Women represented 29% of cardiology trainees and 16% of consultants in the UK in 2021. While the numbers of women in cardiology have increased over the last 20 years, these proportions remain among the lowest in comparison with other medical specialties. This essay aims to explore the contributing factors behind, and plans to reduce, gender disparity in cardiology.
PubMed was searched using keywords such as ‘gender’, ‘inequality’, ‘women’, ‘training’ and ‘cardiology’. Retrieved studies were screened for themes contributing towards, and strategies to overcome, gender inequality within cardiology.
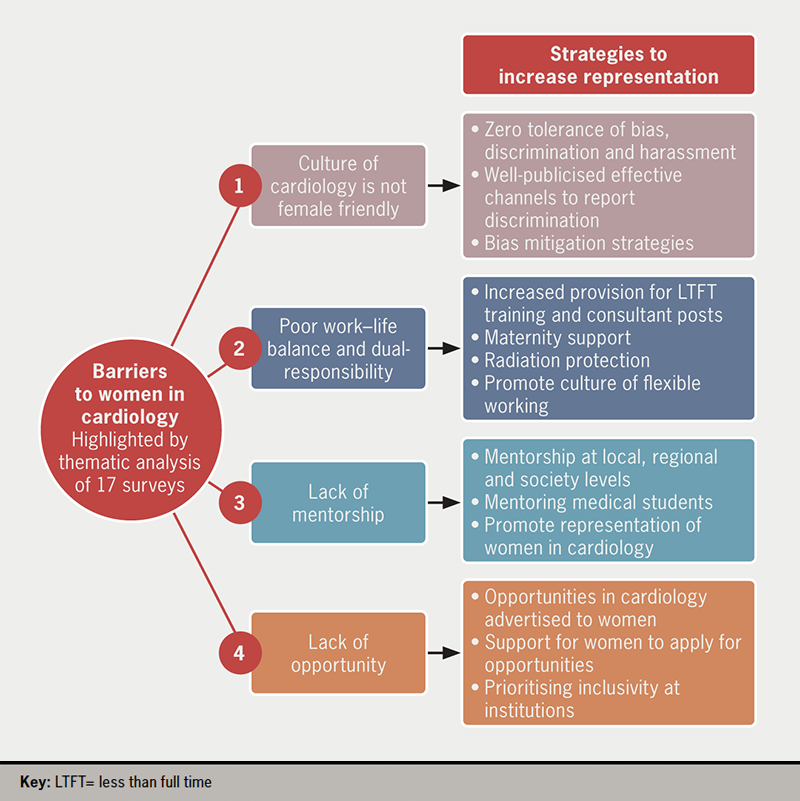
Reasons for gender inequality included poor perceptions of cardiology as a female-friendly specialty, experiences of gender-based discrimination, inflexible working hours, poor work–life balance, and lack of female role models. Recommended resolutions should target these themes; increase opportunities for flexible working hours, enforce a discrimination-free workplace culture, and encourage mentoring relationships between female senior and junior doctors. Improving the experience of the existing female workforce in cardiology will have a knock-on effect on the perceptions of trainees rotating through departments, in addition to initiatives promoting cardiology as a female-friendly specialty.
In conclusion, promoting gender equality within cardiology remains an ongoing challenge. Nationwide efforts to increase retention and improve perceptions should target issues highlighted by the voices of women.
