Current guidelines recommend against vigorous sports for all patients with an implantable cardioverter defibrillator (ICD). In this study, we established the risk of life-threatening arrhythmias and shocks in patients with an ICD participating in sports.
In this single-centre, cohort survey with 71 patients (59% male) ≤40 years old at ICD implantation and with a left ventricular ejection fraction (LVEF) ≥35%, 16 patients were defined as athlete (exercise ≥5 hours per week). Sports-related and clinical data were obtained using questionnaires and medical records. Median age was 38 years (19–53 years). Median follow-up period was 67 months (11–249 months). Idiopathic ventricular fibrillation (VF) was the most frequent indication (20%) for implantation. There were 22 patients (31%) who experienced 127 shock episodes, of which 112 were appropriate: 15% of shocks occurred during physical exercise. Shocks did not occur more frequently in athletes (25%) compared with non-athletes (33%, p=0.760). Intensity of exercise and appropriateness of shocks were not associated.
In conclusion, we found no evidence that participation in sports contributed to the risk of life-threatening arrhythmias and (in)appropriate ICD shocks in patients with an ICD. In individual cases, the advice to participate in sports could be more lenient compared with current guidelines.
Introduction
An implantable cardioverter defibrillator (ICD) is used for primary and secondary prophylaxis in the treatment of life-threatening arrhythmia. Guidelines for ICD patients, originally published in 2005, advise against any competitive sports more vigorous than ‘Class IA’ activities such as bowling or golf.1 American College of Cardiology (ACC)/American Heart Association (AHA)/European Society of Cardiology (ESC) embraced this advice stating “for legal and ethical reasons athletes receiving cardiovascular drugs and devices such as pacemakers and ICDs are generally not allowed to participate in high-grade competition.”2 For leisure-time sports, Heidbuchel et al. allow exercise from six weeks after an ICD implantation with assessment of expected maximal sinus rate and/or preponderance for atrial fibrillation with prophylactic institution of antiarrhythmic or bradycardic therapy.3
The postulated risks on which these restrictions are based, are, first, increased risk of defibrillator shocks, both appropriate and inappropriate, and, second, potential failure of a shock to convert a life-threatening arrhythmia. Competing athletes have an increased adrenergic tone, which may reduce the efficacy of defibrillator shocks. Third, in some sports, such as weightlifting and golf, repetitive arm-motion can induce excessive stress on lead systems. Contact sports have a risk of device and lead damage.4 Finally, adverse events have been reported due to arrhythmia or shock during sports participation, for instance falling from a bicycle while having an arrhythmia treated by an ICD shock.4
Young athletes with an ICD and preserved left ventricular function are often caught between the passion to continue their sport and the guidelines, which are felt to be too restrictive. At the heart of this dilemma is a lack of evidence about the natural history of athletes with an ICD participating in (competitive) sports. As there are no prospective data in elite athletes with ICDs, the current guidelines are based on realistic, albeit largely theoretical, considerations without the essential level-of-evidence classifications. Evidence is needed to guide these patients, their families and physicians to make an informed decision about sports participation.
To address this issue, we performed a retrospective single-centre cohort survey in which the primary end points were to establish:
- Whether participating in sports for patients with an ICD is related to an increased risk of untreatable ventricular arrhythmias.
- Whether athletes with an ICD received more frequently appropriate shocks compared with non-athletes.
Additionally, the following secondary end points were addressed:
- Is the intensity level of the sport related to the initiation of ICD shocks?
- Is there an association between the indication for ICD implantation (diagnosis, primary or secondary prophylaxis) and the occurrence of (in)appropriate shocks?
- Are certain sport activities more likely to induce life-threatening arrhythmias?
- What is the risk of damage to the cardioverter device during physical exercise and does this result in an increased risk of receiving (in)appropriate shocks?
Materials and methods
For this cohort-survey we analysed all patients from our ICD database over the period of 1992 to 2010. We included all patients younger than 40 years of age with a preserved left ventricular ejection fraction (LVEF >35%) at implantation of the device. Ninety-five patients with an ICD were included. LVEF was assessed by ultrasound, radionuclide heart scan or magnetic resonance imaging (MRI). All participants were interviewed via telephone using a questionnaire (available on request). Sports performed by the participants before and after implantation of the device were classified using the Bethesda Classification of Sports.1 Other descriptive variables obtained from the questionnaires, such as prevalence of both appropriate and inappropriate ICD shocks, were categorised in groups and compared with a similar group of patients who did not experience shocks.
