Infective endocarditis (IE) is an increasingly common disease associated with significant morbidity and mortality. It is known that the incidence of IE has been rising globally, but the reasons for this rise are not fully understood. This study sought to investigate the epidemiology of IE in a UK population, with a review of mortality outcomes based on current clinical practice.
Introduction
Infective endocarditis (IE) is a relatively rare disease; however, it is becoming increasingly common and is associated with significant morbidity and mortality.1 A recent meta-analysis has revealed that the epidemiology of IE has evolved over the last five decades,2 with significant global variation. Several large epidemiological studies show that the incidence of IE is increasing, particularly in male and elderly patients.3-5 There have also been changes in the microbiology of IE with staphylococci overtaking streptococci as the most frequent causative organism.6 There are few recent studies describing the incidence or epidemiology of IE in the UK. We carried out a retrospective analysis of IE cases from 2010 to 2017 in a rural district general hospital.
Method
We conducted a retrospective analysis of the medical records of patients who were treated for IE at a rural district general hospital in Herefordshire between 1 January 2010 and 31 December 2017. All patients aged over 18 years, who were diagnosed with IE, were included in the study.
Demographic, clinical, microbiological and clinical outcome data were gathered from patients’ medical records. Incidence rates were calculated as the number of IE cases per 100,000 person-years, with the assumption that the entire adult population of Herefordshire was at risk. The denominators of age- and sex-specific person-years were derived from Herefordshire census data.
A multi-variable Poisson regression model was used to determine if there was a significant temporal trend in the incidence of IE over the study period. Age, sex and year were entered into the model as explanatory variables. A p value of less than 0.05 was considered significant.
Results
Forty-eight cases of IE were identified over the study period. These cases represented 46 patients, two of whom were treated for IE twice during the study period. Forty cases were from patients resident in Herefordshire. The remaining eight cases were patients resident in counties bordering Herefordshire.
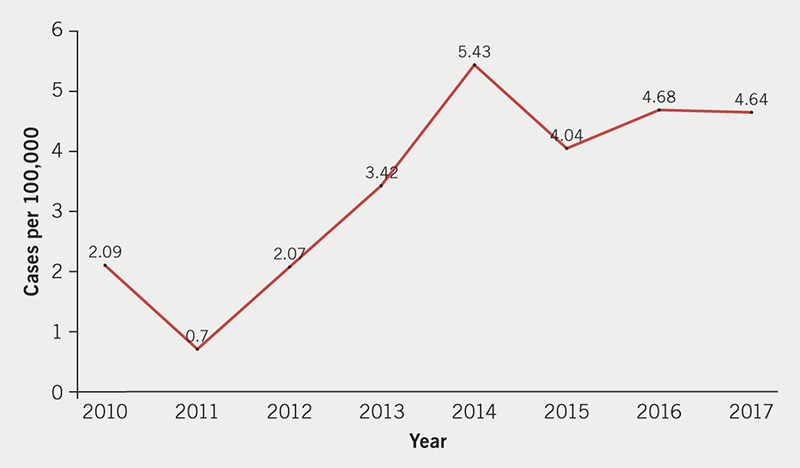
The total age- and sex-adjusted incidence rate of IE over the study period was 3.4 cases per 100,000 person-years. Poisson regression showed a statistically significant increase in the annual incidence of IE in Herefordshire between 2010 and 2017 (95% confidence intervals [CI] 1.011 to 1.416, p=0.036) (figure 1).
IE was more common in males (62.5%) than females (37.5%). Native valve disease was the most common predisposing risk factor for IE (43.8% of patients). Thirty-one percent of patients had a prosthetic valve (n=15). Other predisposing conditions included congenital heart disease (14.6%), previous IE (12.5%), presence of an implantable cardiac device (12.5%), intravenous drug use (8.3%) and hypertrophic obstructive cardiomyopathy (HOCM) (2.1%).
Streptococcus spp. were isolated from blood cultures in 17 cases (35.4%) followed by Staphylococcus spp. (16 cases, 33.3%), Enterococcus (three cases, 6.3%), Pseudomonas aeruginosa (one case, 2.1%), Micrococcus spp. (one case, 2.1%) and 10 cases were culture negative (20.8%). Of the staphylococci, 12 cases were caused by S. aureus (25.0%), of which one case was methicillin-resistant. Four cases were caused by coagulase-negative Staphylococcus. Streptococcal species were the cause of 46% of healthcare-associated infections and 32% of community-acquired infections.
Thirty-three cases had native valve IE (68.7%) and 15 had prosthetic valve IE (31.3%). Infections were most often acquired in the community (72.9%, n=35). Twenty-seven percent of infections were healthcare-associated (n=13) and there were no nosocomial infections.