Introduction

In 2021, doctors identifying as women represented 16% of consultants and 29% of cardiology trainees in the UK.1 While the number of women training in cardiology has increased from 17% since 2003,2 cardiology remains an outlier among medical specialties. Women have outnumbered men entering medical school since 1997,3 39% of medical consultants are women, and gender representation in trainees of most other medical specialties is approaching parity.1 It has been proposed that cardiology will ‘catch up’ with other specialties, however, only 27% of female medical graduates declared an interest in cardiology in 2015 compared with 29% of those in 2005 and 2008–9.4
The underrepresentation of women in cardiology is a worldwide issue. Women represented only 15% of cardiology trainees in an analysis reporting on North America, the UK, and Australasia, while women represented 43% overall in all internal medicine programmes.5 This trend is exacerbated in subspecialty selection. In comparison with their colleagues who identify as men, significantly fewer women trainees prefer interventional cardiology (29% vs. 43%) and electrophysiology (6% vs. 17%).6 Women are underrepresented in leadership roles and in academia within cardiology worldwide.7,8 Women represented only 10% of authorship in pivotal efficacy trials of novel cardiovascular drugs approved by the Food and Drug Administration (FDA) between 2008 and 2020,9 and are underrepresented on committees responsible for producing current treatment guidelines in cardiology.10
In 2005, a working group of the (then) Cardiac Society concluded that increasing representation of women in cardiology was required ‘to maintain high standards of cardiological practice and research in this country’.2 Emerging evidence suggests that physician gender impacts patient treatment,11 and that concordance of physician–patient gender can improve patient outcomes in cardiology.12 Representation of women in those leading the design of clinical trials and treatment guidelines should be part of the solution in dissipating systemic bias in medicine that has historically overlooked female patients. Looking to the future, diversity in medicine has been proven to improve innovation.13 Therefore, it remains important to strive for increased representation of women in cardiology.
This essay aims to analyse the contributing factors behind gender disparity in cardiology through a rapid review of the current literature, highlighting barriers provided by the voices of women. This essay will explore strategies to overcome these barriers to inform future recommendations to increase the representation of women in cardiology.
Method
PubMed was searched for studies published between 1 January 1980 and 27 October 2022, using the key words:
- Women OR Female OR Gender OR Sex OR Pregnancy
- Training OR Trainee OR Physician OR Doctor OR Professional OR Medical Student OR Consultant
- Inequality OR Inequity OR Representation OR Gap OR Barriers OR Perception OR Sexism
- Cardiology OR Cardiologist.
There were no restrictions on country, language, or methodology.
Inclusion criteria were study design (surveys, interviews), population (doctors or medical student cohorts including women) and perceptions of cardiology (represented as quantitative data in agreement with pre-defined statements or as free-text quotations). Study characteristics and data on perceptions of barriers to a career in cardiology were extracted. Where available, data stratified by perceptions of women versus men were extracted. A thematic analysis was compiled. An exploration of strategies to overcome the barriers identified by the thematic analysis will be included in the discussion of this essay.
Results
The literature search yielded 1,336 citations, of which 17 studies including 9,335 participants were eligible for inclusion in the thematic analysis. Sixteen studies gathered perceptions using online surveys, while one used one-to-one semi-structured interviews. Studies were conducted between 2007 and 2021, from countries spanning the UK, North America, Latin America, Australia, New Zealand, and Japan. This reflects the length of time of cardiology’s status as an outlier in physician diversity and the international scale of the issue. One study specifically addressed interventional cardiology. Study characteristics are available on file.14-30
Thematic analysis identified four recurring themes that constitute barriers to women in cardiology:
- Culture of cardiology
- Work–life balance and dual-responsibility
- Mentorship
- Lack of opportunity.
Data from included studies on these four themes are presented in a table available on file. Any miscellaneous barriers are presented under ‘Other’. The culture of cardiology and work–life balance/dual-responsibility are identified more frequently as barriers. However, it is difficult to interpret with certainty that these themes are the most pervasive barriers due to the differences in study aims, which may dictate the nature of questions directed towards participants.
Culture of cardiology
Twelve studies reported data on perceptions of the culture of cardiology, including experiences of gender-related bias, discrimination, and sexual harassment. Cardiology was described as a ‘men’s club’, and women were consistently more likely to experience gender-related bias, discrimination, and harassment compared with men. A participant from Banks et al.14 pointed out that effective systems are not in place to report and prevent misogyny in cardiology. Women identified the culture of cardiology as a barrier that makes training more difficult, or as a main deterrent in choosing to pursue cardiology.
