Troponin testing is the cornerstone diagnostic test for evaluating acute coronary syndromes (ACS). Evidence suggests this test is increasingly being utilised in a less specific fashion. We sought to evaluate the appropriateness of bedside point-of-care (POC) troponin T (TnT) sampling in our hospital.
We examined the case records for 109 consecutive patients who underwent admission troponin testing. We reviewed the clinical presentation, baseline electrocardiogram (ECG) and final diagnoses.
Only 55% of patients presented with actual cardiac chest pain. A troponin-positive result was found in 19.2% of patients (n=21); however, only half of these had a final diagnosis of ACS. The troponin assay was negative in 80.8% of patients (n=88); under one-quarter of these (n=16) underwent further ischaemia assessment. Almost one-third of patients had neither chest pain nor ECG changes (n=35), but still underwent troponin testing. None had a final diagnosis of coronary artery disease.
Troponin assays are requested for patients with a relatively low suspicion of an ACS. A failure to undertake further ischaemia assessment suggests a lack of initial conviction of a cardiac diagnosis. True ACS was diagnosed in less than half of troponin-positive cases. These data support a need for more selective usage.
Introduction
Current evidence suggests there has been a marked proliferation of troponin testing within medical units as the troponin assay has become the cornerstone biomarker in the diagnosis of an acute myocardial infarction (AMI).1,2 Both troponin T (TnT) and troponin I (TnI) are cardio-specific structural subunits and highly sensitive and specific markers of myocardial injury.3,4 Newer generation high-sensitivity troponin (hs-Tn) assays can detect increasingly lower troponin concentrations within an earlier time window of up to three hours.5 Early implementation of first-generation assays were accompanied with poor patient selection; availability of point-of-care (POC) ‘bedside’ sampling may exacerbate this.6
The increasing sensitivity of troponin assays is inevitably associated with an erosion of test sensitivity; more patients may be detected with non-acute coronary syndrome (ACS) related myocardial injury from medical pathology (pulmonary thromboembolism [PTE], sepsis) or chronic cardiac disease (congestive cardiac failure [CCF], cardiac dysrhythmias).7,8
Additionally, the 2012 European Society of Cardiology (ESC)/American College of Cardiology Foundation (ACCF)/American Heart Association (AHA)/World Heart Federation (WHF) task force suggest cardiac biomarker changes alone are insufficient for a final diagnosis of AMI.2 They must be accompanied by evidence of ischaemia (clinical or electrocardiographic) and cardiac imaging suggestive of myocardial damage. Current practice also recommends that a further ischaemia assessment be undertaken in troponin-negative patients to evaluate for unstable angina.
As POC and hs-Tn testing become more popularised, appropriate patient test selection will be essential to reduce false-positive results and inappropriate treatment.
Methods
The medical records of 109 consecutive patients, who had a POC troponin requested from either the emergency department or the medical admissions unit, were prospectively reviewed over a one-month period at a district general hospital. The samples were analysed using a POC TnT assay (Roche Cardiac T-Quantitative test). The local hospital policy recommends troponin sampling on admission and again at 12 hours post-event. Tests are reported as being either negative (<50 ng/ml), intermediate (50–100 ng/ml) or positive (>100 ng/ml). All intermediate and positive results are confirmed by formal laboratory assessment. Both POC and laboratory assays are standardised against the fifth generation Roche Elecsys hs-TnT.
We collected data on three principal areas: the clinical presentation, subsequent relevant investigations and the final diagnosis on discharge. Data were collected on the presenting complaint, electrocardiographic (ECG) changes and coronary risk factors. We noted all subsequent cardiac tests requested (exercise treadmill tests, dobutamine stress echo, computed tomography [CT] coronary angiography, conventional angiography) and non-routine medical tests (D-dimer, CT pulmonary angiography and oesophagogastroduodenoscopy [OGD]). Each patient was followed through until completion of their clinical journey, and the final discharge diagnosis was noted.
Results
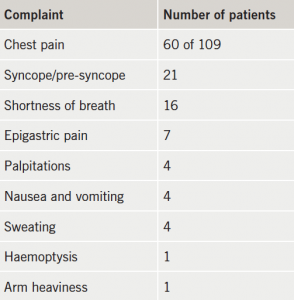
Of the 109 patients in the audit, 46.8% (n=51) were male, and 53.2% (n=58) were female. The mean age of the patients was 67.5 years. Only 55% (n=60) patients tested had a history of cardiac chest pain; while many presented with a combination of non-cardiac symptoms (table 1).
