We describe a case of pneumopericardium following emergency pericardiocentesis in a patient with coronavirus disease 2019 (COVID-19).
Case
A 21-year-old man with a background of trisomy 21, previous cardiac surgery and cardiac resynchronisation therapy-pacemaker (CRT-P) was admitted with a one-week history of pleuritic chest pain, dyspnoea and non-productive cough. Cardiac surgery and CRT-P implantation was undertaken in the Middle East, the precise details of which were unavailable. Admission chest radiograph (figure 1A) revealed features suggestive of coronavirus disease 2019 (COVID-19), which was confirmed on nasopharyngeal swab. Electrocardiography (ECG) revealed sinus tachycardia with biventricular pacing markers. Other than an elevated troponin T (225 ng/L; normal range 0–20 ng/L) and C-reactive protein (CRP) 19 mg/dL, laboratory, investigations were unremarkable.
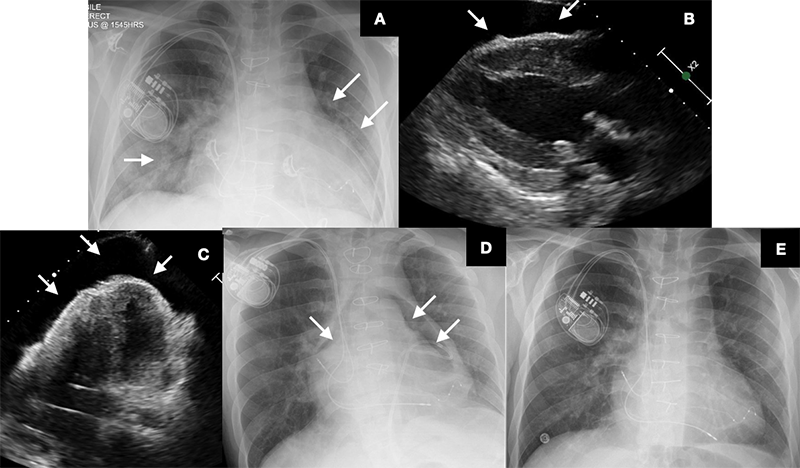
Emergency transthoracic echocardiography (TTE) – undertaken for rapid characterisation of cardiac function and to facilitate exclusion of pertinent differential diagnoses, namely, pulmonary embolism, acute coronary syndrome and myocarditis with associated pericardial effusion – revealed a large circumferential pericardial effusion with features of tamponade (figures 1B and 1C).
Deteriorating haemodynamic status prompted emergency TTE and fluoroscopy-guided pericardiocentesis in the catheterisation laboratory, yielding 750 ml of straw-coloured fluid. Chest radiography undertaken three hours post-pericardiocentesis revealed significant pneumopericardium (figure 1D). Remarkably, the patient remained haemodynamically stable. Given the considerable clinical uncertainty associated with COVID-19 infection, an emergency heart team consensus favoured decompression by syringe aspiration through the pericardial catheter. Air leakage within the pericardial catheter system due to a poorly secured luer lock connection during pericardiocentesis was deemed the likely underlying cause, however, the role played by COVID-19 infection is unclear. Pericardial aspiration yielded 500 ml of air, resulting in near complete resolution of pneumopericardium (figure 1E).
Discussion
Pneumopericardium is a rare complication associated with pericardiocentesis and is often managed conservatively. In this instance, the significant clinical uncertainty associated with COVID-19 prompted an emergency heart team discussion and consensus for decompression by syringe aspiration. This clinical vignette demonstrates how COVID-19 has substantially altered day-to-day clinical practice in emergency settings, and the ever-increasing need for a multi-disciplinary approach, often at short notice.
Conflicts of interest
None declared.
Funding
None.
Patient consent
Written consent was obtained for the publication of this work including all anonymised images and videos.