Work–life balance and dual-responsibility
Thirteen studies reported data on perceptions of work–life balance and the impact of managing dual-responsibilities in cardiology. Dual-responsibility includes managing maternity, childcare and elderly care responsibilities, which women are more likely to take on than men. Cardiology is a competitive specialty with high expectations of trainees, who often take on out-of-training fellowships and postgraduate degrees to stand out. These factors contribute towards long and unpredictable working hours. From the included studies, women in cardiology were less likely to be married and have children than their male colleagues. If they did have children, they were more likely to have sole child-bearing responsibilities and to have delayed their career progression for children. Women were more likely to identify poor work–life balance as a significant deterrent from pursuing cardiology.
Mentorship
Five studies highlighted the value of mentorship from fellow women or female role models. Cardiology has historically been a male-dominated field. Women stated that seeing female role models in the field assured them that ‘it could be done’. An absence of women trainees in cardiology reinforced the perception that cardiology did not foster a culture acceptable to women.
Lack of opportunity
Seven studies reported data on the lack of opportunity as a barrier to women in cardiology. Women were more likely to agree that they had been excluded from opportunities based on their gender compared with their male colleagues. Women were more likely to agree that they felt excluded from research projects, and more likely to be dissatisfied with support from seniors in academia. In one study, 29% of female respondents identified a lack of opportunity as the main reason for not pursuing interventional cardiology.
Other
Several studies identified barriers such as perceptions of cardiology as not a ‘female-friendly’ specialty, a lack of interest in prioritising diversity when enrolling cardiology fellows, and increased levels of career dissatisfaction in women compared with men in cardiology. Concerns about radiation exposure, particularly with regards to childbearing plans, were the most prominent ‘miscellaneous’ themes.
Discussion
While the numbers of women in cardiology have increased over the past two decades, it is imperative to renew efforts to address the barriers highlighted by the thematic analysis. It is important to recognise that the effect of barriers to women in cardiology is compound. Most studies highlighted work–life balance as a barrier, however, this does not appear such a significant barrier in other specialties where high levels of out-of-hours work are expected, such as obstetrics and gynaecology, where women represent 80% of trainees in the UK as of 2018.31 This suggests that women consider multiple barriers when choosing not to pursue cardiology. Additionally, barriers are often interlinked. A lack of opportunity for women in cardiology may be linked with gender-related bias and discrimination. For example, an analysis of national health research grants in Canada found that gender gaps in grant funding are attributable to less favourable assessments of women as lead investigators, not the quality of their research proposal.32 Therefore, a multi-faceted approach addressing each of the themes raised by women is required to continue making progress. Strategies targeting each of the themes to promote and retain women in cardiology are summarised in figure 1.
Transforming the culture of cardiology
It should not be acceptable that women are experiencing gender-based bias, discrimination, and harassment in cardiology departments in 2022. Improving the culture of cardiology so that it is more receptive to diversity should be a priority. This will improve the experience of cardiology trainees, as well as junior doctors and medical students rotating through cardiology departments prior to specialisation. Implicit bias training for senior committees responsible for selecting trainees,33 and artificial intelligence algorithms to pre-screen applications to overcome bias have been explored with success.34 Banks et al.14 highlighted systemic issues that prevent women from reporting instances of discrimination or harassment. Therefore, it is important to ensure that Trusts have clearly sign-posted, anonymous, and effective channels to report such instances. Support for dealing with discrimination and harassment should be obviously available, particularly as junior doctors rotate between Trusts frequently and may not be familiar with new policies.
