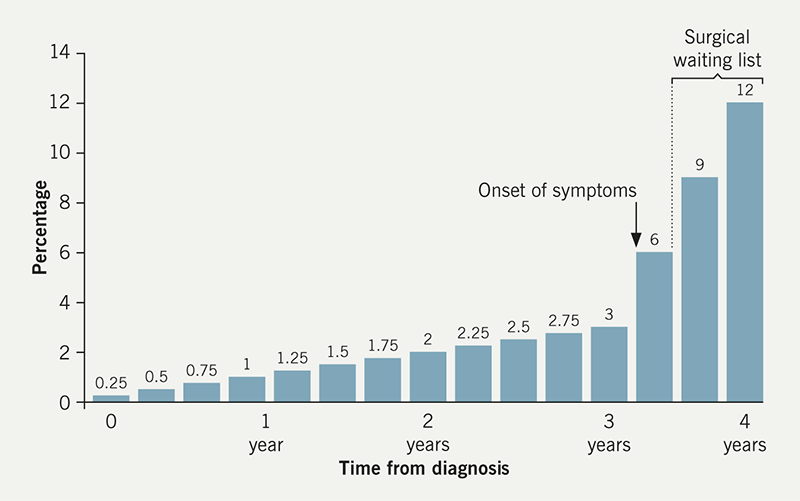
Echocardiography is key for the assessment of aortic stenosis (AS), but taking a good history is also crucial and requires specialist competency. Symptomatic AS requires surgery and, if physicians miss the onset of symptoms, the risk of death rises from 1% per annum in patients without symptoms to 14% on a six-month surgical waiting list. A case is described illustrating the difficulty of obtaining the history in a patient with AS, and suggests how to take a careful history and questions to ask. Patients with a murmur suggesting AS should be considered for a specialist valve clinic.
Introduction
Aortic stenosis (AS) is the most common type of primary heart valve disease in industrialised countries. Although echocardiography is key for its assessment, the need for surgery is most frequently dictated by symptoms.1 However, the history can be surprisingly elusive, and physicians without specialist competencies in valve disease may miss their onset.2 This is important because the risk of death is approximately 1% per annum without symptoms but 4% in the first three months after the onset of symptoms,3 usually before the patient has time to contact their physician (figure 1). It then rises up to 14% on a six-month surgical waiting list.4
Case history
A 75-year-old man was referred to a specialist valve clinic for surveillance of apparently asymptomatic severe AS. He reported no breathlessness or chest pain, and the referring cardiologist had noted that he could still work in his garden. On further enquiry, he described having to stop frequently after each task in the garden. He was mildly breathless, but put this down to ageing and had not thought to mention it. His daughter said he had slowed down and become less active over the past year. The blood pressure was 145/80 mmHg with a pulse rate of 75 bpm. There was a long ejection systolic murmur, maximal towards the apex, but radiating to the carotid area, and associated with a soft second sound. On echocardiography the aortic valve was heavily calcified with peak velocity 4.0 m/s, mean gradient 40 mmHg and effective orifice area 0.8 cm2, all indicating severe AS. Because of the discrepancy in assessment and the relative non-specificity of his symptoms, he was asked to walk on a treadmill using a Bruce protocol modified by two warm-up stages, under supervision from a cardiologist. He became severely breathless after five minutes (expected exercise capacity 15 minutes), and the systolic blood pressure fell from 140 to 80 mmHg. The test was stopped immediately and he recovered fully within three minutes. With his consent, he was referred for an urgent surgical opinion.
Discussion
Symptoms are the main indication for surgery in severe AS,1 but in most patients their onset is subtle. In a widely referenced series,5 38% of patients had aortic valve replacement for reduced exercise capacity and only 23% for heart failure, 15% for chest pain and 12% for exertional dizziness. In 12%, surgery was performed prophylactically because the risk of surgery, 1.5% in the UK for all ages and presentations,6 is far lower than the risk of dying before surgery if symptoms are missed.
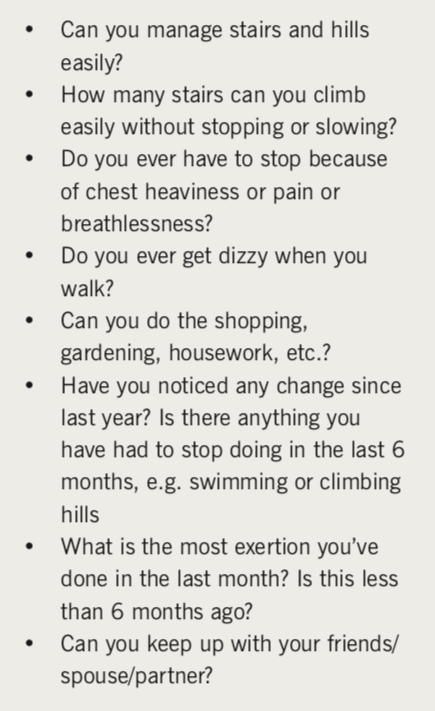
The history is, therefore, crucial. Because patients tend to slow down to avoid overt symptoms, it is important to ask questions about exercise capacity and, particularly, changes in exercise ability (table 1). It is worth repeating the question in different forms, and important to ask friends or relatives, who are more likely than the patient to notice a change. If the patient appears genuinely asymptomatic, or if the history is equivocal, a supervised symptom-limited treadmill exercise test should be performed.1 It is also worth chatting further, before and during the exercise test, since this makes the test more relaxed, and the patient may have had a chance to remember more details. Treadmill exercise reveals symptoms in 38% of apparently asymptomatic patients with severe AS and is safe,7 provided it is stopped for symptoms or if the blood pressure falls. Exercise testing is not indicated if there are unequivocal spontaneous symptoms, or if surgery will only be done for severe spontaneous symptoms (e.g. in the presence of major comorbidity or advanced age). Clearly, patients who are unable to exercise adequately should not be put on a treadmill, and if there are multiple potential causes of symptoms (e.g. chronic obstructive pulmonary disease [COPD] or obesity) interpretation is likely to be difficult or impossible. In these, the B-type natriuretic peptide (BNP) level or respiratory function test or the correlation of a change in test results against the development of symptoms is sometimes helpful.