To define ‘sport’ we used the World Health Organization’s definition: “Physical activity with a described functional purpose, e.g. competition, practicing for competition, improving physical health. This includes practice and training as well as pre-event (e.g. taping, dressing), warm-up, cool down, and post-event (e.g. showering, dressing) activities. Travel to and from the event or activity is not included.”5
As an athlete we classified those participants who exercised ≥5 hours per week on a structural basis, in analogy of Drezner et al.6
An ‘appropriate shock’ was considered to be a shock delivered by the ICD because of a life-threatening arrhythmia (ventricular tachycardia [VT] or ventricular fibrillation [VF]). An ‘inappropriate shock’ was considered to be a shock delivered by the ICD because of any other reason, for instance supraventricular tachycardia or malsensing. To decide whether the shock was appropriate, the treating physician’s diagnosis after interrogation of the ICD was used.

All data were entered into a computerised database. Descriptive statistics were provided, and cross-tabulation and subsequent Chi-square tests were performed for categorical and dichotomous variables. The study population was categorised in groups: athletes versus non-athletes. Variables were untreatable arrhythmias and appropriate shocks for analysis of primary end points. To analyse whether the intensity level of the sport relates to the initiation of ICD shocks, we categorised our study population in groups using the Bethesda classification of sports.1 To analyse whether there is an association between the indication for implantation of an ICD and the occurrence of shocks, we categorised our study population in groups using International Classification of Diseases, version 10. The same test was performed categorising the study population in groups according to primary or secondary prophylaxis. To analyse whether certain sport activities are more likely to induce life-threatening arrhythmias we categorised the study population in groups according to sport: contact sports, arm sports, swimming, fitness, endurance sports, horseback riding, other sports. The variable in this case was untreatable arrhythmias. To assess the risk of damage to the ICD device we used the same groups as in the third question, variable in this case was damage to ICD device.
Data were analysed using SPSS version 20.0 and a p value <0.05 was considered as significant.
Results
A total of 95 patients fulfilled the inclusion criteria, of whom, 19 were lost to follow-up and two patients did not want to participate. The patients who were lost to follow-up came to our hospital for ICD implantation only. After the operation they went back to their own cardiologist’s practice for follow-up. These patients must have moved in the meantime, since the registered contact details no longer worked. Three patients died during the follow-up period because of non-related causes. We did not include these three patients in our analysis because it was not possible to establish whether they would have met the criteria for an athlete.
The median age of the 71 remaining participants was 38 years (range 19–53 years). The median age at ICD implantation was 30 years (range 14–40 years). Median follow-up after implantation was 67 months (range 11–249 months). Demographic and clinical characteristics of our population are shown in table 1.
The most frequent diagnosis for ICD implantation in our study population was idiopathic VF (20%). In 62% of participants the ICD was implanted as secondary prophylaxis. Before ICD implantation the most common sports in our population were equally divided over fitness (18%), endurance (18%) and contact sports (17%). A total of 10 patients did not participate in any sport before ICD implantation. After implantation a considerable part of our population became non-athletic (29 patients) or even quit exercising (26 patients). Time spent exercising decreased after ICD implantation, from an average of 4.1 hours per week to 2.7 hours per week (table 1). The most common sports remained endurance sports and fitness. Patients participating in swimming sports before ICD implantation (n=4) all quit after implantation.
Of our study population, 70% stated that their cardiologist advised them to either quit their sport or to choose another, less vigorous type of sport according to Bethesda classification. Prudence enforced by restrictive current guidelines was the basis for this advice. Interestingly, 89% of our study population said they were confident to exercise, even after receiving a shock, although only 63% actually participated in sports in one form or another.