A work–life balance for all
Work–life balance should be improved for cardiologists of any gender. In 2020, Health Education England (HEE) rolled out a scheme to enable trainees from any specialty to work less than full time (LTFT) for personal choice.35 It is the joint responsibility of seniors and fellow trainees to destigmatise working LTFT for all genders and for any reason. Currently, only 10% of consultants in cardiology work LTFT.1 Trusts should focus on increasing the number of flexible consultant and training posts to enable women with child-caring responsibilities to pursue competitive careers in cardiology. The COVID-19 pandemic has demonstrated that it is possible for a portion of doctors’ workload to be completed effectively remotely.14 This flexibility should be retained as we move out of the pandemic. The National Health Service (NHS) offers 52 weeks of maternity leave, which is significantly longer than maternity leave offered in the US. However, clear infrastructure to support women returning to work following maternity leave should be implemented in all cardiology departments, including support such as the opportunity for staggered return to work, supervision sessions from seniors to explore worries and establish personal return plans, and provisions for mothers to continue breastfeeding, if required. Women also highlighted exposure to radiation during childbearing years as a barrier to working in cardiology. Cardiology departments should ensure that doctors are aware of their radiation exposure policies. Finally, it is important to promote a culture where women feel empowered to utilise the options of LTFT work, maternity support, and radiation protection without retribution.

Opportunities for all
Creating a culture that prioritises equality, inclusion, and belonging is central to promoting opportunities for women. Departments should focus on reducing implicit bias in appointing roles/awards, and offering support for women applying to opportunities, for example, through mentorship. Opportunities to foster a successful career in cardiology should be available for, or include, women from medical school through to senior doctors.
Representing and supporting success in cardiology
Surveys highlighted a desire for mentorship and increased visibility of women in cardiology to provide individual support as they navigate their careers, and to provide reassurance that it is possible for women to navigate the culture of cardiology, work–life balance, and benefit from opportunity. Mentorship should be promoted at the level of the department, regionally, and by societies. Levels of mentorship are particularly important to promote continuity of contact with rotating UK trainees.
Conclusion
Promoting gender equality within cardiology remains an ongoing challenge. Cumulatively, targeting these themes highlighted by the voices of women should improve the experiences of existing women in cardiology and perceptions of those yet to specialise. We should aspire to a culture of inclusivity and equality, where doctors of all genders can pursue a successful career in cardiology with flexible hours, equal access to opportunity, and support from those around them. Actioning strategies to increase diversity requires honest introspection and commitment to progress by cardiology departments worldwide.
Key messages
- Women remain underrepresented in cardiology, representing 29% of cardiology trainees and 16% of consultants in the UK in 2021
- Barriers to women pursuing a career in cardiology include the culture of cardiology, poor work–life balance, limited mentorship and representation, and a lack of opportunity
- Strategies to promote the representation of women in cardiology must target each of these barriers in concert
Conflicts of interest
None declared.
Funding
None.
Study approval
None required.
Editors’ note
This essay was submitted for, and the winner of, the British Cardiovascular Society Women in Cardiology Medical Student Essay Competition 2022. Supplementary files are available from the author on request.
References
1. Census of consultant physicians and higher specialty trainees in the UK. Working differently in the shadow of COVID-19: the UK 2021 census of consultant, higher specialty trainee and SAS physicians. London: Royal College of Physicians, 2022. Available from: https://www.rcplondon.ac.uk/projects/outputs/working-differently-shadow-covid-19-uk-2021-census-consultant-higher-specialty [accessed 31 October 2022].