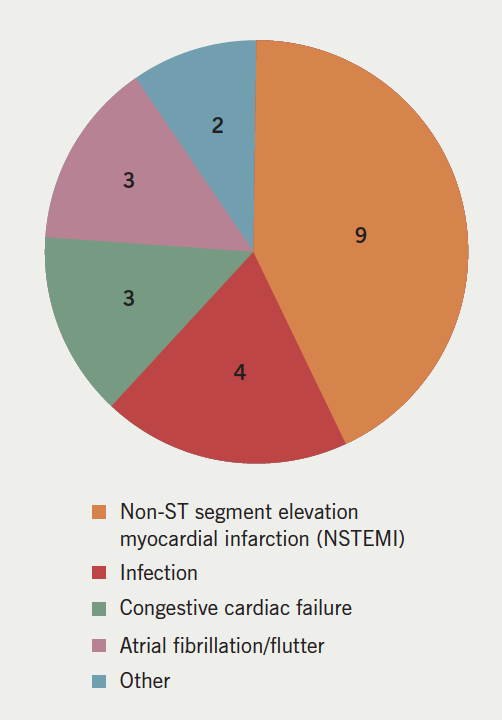
A positive TnT result was found in 19.2% of patients (n=21). Of these, nine were diagnosed with an ACS or coronary artery disease (CAD). In the majority of instances, the troponin rise was attributed to other causes including tachyarrhythmias (n=6), congestive cardiac failure (n=3), and sepsis (n=2) (figure 1).
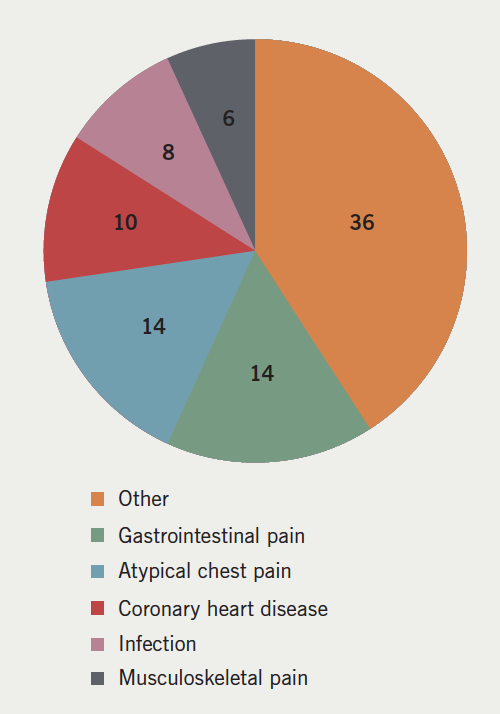
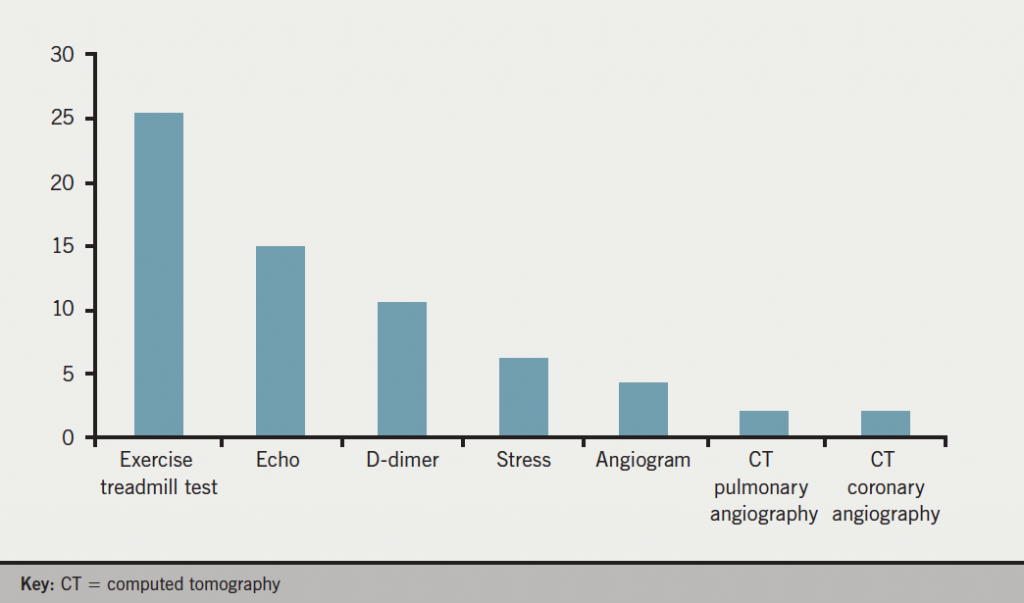
A negative troponin was found in 80.8% (n=88) of patients. A majority of these patients were discharged with no further ischaemia assessment (54%; n=40). A small number were diagnosed with stable angina, but only two referred for coronary revascularisation (final diagnoses shown in figure 2). The exercise tolerance test was the most common investigation following a negative TnT result (most common investigations shown in figure 3).
We identified 35 patients (32.1%), with neither chest pain nor ECG changes (therefore ‘low-risk’), who had a TnT requested, regardless. In all these cases, the TnT assay was negative and none were given a final diagnosis of ACS or coronary heart disease (CHD).
From the study, 93 patients (85%) had a troponin checked at baseline, and in around half of cases (46.8%; n=51) a 12-hour troponin was required to complete the ACS screen. All patients with positive or intermediate bedside troponin results had a laboratory sample obtained to confirm the findings: 100% of patients had a completed TnT screen within the 12-hour assessment period.
