A 60-year-old male was admitted acutely unwell with prolonged ischaemic chest pain. Seven weeks earlier he had undergone percutaneous coronary intervention (PCI) following admission with an acute coronary syndrome (ACS). Two paclitaxel-eluting stents to his left anterior descending (LAD) artery (2.75 x 32 mm, 2.75 x 16 mm), a 3 x 12 mm Tecnic stent to his obtuse marginal artery and 3.5 x 9 mm Tecnic stent to his proximal circumflex artery were inserted. The patient received intravenous heparin plus abciximab and an excellent angiographic result was achieved (figure 1A). He was discharged home on six months’ dual antiplatelet therapy.
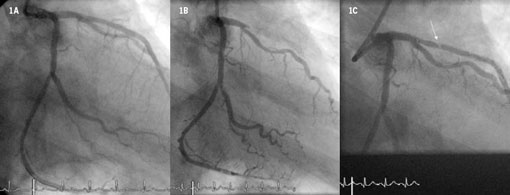
On this admission the electrocardiogram (ECG) showed peaked anterior T waves without ST elevation and urgent coronary angiography was undertaken demonstrating occlusion of the LAD artery distal to the first diagonal branch and within the stented segment. There was also the appearance of thrombus within the obtuse marginal stent (figure 1B). Plain old balloon angioplasty (POBA) restored flow to the LAD artery and revealed a probable tissue prolapse in the proximal part of the stented segment (figure 1C). A further two paclitaxel-eluting stents were deployed with the restoration of TIMI 3 flow. The patient received intravenous heparin and abciximab. He had preserved left ventricular function but an elevated troponin T (10.7 ng/ml).
Subacute stent thrombosis (SAT) remains an uncommon complication of PCI with drug-eluting stents, occurring in fewer than 0.6% of cases within the first 12 months, although it can have major consequences. Resistance to the antiplatelet effects of aspirin and clopidogrel must be considered. The discontinuation of antiplatelet therapy is associated with the development of SAT and this patient later admitted to ‘occasional’ poor compliance.
Conflict of interest
None declared.