2. Timmis AD, Baker C, Banerjee S et al. Women in UK cardiology: report of a Working Group of the British Cardiac Society. Heart 2005;91:283. https://doi.org/10.1136/hrt.2004.047340
3. Moberly T. Number of women entering medical school rises after decade of decline. BMJ 2018;360:k254. https://doi.org/10.1136/bmj.k254
4. Lambert TW, Smith F, Goldacre MJ. Career specialty choices of UK medical graduates of 2015 compared with earlier cohorts: questionnaire surveys. Postgrad Med J 2018;94:191–7. https://doi.org/10.1136/postgradmedj-2017-135309
5. Zaman S, Shaw E, Ellenberger K et al. Representation of women in internal medicine specialties in North America, the United Kingdom, and Australasia: cardiology’s outlier status and the importance of diversity. Am J Cardiol 2022;185:122–8. https://doi.org/10.1016/j.amjcard.2022.08.030
6. Sinclair HC, Joshi A, Allen C et al. Women in cardiology: the British Junior Cardiologists’ Association identifies challenges. Eur Heart J 2019;40:227–31. https://doi.org/10.1093/eurheartj/ehy828
7. Borrelli N, Brida M, Cader A et al. Women leaders in cardiology. Contemporary profile of the WHO European region. Eur Heart J Open 2021;1:oeab008. https://doi.org/10.1093/ehjopen/oeab008
8. Ouyang D, Sing D, Shah S et al. Sex disparities in authorship order of cardiology scientific publications. Circ Cardiovasc Qual Outcomes 2018;11:e005040. https://doi.org/10.1161/CIRCOUTCOMES.118.005040
9. Shahid I, Khan MS, Sohail A et al. Evaluation of representation of women as authors in pivotal trials supporting US Food and Drug Administration approval of novel cardiovascular drugs. JAMA Netw Open 2022;5:E220035. https://doi.org/10.1001/jamanetworkopen.2022.0035
10. Sardar P, Kundu A, Poppas A, Abbott JD. Representation of women in American College of Cardiology/American Heart Association guideline writing committees. J Am Coll Cardiol 2018;72:464–6. https://doi.org/10.1016/j.jacc.2018.06.011
11. Bertakis KD. The influence of gender on the doctor-patient interaction. Patient Educ Couns 2009;76:356–60. https://doi.org/10.1016/j.pec.2009.07.022
12. Lau ES, Hayes SN, Volgman AS, Lindley K, Pepine CJ, Wood MJ. Does patient-physician gender concordance influence patient perceptions or outcomes? J Am Coll Cardiol 2021;77:1135–8. https://doi.org/10.1016/j.jacc.2020.12.031
13. O’Brien KR, Scheffer M, van Nes EH, van der Lee R. How to break the cycle of low workforce diversity: a model for change. PLoS One 2015;10:e0133208. https://doi.org/10.1371/journal.pone.0133208
14. Banks L, Randhawa VK, Caterini J et al. Sex, gender, and equity in cardiovascular medicine, surgery, and science in Canada: challenges, successes, and opportunities for change. CJC Open 2020;2:522. https://doi.org/10.1016/j.cjco.2020.06.016
15. Biondi-Zoccai G, Cerrato E, Peruzzi M et al. An international survey on taking up a career in cardiovascular research: opportunities and biases toward would-be physician-scientists. PLoS One 2015;10:e0131900. https://doi.org/10.1371/journal.pone.0131900
16. Capranzano P, Kunadian V, Mauri J et al. Motivations for and barriers to choosing an interventional cardiology career path: results from the EAPCI Women Committee worldwide survey. EuroIntervention 2016;12:53–9. https://doi.org/10.4244/EIJY15M07_03
17. Crowley AL, Damp J, Sulistio MS et al. Perceptions on diversity in cardiology: a survey of cardiology fellowship training program directors. J Am Heart Assoc 2020;9:e017196. https://doi.org/10.1161/JAHA.120.017196
18. Dettmer S, Wenzel A, Trenkwalder T, Tiefenbacher C, Regitz-Zagrosek V. Gender and career in cardiology – a cross-sectional study. Herz 2021;46:150–7. https://doi.org/10.1007/s00059-021-05027-0