Discussion
Higher-sensitivity troponin testing is a powerful tool for the assessment of myocardial infarction. The real world implementation of newer POC ‘bedside’ testing has not been extensively documented.
POC testing was frequently performed in patients with a non-ACS clinical presentation. The majority had no history of cardiac chest pain; instead, non-specific cardiovascular complaints (pre-syncope, palpitations, etc.) triggered a troponin check. Almost one-third of patients had neither chest pain nor ECG changes suggestive of ischaemia. In these cases, there was, unsurprisingly, no final diagnosis of CAD.
In suspected ACS, where the troponin samples are negative, some further form of functional assessment should be performed to evaluate inducible ischaemia.9 In this analysis, a negative TnT test was found in 80.8% of patients (n=88), but an ischaemia assessment was omitted in over half (n=48). This could imply a lack of clinical conviction in suspecting a genuine cardiac event (and, hence, reflect poor patient selection for POC testing). It may also suggest that a negative test is being incorrectly utilised to underwrite safe discharge without follow-up.
A higher detection rate of true AMI could have been anticipated if our assay was used appropriately. From our study, 19.2% of patients were troponin positive; this is higher than the troponin positive rate of 9% from a recent multi-centre analysis by Groarke et al.1 However, in our cohort, the majority of these rises were of non-ACS aetiology (12/21 cases). Elevated cardiac TnT with CCF, PTE and sepsis is associated with increased morbidity, however (with the possible exception of PTE), haphazard troponin sampling is not recommended, as the influence on clinical management is not conclusively established.
In many cases, POC requests are initiated by less experienced ‘front-door’ staff to accelerate patient throughput. However, use of the bedside assay still allows timely and complete sampling at appropriate time intervals.
As patient comorbidity increases and higher-sensitivity assays are more readily available, adequate patient selection must be further emphasised. Indiscriminate testing will yield more non-coronary troponin rises, which can cloud clinical judgement, misguide therapy and incur additional medical expenses from further investigations and prolonged inpatient stay.
Better clinical selection could be engendered by protocolising sample requests, continuous screening or requiring senior authorisation prior to testing. However, these strategies slow turnover time and are impractical for a bedside assay. The role of the clinician is essential to adjudicate testing for more equivocal cases. Our data suggest further education regarding thoughtful patient selection and result interpretation will be essential for effective implementation of the POC, and eventually the hs-Tn assay.
Conflict of interest
None declared.
Sources of support
No external funding.
Key messages
- Point-of-care (POC) troponin T (TnT) testing can be implemented effectively in acute coronary syndromes (ACS)
- TnT assays are requested for patients with a relatively low suspicion of ACS
- A lack of initial conviction is further evidenced by a failure to undertake further ischaemia assessment
- Higher-sensitivity assays yield a greater number of non-coronary troponin rises; a final diagnosis of genuine ACS was made in less than half of troponin-positive cases suggesting non-optimal pre-test selection
- Effective use of the POC and higher-sensitivity TnT assays will require more selective usage and consideration of the clinical context
References
1. Groarke JD, Browne L, Margey R et al. A multicentre analysis of troponin use in clinical practice. Ir J Med Sci 2013;182:185–90. http://dx.doi.org/10.1007/s11845-012-0853-2
2. Thygesen K, Alpert JS, Jaffe AS et al. Third universal definition of myocardial infarction. Circulation 2012;126:2020–35. http://dx.doi.org/10.1161/CIR.0b013e31826e1058
3. Saenger AK. A tale of two biomarkers: the use of troponin and CK-MB in contemporary practice. Clin Lab Sci 2010;23:134–40.
4. Saenger AK, Jaffe AS. The use of biomarkers for the evaluation and treatment of patients with acute coronary syndromes. Med Clin North Am 2007;91:657–81. http://dx.doi.org/10.1016/j.mcna.2007.04.001
5. Apple FS, Collinson PO. Analytical characteristics of high-sensitivity cardiac troponin assays. Clin Chem 2012;58:54–61. http://dx.doi.org/10.1373/clinchem.2011.165795
6. Rajappan K, Murphy E, Amber V et al. Usage of troponin in the real world: a lesson for the introduction of biochemical assays. QJM 2005;98:337–42. http://dx.doi.org/10.1093/qjmed/hci052
7. Gupta S, de Lemos JA. Use and misuse of cardiac troponins in clinical practice. Prog Cardiovasc Dis 2007;50:151–65. http://dx.doi.org/10.1016/j.pcad.2007.01.002
8. Mahajan VS, Jarolim P. How to interpret elevated cardiac troponin levels. Circulation 2011;124:2350–4. http://dx.doi.org/10.1161/CIRCULATIONAHA.111.023697
9. Bertrand ME, Simoons ML, Fox KA. Management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur Heart J 2002;23:1809–40. http://dx.doi.org/10.1053/euhj.2002.3385