Primary end points
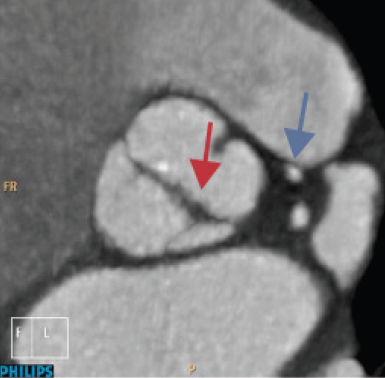
There were 22 patients (31% of study population) who experienced 127 shock episodes. Eventually, 112 (88%) of these shock episodes were shown to be appropriate (figure 1). In our study population, six individuals experienced an electrical storm, i.e. ≥3 distinct episodes of VT/VF in 24 hours (8% of our study population). In the present survey, electrical storms occurred in patients with idiopathic VF (n=3), hypertrophic cardiomyopathy (n=1), long QT syndrome (n=1) and arrhythmogenic cardiomyopathy (n=1). None of our patients with catecholaminergic polymorphic VT experienced an electrical storm, even though electrical storms are common in this cardiac condition.7 Two of the six persons who experienced an electrical storm had it during exercise, i.e. walking and delivering a baby. Only one of these six persons experiencing an electrical storm was classified to be an athlete.

Overall, 15% of both appropriate and inappropriate shocks occurred during exercise. Athletes did not receive shocks more frequently than non-athletes (p=0.760). ICD shocks in athletes were not more frequently appropriate nor inappropriate compared with non-athletes (p=0.501).
Secondary end points
We could not establish a relationship between receiving either appropriate or inappropriate shocks and the level of physical exercise or the kind of sports. This is due to small sample size; we didn’t perform a power analysis on secondary end points. Eleven patients received a shock during physical exercise. When classified in groups according to the Bethesda classification,1 three patients received a shock during exercise at low intensity (VO2max <40%) and six patients received a shock during exercise at high intensity (VO2max >70%). One patient in this group received a shock when having sexual intercourse and one patient during delivery of a baby.
Shocks during or after high-intensity physical activity occurred in patients with idiopathic VF (n=3), hypertrophic cardiomyopathy (n=1), catecholaminergic polymorphic VT (n=1) and arrhythmia not specified (n=1). Shocks occurred during low-intensity physical activity in individuals with Brugada syndrome (n=1), arrhythmogenic cardiomyopathy (n=2) and idiopathic VF (n=2). Specific details on the 20 patients receiving either an appropriate or inappropriate shock are available on request. In this analysis, more non-athletes than athletes received a shock, both in rest and during exercise. The athletes in our study population did not experience more damage to their leads or devices than the non-athletes (p=1.000).
In a subgroup analysis, we found that receiving ICD shocks was not associated with the cardiac diagnosis (p=0.224). This was also the case for receiving appropriate shocks in relation to the cardiac diagnosis (p=0.505). Moreover, the indication (primary or secondary) for implanting the device was not associated with receiving shocks (p=0.075) nor with receiving appropriate shocks (p=0.153).
Discussion
The guidelines for cardiac patients with an ICD restrict physical activity to the level IA (meaning a low dynamic and low static component) sports, e.g. playing golf or billiards, the rationale being the fear for intractable VT/VF during more demanding sports. However, no risk stratification based on, for instance, underlying cardiac disease or LVEF has ever been made, and so one wonders whether there are subsets of patients with an ICD for which the restrictions can be eased.
In this study, we could not establish that in patients under 40 years with an ICD and a LVEF >35%, performing vigorous sports, were at greater risk of appropriate or inappropriate shocks compared with patients who did not perform these sports. This was true for all the indications (underlying cardiac disease, primary or secondary indication). So far, our study included the largest population. Due to the lack of consensus on clinically important event rates, a sample size calculation cannot be performed. The way this study was designed, the possibility of a selection bias was minimised. The population represents a cross-section of a population with an ICD not restricted by further selection of a population with a certain type or brand of cardioverter device.
The number of both appropriate and inappropriate shocks are in line with the numbers found in the literature,8 although it concerned patients with a reduced LVEF (<35%) after myocardial infarction. We note that our follow-up time was longer.
There are only limited data on the safety of sports in ICD patients. Lampert et al. found in 372 patients engaged in organised or high-risk sports (meaning that loss of consciousness could result in severe injury or death) that 10% received a shock, of which about half were appropriate.9 In a subset of 60 young patients (<21 years), from university teams engaging in competitive sports, 28% received 25 shocks, of which only half were appropriate and only two occurred during competition or practice, and six during other physical activity. There was no statistical difference in shock frequency between the competitive and the non-competitive groups.