Untreated symptomatic severe AS has a prognosis as poor as many cancers. For this reason, it is important to consider surgery at the first evidence of decompensation, or even prophylactically (e.g. Vmax >5.0 m/s),1,8 provided surgical risk is low. The significance of AS may be underestimated, not only by the difficulty of the history, but because the examination is an unreliable guide to severity.9 The presence of a normal or high systemic blood pressure is often thought to exclude severe AS. In fact, the ‘textbook’ low systolic pressure with a narrow pulse pressure was described when AS was predominantly caused by rheumatic disease presenting in young or middle-aged people. Calcific degenerative disease is the dominant aetiology today for which age, dyslipidaemia, diabetes, smoking and, importantly, systemic hypertension are risk factors. Systemic hypertension now occurs in around three quarters of patients with moderate or severe AS.7
Patients with a murmur suggesting AS should be considered for a specialist valve clinic, which is able to identify symptoms far sooner than usual care.10 This case illustrates how the history must include more than a simple enquiry for overt symptoms to avoid missing high-risk cases requiring surgery. A careful history could avoid a needless death.
Key messages
- Taking a careful history is crucial in all patients with aortic stenosis (AS)
- Symptoms as an indication for surgery in AS can initially be non-specific and an exercise test should be considered as an extension of the history
- All patients with valve disease, including AS, should be considered for a specilaist valve clinic
Conflicts of interest
None declared.
Consent
The patient is not identifiable from the case report since this is all too common a scenario.
References
1. Baumgartner H, Falk V, Bax JJ et al. 2017 ESC/EACTS guidelines for the management of valvular heart disease. Eur Heart J 2017;38:2739–86. https://doi.org/10.1093/eurheartj/ehx391
2. Chambers J, Campbell B, Wilson J, Arden C, Ray S. How should specialist competencies in heart valve disease be recognised? Quart J Med 2015;108:353–4. https://doi.org/10.1093/qjmed/hcv002
3. Pellika PA, Nishimura RA, Bailey KR, Tajik AJ. The natural history of adults with asymptomatic, hemodynamically significant aortic stenosis. J Am Coll Cardiol 1990;15:1012–17. https://doi.org/10.1016/0735-1097(90)90234-G
4. Malaisrie SC, McDonald E, Kruse J et al. Mortality while waiting for aortic valve replacement. Ann Thoracic Surg 2014;98:1564–71. https://doi.org/10.1016/j.athoracsur.2014.06.040
5. Otto CM, Burwash IG, Legget ME et al. Prospective study of asymptomatic valvular aortic stenosis. Clinical, echocardiographic, and exercise predictors of outcome. Circulation 1997;95:2262–70. https://doi.org/10.1161/01.CIR.95.9.2262
6. Bridgewater B, Keogh B, Kinsman R, Walton P. Demonstrating quality: the sixth National Adult Cardiac Surgery database report. Henley-on-Thames, UK: Dendrite Clinical Systems Ltd., 2009. Available from: https://scts.org/_userfiles/resources/SixthNACSDreport2008withcovers.pdf
7. Saeed S, Rajani R, Parkin D, Chambers JB. Safety and tolerability of exercise testing in asymptomatic patients with moderate to severe aortic stenosis. Heart 2018;104:1836–42. https://doi.org/10.1136/heartjnl-2018-312939
8. Taniguchi T, Morimoto T, Shiomi H et al. Initial surgical versus conservative strategies in patients with asymptomatic severe aortic stenosis. J Am Coll Cardiol 2015;66:2827–38. https://doi.org/10.1016/j.jacc.2015.10.001
9. Das P, Pocock C, Chambers J. The patient with a systolic murmur: severe aortic stenosis may be missed during cardiovascular examination. Quart J Med 2000;93:685–8. https://doi.org/10.1093/qjmed/93.10.685
10. Zilbersac R, Lancellotti P, Gilon D et al. Role of a heart valve clinic programme in the management of patients with aortic stenosis. Eur Heart J Cardiovasc Imaging 2017;18:138–44. https://doi.org/10.1093/ehjci/jew133