Five of the 48 cases developed a para-valvular abscess (10.4%) and embolic events were reported in five cases (10.4%). Nine of the 48 cases required valve surgery during their acute admission for IE (18.8%). Two of the nine patients died within six months of having surgery. There were four in-hospital deaths (8.3%) and six-month mortality was 16.7% (n=8).
Discussion
This study found that the incidence of IE has significantly increased in the adult population of Herefordshire between 2010 and 2017. This is in keeping with a trend of increasing incidence reported elsewhere in the UK,5 and worldwide.2,4,7
There are likely to be multiple factors influencing the rising incidence of IE including an increasingly elderly population,8 with increasing numbers of comorbidities, leading to increased contact with the healthcare system and increasing numbers of intra-cardiac devices.2,9
Staphylococcal IE has been typically associated with healthcare associated IE,9,10 however, we found streptococcal species to be the predominant cause of healthcare-associated IE. This may be partly explained by Herefordshire being a predominantly rural population with a low rate of intravenous drug use. There may be other reasons for this finding, but the cohort is small and larger studies are needed to evaluate this further.
Key messages
- Infective endocarditis (IE) is an increasingly common disease associated with significant morbidity and mortality. There are no studies, of which we are aware, that describe morbidity or mortality outcomes associated with IE in the UK
- This study shows that the incidence of IE has significantly increased in the UK population studied from 2010 to 2017, in keeping with global trends. Streptococci were the predominant cause of healthcare-associated IE, in contrast to other areas of the world where staphylococci are the main cause
- There was no significant additional mortality associated with prosthetic valve endocarditis (PVE) or repeat infection with IE, both of which are associated with worse treatment outcomes
- In this study, patients treated with one antibiotic had no significant additional mortality compared with patient’s treated with more than one antibiotic. This finding may reassure clinicians and help to reduce over-prescribing of antibiotics in the treatment of IE amenable to single antibiotic therapy
Conflicts of interest
None declared.
Funding
All authors are employed by the UK National Health Service. The views expressed in this publication are those of the authors and not necessarily those of the UK National Health Service.
Study approval
The study was approved by the Clinical Audit Department at Wye Valley Trust. Formal ethics approval was not required.
References
1. Cahill TJ, Prendergast BD. Infective endocarditis. Lancet 2016;387:882–93. https://doi.org/10.1016/S0140-6736(15)00067-7
2. Slipczuk L, Codolosa JN, Davila CD et al. Infective endocarditis epidemiology over five decades: a systematic review. PLoS One 2013;8:1–17. https://doi.org/10.1371/journal.pone.0082665
3. Bor DH, Woolhandler S, Nardin R, Brusch J, Himmelstein DU. Infective endocarditis in the U.S., 1998–2009: a nationwide study. PLoS One 2013;8:e60033. https://doi.org/10.1371/journal.pone.0060033
4. Pant S, Patel NJ, Deshmukh A et al. Trends in infective endocarditis incidence, microbiology, and valve replacement in the United States from 2000 to 2011. J Am Coll Cardiol 2015;65:2070–6. https://doi.org/10.1016/j.jacc.2015.03.518
5. Dayer MJ, Jones S, Prendergast B, Baddour LM, Lockhart PB, Thornhill MH. An increase in the incidence of infective endocarditis in England since 2008: a secular trend interrupted time series analysis. Lancet 2015;385:1219–28. https://doi.org/10.1016/S0140-6736(14)62007-9
6. Selton-Suty C, Célard M, Le Moing V et al.; AEPEI Study Group. Preeminence of staphylococcus aureus in infective endocarditis: a 1-year population-based survey. Clin Infect Dis 2012;54:1230–9. https://doi.org/10.1093/cid/cis199
7. DeSimone DC, Tleyjeh IM, Correa de Sa DD et al. Temporal trends in infective endocarditis epidemiology from 2007 to 2013 in Olmsted County, MN. Am Heart J 2015;170:830–6. https://doi.org/10.1016/j.ahj.2015.07.007
8. Durante-Mangoni E, Bradley S, Selton-Suty C et al. Current features of infective endocarditis in elderly patients: results of the International Collaboration on Endocarditis Prospective Cohort study. Arch Intern Med 2008;168:2095–103. https://doi.org/10.1001/archinte.168.19.2095
9. Benito N, Miró JM, de Lazzari E et al. Health care-associated native valve endocarditis: importance of non-nosocomial acquisition. Ann Intern Med 2009;150:586–94. https://doi.org/10.7326/0003-4819-150-9-200905050-00004
10. Athan E, Chu VH, Tattevin P et al. Clinical characteristics and outcome of infective endocarditis involving implantable cardiac devices. JAMA 2012;307:1727–35. https://doi.org/10.1001/jama.2012.497