The follow-up period of Lampert’s study was 31 months (median) with a slightly younger population (average age 33 years, median).9 In our study, the follow-up time was 67 months (median) with an average age of 38 years (median): our estimates are, therefore, more precise. The incidence of shocks in our study group and in the young competitive group of Lampert et al. was similar, thus, indicating a low a priori risk.9 Although it is tempting to speculate that the incidence of ICD shocks may not change over time in this subpopulation, this has not been established yet.
From this study, it cannot be inferred whether the underlying diagnosis must influence a decision to engage as an athlete or not, since a wide diversity of diagnoses for which the ICD was implanted was present in the cohort. However, it concerned relatively young patients with a preserved LVEF and there were no reasons, other than the ICD implantation itself and the concomitant fear of a life-threatening arrhythmia provoking an ICD shock, not to engage in sports. A reason not to engage as an athlete could be the evidence that sport indeed lowers the arrhythmia threshold. This has been described in a study with patients with arrhythmogenic right ventricular cardiomyopathy.10 A subset of patients with hypertrophic cardiomyopathy and VT/VF during exercise testing are also more at risk of VT/VF during exercise.11 An association of VT/VF with exercise was found in polymorphic catecholaminergic VT and long QT syndrome type I, but not in Brugada syndrome nor idiopathic VF.12 Although it may be inferred that exercise can provoke arrhythmias in some patients with the above-mentioned diagnoses, an athletic lifestyle does not apparently increase the risk of ICD in these categories.
We realise that the ICD implantation itself has an effect on performing sports and on the type of sports performed (figure 2). ICD patients tend to give up sports, especially contact sports or arm sports. Swimming was given up altogether. However, a lot of participants admit that they would like to do some sort of exercise but that they were advised against. Another explanation to give up sport or to choose another sport can be found in psychological factors, such as the fear to provoke an ICD shock. After ICD implantation, the most frequently performed sports were fitness and endurance sports. Some athletes participated in moderate contact sports like soccer and hockey; none played more aggressive contact sports, such as rugby or ice hockey. It is possible that damage to the ICD system would have occurred in these types of exercise. Therefore, the results from this study must be restricted to this category.

A limitation of this survey is its retrospective design. Three possible sources of bias are recognised: the 19 subjects, lost to follow-up, are possibly a deviating subgroup; differences in athlete/non-athlete group characteristics as the groups were not randomised; and recall bias. To deal with the first of these we checked the underlying diagnosis and the demographics of these 19 subjects: there were no relevant differences in baseline characteristics, e.g. age, LVEF or underlying disease. We, thus, conclude that they were ‘missing at random’. When subjects are deemed to be more prone to shocks than others, the advice to stop exercising will/may be more stringent. These subjects will easily slip into the non-athlete group and show possibly a higher shock rate: this ‘increased probability’ was comparable with the shock rate in athletes, which is then also ‘higher’ as expected. At the moment, however, there are no clear objective reasons and/or diagnosis to advise stronger against sports and we judge this mechanism as improbable. The third source, recall bias, must be assumed to be present, while realising the profound effect of a shock on the subjects’ psyche. Recall bias, however, to invalidate the outcome must be unequally distributed over the athlete/non-athlete groups: when both groups suffer from the same amount of recall bias, the effects are similar and do not influence the comparison. There is no reason to assume that one group suffers from stronger recall bias.
Another possible limitation of this survey is the length of the follow-up period. Five and a half years of follow-up, on average, is a long time, however, we cannot predict whether this period is long enough to make recommendations for a patient’s lifetime. On the other hand, there is currently no study with a longer follow-up period.
Conclusion
In young patients with an ICD and with a preserved LVEF, we found no evidence that participation in sports (mainly endurance sport and fitness) contributed to the risk of life-threatening arrhythmias and
(in)appropriate ICD shocks.
The current guidelines for performing sports with an ICD may be too restrictive for some patients. Patient-tailored advice is recommended for patients who want to continue their sport activities after ICD implantation, which might include lifting the restrictions to sport beyond the IA category.
