Correspondence from the world of cardiology
Dear Sirs,
Statistical probabilistic reasoning is important in understanding the likelihood of ‘false-positive’ (FP) and ‘false negative’ (FN) results when requesting any diagnostic test. In cohorts with a low prevalence of disease, a significant number of positive results are likely to be FP. Conversely, when the disease has high prevalence, FN results increase.
Identification of patients with suspected coronary artery disease (CAD) relies on clinical history, examination and electrocardiogram (ECG)/laboratory results. The National Institute for Health and Care Excellence (NICE) define angina as “typical” or “atypical” depending on the presence of key features; diagnostic pathways have thus been developed.1 Non-cardiac pain within this classification requires no further cardiac investigation.
Computed tomographic coronary angiography (CTCA) has emerged as a valuable diagnostic tool in the evaluation of CAD with sensitivities, specificities and negative predictive values (NPV) of >90%.2
Thus whilst CTCA enhances diagnosis,3 the incidence/prevalence of the disease in cohorts is also paramount. Young patients, for example, have a low disease prevalence, while the elderly have a high prevalence, which may result in significant FP in the former and significant FN in the latter.
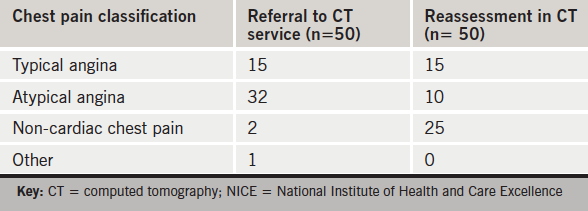
Accurate history taking and pre-test probability classification, however, may influence the FN/FP rates. We reassessed the impact of history-taking in 50 consecutive CTCA referrals for chest pain.
Prior to cardiac CT acquisition, a repeat history was taken by a senior cardiologist/radiologist according to NICE criteria. All 15 patients referred with ‘typical angina’ were confirmed but of the 32 patients referred with ‘atypical angina’, only 10 out of 32 fulfilled the criteria. Three of the 50 patients referred for CTCA had non-cardiac symptoms. Thus 25 of 50 were classified as ‘non-cardiac’ chest pain (see table 1). Of these 25 patients reclassified as ‘non-cardiac’ chest pain, 12 had evidence of CAD, none of which was severe, 11 had no evidence of CAD and two did not proceed to CTCA at all.
Conclusion
The following findings emerged from this study:
1. 50% of patients referred may not have needed any cardiac investigation. Such referrals result in unwarranted exposure to radiation as well as unnecessary further investigations, patient anxiety and effectively amounts to using CT as a screening tool for CAD.4
2. A failure to account for disease prevalence in research studies may have significantly overestimated the non-predictive value of CTCA.
3. Inaccurate history taking appears to be a major cause of misclassification. This may be due to several factors: a) clinician anxiety about missing significant CAD and consciously/subconsciously misclassifying the patient to justify a CTCA; b) patients’ recollection of symptoms may alter over time, or; c) clinicians’ lack of awareness of NICE criteria. We recognise that the history taken at the time of CTCA may have been limited.
4. Accurate history taking may reduce the adverse impact on individual patients, protect NHS resources and ensure the appropriate utility of nationally-defined pathways for chest pain management.
Acknowledgment
This research was supported by the National Institute for Health Research Biomedical Research Unit in Cardiovascular Disease at the University Hospitals Bristol NHS Foundation Trust and the University of Bristol.
Conflict of interest
None declared.
Yasmin Ismail, Consultant Cardiologist
Nathan Manghat, Consultant in Cardiac Radiology
Mark Hamilton, Consultant in Cardiac Radiology
Bristol Royal Infirmary, University Hospitals Bristol NHS Foundation Trust, Upper Maudlin Street, Bristol BS2 8HW
References
1. NICE Guideline CG95: chest pain of recent onset, quick reference guide. NICE March 2010. Available online at https://www.nice.org.uk/guidance/cg95/resources
2. Chow B, Abraham A, Wells G, et al. Diagnostic accuracy and impact of computed tomographic coronary angiography on utilization of invasive coronary angiography. Circ Cardiovasc Imaging 2009; 2:16–23. http://dx.doi.org/10.1161/CIRCIMAGING.108.792572
3. Wallis A, Manghat N, Hamilton M. The role of coronary CT in the assessment and diagnosis of patients with chest pain. Clin Med 2012;12:222–9.
4. Melgies J, Hamilton MC, Manghat NE. Computed tomographic coronary angiography – is it ready as a screening tool for coronary artery disease? Clin Med 2013;13:465–7. http://dx.doi.org/10.7861/clinmedicine.13-5-465