19. Douglas PS, Rzeszut AK, Noel Bairey Merz C et al. Career preferences and perceptions of cardiology among US internal medicine trainees: factors influencing cardiology career choice. JAMA Cardiol 2018;3:682–91. https://doi.org/10.1001/jamacardio.2018.1279
20. Jaijee SK, Kamau-Mitchell C, Mikhail GW, Hendry C. Sexism experienced by consultant cardiologists in the United Kingdom. Heart 2021;107:895–901. https://doi.org/10.1136/heartjnl-2020-317837
21. Kurdi H, Morgan H, Williams C. Women not in cardiology: where are we going wrong? A survey of the perceptions and barriers to training. Br J Cardiol 2020;27:119–23. https://doi.org/10.5837/bjc.2020.030
22. Lewis SJ, Mehta LS, Douglas PS et al. Changes in the professional lives of cardiologists over 2 decades. J Am Coll Cardiol 2017;69:452–62. https://doi.org/10.1016/j.jacc.2016.11.027
23. Raymundo-Martínez GIM, Alanis-Estrada GP, Araiza-Garaygordobil D et al. Gender differences in cardiology professionals: a Latin American survey. Arch Cardiol Mex 2022;92:11. https://doi.org/10.24875/ACM.200001591
24. Ruzycki SM, McFadden C, Jenkins J, Kuriachan V, Keir M. Experiences and impacts of harassment and discrimination among women in cardiac medicine and surgery: a single-center qualitative study. CJC Open 2022;4:676–84. https://doi.org/10.1016/j.cjco.2022.04.003
25. Sarma AA, Nkonde-Price C, Gulati M, Duvernoy CS, Lewis SJ, Wood MJ. Cardiovascular medicine and society: the pregnant cardiologist. J Am Coll Cardiol 2017;69:92–101. https://doi.org/10.1016/j.jacc.2016.09.978
26. Tsukada YT, Tokita M, Kato K et al. Solutions for retention of female cardiologists: from the survey of gender differences in the work and life of cardiologists. Circ J 2009;73:2076–83. https://doi.org/10.1253/circj.CJ-09-0206
27. Castles AV, Burgess S, Robledo K et al. Work-life balance: a comparison of women in cardiology and other specialties. Open Heart 2021;8:e001678. https://doi.org/10.1136/openhrt-2021-001678
28. Wong B, Brennan A, James S et al. A report from the Irish women in cardiology survey, exploring Europe’s largest gender gap in cardiology. Eur Heart J Open 2022;2:oeac033. https://doi.org/10.1093/ehjopen/oeac033
29. Yong CM, Abnousi F, Rzeszut AK et al. Sex differences in the pursuit of interventional cardiology as a subspecialty among cardiovascular fellows-in-training. JACC Cardiovasc Interv 2019;12:219–28. https://doi.org/10.1016/j.jcin.2018.09.036
30. York M, Douglas PS, Damp JB et al. Professional preferences and perceptions of cardiology among internal medicine residents: temporal trends over the past decade. JAMA Cardiol 2022;12:e223485. https://doi.org/10.1001/jamacardio.2022.3485
31. Royal College of Obstetricians and Gynaecologists. O&G Workforce Report 2018. London: RCOG, 2018. Available from: https://www.rcog.org.uk/media/k2xd2qyo/rcog-og-workforce-report-2018.pdf
32. Witteman HO, Hendricks M, Straus S, Tannenbaum C. Are gender gaps due to evaluations of the applicant or the science? A natural experiment at a national funding agency. Lancet 2019;393:531–40. https://doi.org/10.1016/S0140-6736(18)32611-4
33. Gonzaga AMR, Appiah-Pippim J, Onumah CM, Yialamas MA. A framework for inclusive graduate medical education recruitment strategies: meeting the ACGME standard for a diverse and inclusive workforce. Acad Med 2020;95:710–16. https://doi.org/10.1097/ACM.0000000000003073
34. Lau CO, Johnson AB, Nolder AR, King D, Strub GM. A novel algorithm to reduce bias and improve the quality and diversity of residency interviewees. Laryngoscope Investig Otolaryngol 2022;7:1367–75. https://doi.org/10.1002/lio2.908
35. Health Education England. Delivering greater flexibility. Available at: https://www.hee.nhs.uk/our-work/doctors-training/delivering-greater-flexibility [accessed 2 November 2022].
