Refractory angina (RA) is an increasingly common, chronic, debilitating condition, which severely reduces quality of life. It can severely impact on physical, social and psychological wellbeing. RA should be considered in patients with known coronary artery disease, who continue to experience frequent angina-like symptoms, despite surgical or percutaneous revascularisation and optimal medical therapy. Objective evidence of reversible ischaemia should also be demonstrated. Treatment is challenging and often not delivered adequately. Management should ideally be provided by a specialist multi-disciplinary team, but national provision of such services is extremely limited. As a result, patients with RA commonly enter a downward spiral of long-term local review, cycling between the outpatient department and Accident and Emergency (A&E). Consequently, a disproportionately high proportion of healthcare resource is consumed in the management of these patients due to high attendance rates in primary and secondary care, unscheduled hospitalisation, prolonged hospital stays, investigations and polypharmacy. This may be improved by the implementation of more appropriate models of care delivery.
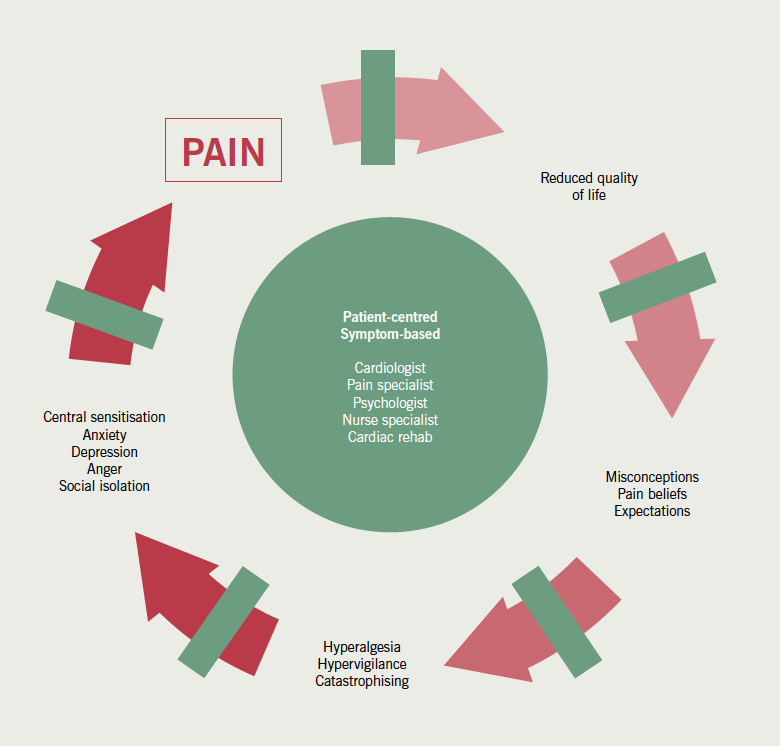
Patel and colleagues (see pages 57–60) from the Bradford Royal Infirmary are to be congratulated on addressing the management of this complex and challenging patient group by developing a practical, effective programme, with particular emphasis on providing psychological support and modulating patients’ psychological responses. This has been achieved through an educational programme, which helps to correct the misconceptions that frequently fuel patients’ anxieties, while simultaneously improving confidence and promoting self-management of their symptoms. This was a single-centre study, inviting participants to attend a four-week course of pragmatic rehabilitation involving both cognitive behavioural therapy and educational sessions. Patients were initially assessed with questionnaires to evaluate mental and physical health, which were repeated at one month and two years post-intervention. The sample size is small, and the authors do not provide information on baseline ischaemic burden or control data for comparison. Furthermore, it is not known whether the intervention reduced the number of emergency attendances to hospital. That said, the study does suggest a consistent improvement of symptoms of depression and an improvement in quality of life, though there was little change in self-reported angina symptoms or glyceryl trinitrate (GTN) use. This interesting finding illustrates the profound impact that cognitive wellbeing can have on perception and tolerability of physical discomfort, and demonstrates this is an important target for intervention. As highlighted by the authors, living with RA often leads to unhelpful psychological responses resulting in anxiety, depression, hyperalgesia, catastrophisation, social isolation and profoundly reduced quality of life. They now demonstrate an approach that may effectively address these issues, which are not often considered in the routine management of patients with angina pectoris, so as to achieve the treatment goals that are of greatest priority to the patient.
