave another clue to the diagnosis…
The chest radiograph (figure 1) shows clear lung fields, normal cardiac contour and, more importantly, a radio-opaque structure across the anterior surface of her heart. This is sometimes termed a ‘full metal jacket’, implying extensive stenting of a coronary artery in its entirety from percutaneous coronary intervention (PCI); in this case, across her left anterior descending artery. This was later confirmed by the patient’s daughter, who reported her mother had undergone multiple PCI procedures in the past. Therefore, acute coronary syndrome (ACS) was suspected, and subsequently confirmed by raised cardiac biomarkers. The patient was successfully treated with medical therapy for ACS and discharged three days later: she was not offered repeat coronary angiography on this occasion due to her clinical presentation and cognitive impairment.
While the classical triad for the diagnosis of ACS is given by a combination of chest pain, ECG changes and elevation of cardiac biomarkers, other basic investigations may play a significant role in formulating the correct diagnosis, particularly in complex circumstances, as in the case we present with this report.
Conflict of interest
None declared.