Sources of support for research
None.
Conflict of interest
None declared.
Editors’ note
Additional information showing the number of appropriate and inappropriate shock events and the diagnosis for ICD implantation is available on request. Email: editorial@bjcardio.co.uk
Key messages
- There is no increased risk of untreatable ventricular arrhythmias for young patients participating in sports with an implantable cardioverter defibrillator (ICD) (≤40 years old) and with a preserved left ventricular ejection fraction (LVEF)
- Athletes with an ICD do not receive more frequent appropriate shocks compared with non-athletes
- The intensity level of sport is not related to the occurrence of shocks
- In individual cases, the advice to participate in sports could be more lenient compared with current guidelines
References
1. Maron BJ, Zipes DP. 36th Bethesda Conference: eligibility recommendations for competitive athletes with cardiovascular abnormalities. J Am Coll Cardiol 2005;45:1313–75. http://dx.doi.org/10.1016/j.jacc.2005.02.006
2. Zipes DP, Camm AJ, Borggrefe M et al. ACC/AHA/ESC 2006 guidelines for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death. Europace 2006;8:746–837. http://dx.doi.org/10.1093/europace/eul108
3. Heidbuchel H, Corrado D, Biffi A et al. Recommendations for participation in leisure-time physical activity and competitive sports of patients with arrhythmias and potentially arrhythmogenic conditions. Part II: ventricular arrhythmias, channelopathies and implantable defibrillators. Eur J Cardiovasc Prev Rehabil 2006;13:676–86. http://dx.doi.org/10.1097/01.hjr.0000239465.26132.29
4. Lampert R, Philip Saul J. Chapter 18. Athlete with a device: implantable cardioverter defibrillators and pacemakers. In: Lawless CE, ed. Sports Cardiology Essentials. Evaluation, Management and Case Studies. New York, NY: Springer, 2011. http://dx.doi.org/10.1007/978-0-387-92775-6_18
5. Valkenberg H, Schoots W, Van Nunen M et al. Handboek Epidemiologie Sportblessures, versie 4.1. Stichting Consument & Veiligheid, maart 2010.
6. Drezner JA, Fischbach P, Froelicher V et al. Normal electrocardiographic findings: recognising physiological adaptations in athletes. Br J Sports Med 2013;47:125–36. http://dx.doi.org/10.1136/bjsports-2012-092068
7. Miyake CY, Webster G, Czosek RJ et al. Efficacy of implantable cardioverter defibrillators in young patients with catecholaminergic polymorphic ventricular tachycardia: success depends on substrate. J Circ Arrhythm Electrophysiol 2013;3:579–87. http://dx.doi.org/10.1161/CIRCEP.113.000170
8. Daubert JP, Zareba W, Cannom DS et al. Inappropriate implantable cardioverter-defibrillator shocks in MADIT-II: frequency, mechanisms, predictors and survival impact. J Am Coll Cardiol 2008;51:1357–65. http://dx.doi.org/10.1016/j.jacc.2007.09.073
9. Lampert R, Olshansky B, Heidbuchel H et al. Safety of sports for athletes with implantable cardioverter-defibrillators: a prospective, multinational registry. Circulation 2013;127:2021–30. http://dx.doi.org/10.1161/CIRCULATIONAHA.112.000447
10. James CA, Bhonsale A, Tichnell C et al. Exercise increases age-related penetrance and arrhythmic risk in arrhythmogenic right ventricular dysplasia/cardiomyopathy-associated desmosomal mutation carriers. J Am Coll Cardiol 2013;62:1290–7. http://dx.doi.org/10.1016/j.jacc.2013.06.033
11. Gimeno JR, Tome-Esteban M, Lofiego C et al. Exercise-induced ventricular arrhythmias and risk of sudden cardiac death in patients with hypertrophic cardiomyopathy. Eur Heart J 2009;30:2599–605. http://dx.doi.org/10.1093/eurheartj/ehp327
12. Prystowsky EN, Padanilam BJ, Joshi S, Fogel RI. Ventricular arrhythmias in the absence of structural heart disease. J Am Coll Cardiol 2012;59:1733–44. http://dx.doi.org/10.1016/j.jacc.2012.01.036