Importance of multi-disciplinary approach
This work highlights the importance of a multi-disciplinary approach to the management of RA, which should ideally be delivered by a team comprised of a cardiologist, nurse specialist, pain management specialist and psychologist. Our approach to RA management is summarised in figure 1. These patients are a heterogeneous group whose symptoms can vary from typical angina to an array of other symptoms, which patients often attribute to their heart, and which they perceive to be of sufficient severity and threat to warrant calling the emergency services. Initial detailed clinical assessment of both physical and psychological needs is essential.
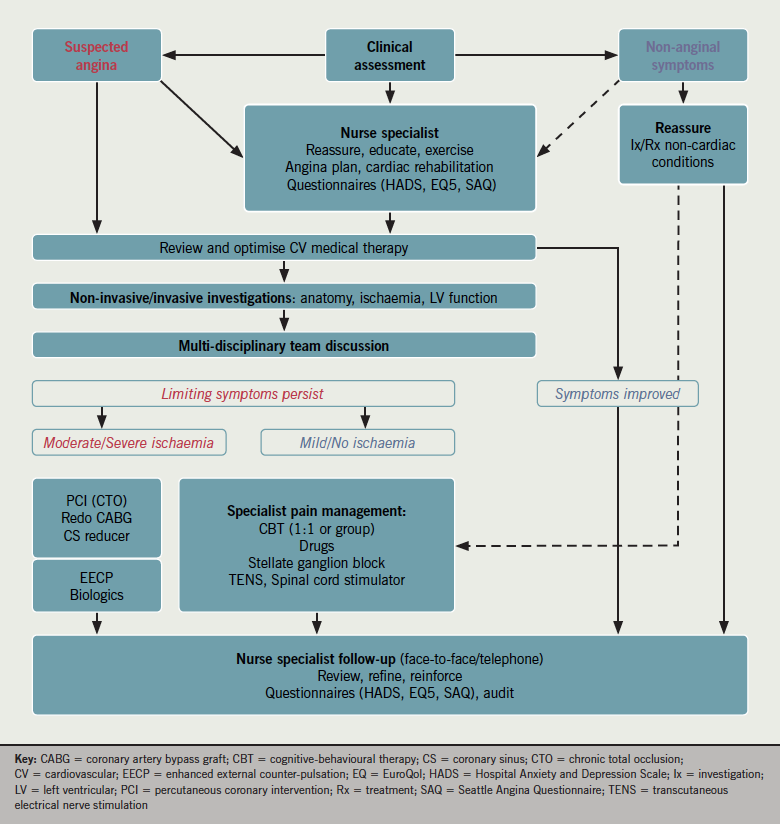
Many patients have non-cardiac pain (e.g. musculoskeletal or gastrointestinal), which should be actively assessed and excluded. In appropriately selected patients, ischaemia testing should be undertaken. It is common for the perceived severity of symptoms to be disproportionate to the burden of ischaemia.1 The central representation and processing of afferent pain signalling, which underlies the perception of pain, resulting from visceral nociceptive stimuli is complex. Neuromodulation can be achieved pharmacologically or via a number of other interventions, but is probably a major mechanism explaining the benefits of pragmatic rehabilitation, a major part of which is to reassure patients that long-term prognosis is often good,2 which is contrary to the understanding of most patients and clinicians. As shown by the Bradford group, management is best delivered via a structured multi-disciplinary approach. Programmes may be offered individually or as a group. In order to try and break the pain cycle that results in angina progressing to RA (figure 2), these types of interventions should ideally be considered early after the initial diagnosis of angina pectoris is established.
In England and Wales, provision of treatment for patients with RA remains extremely limited. It is important for clinicians to be aware that effective treatment options are available for those patients who have previously been considered no-option patients. These are best delivered by specialist multi-disciplinary units, as illustrated by the report from colleagues in Bradford. While these interventions can significantly improve quality of life, the challenge remains to confirm that they also decrease utilisation of healthcare resources and are cost-effective.
Conflict of interest
None declared.
Editors’ note
See also the article by Patel et al. on pages 57–60 of this issue. Also of interest, Tinson et al. on pages 61–4 of this issue. The latter study was accepted for publication after this editorial was commissioned. It also describes benefits in RA patients participating in a CBT programme.
References
1. Foreman RD. Mechanisms of cardiac pain. Ann Rev Physiol 1999;61:143–67. http://dx.doi.org/10.1146/annurev.physiol.61.1.143
2. Henry TD, Satran D, Hodges JS et al. Long-term survival in patients with refractory angina. Eur Heart J 2013;34:2683–8. http://dx.doi.org/10.1093/eurheartj/eht165

