Dear Sirs,
Of the serious complications of gastrointestinal ulcers (bleeding, perforation, obstruction, and sometimes death), non-variceal upper gastrointestinal bleeding (NVUGIB) remains the commonest. These days it is mostly seen in association with the use of antithrombotic drugs (ATDs), particularly low-dose aspirin (75–325 mg/day), given for vascular protection.1
Nicorandil is a vasodilator that acts as a nitrate and K+ATP channel agonist. It is used in many countries worldwide and is often added to ATDs in the management of angina. In light of some case reports, its manufacturer and the medicines advisors and regulatory agencies have issued cautions that it can cause mucosal ulcers, perforation and bleeding, and that these might be worse in users of aspirin.2,3 We therefore investigated the possibility that NVUGIB is more severe in patients using ATDs plus nicorandil than ATDs alone.
In an observational and retrospective analysis, patients presenting to our institution during 2010–2014 with NVUGIB and using ATDs plus nicorandil (n=59) were compared to those using ATDs alone (controls; n=1,056). We compared haemoglobin level, Blatchford UGIB risk score,4 composite endoscopy score (covering erosive and ulcer lesions in the oesophagus, stomach and duodenum),5 need for blood transfusion, length of hospital admission, and 30-day mortality. NVUGIB comprised haematemesis and/or melena in the absence of portal hypertensive gastropathy, oesophageal or gastric varices.1 ATDs included low-dose aspirin, clopidogrel, dipyridamole, warfarin and heparin. The work was approved by the institutional Clinical Governance Team.
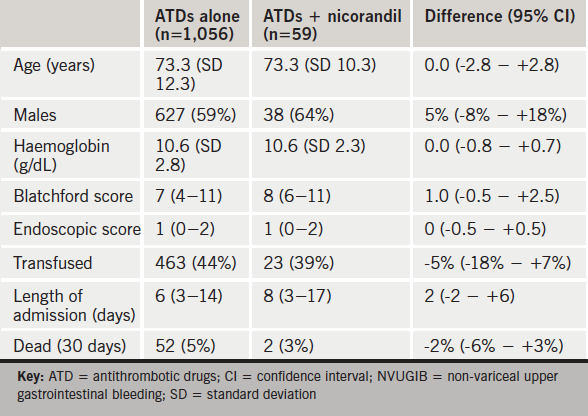
The outcomes of NVUGIB and the characteristics of patients using ATDs alone versus those using ATDs plus nicorandil are shown in table 1. Age and haemoglobin are shown as mean (SD); Blatchford score, endoscopic score and length of admission as median (interquartile range); and binary variables as number (percentage). The final column shows differences between groups (nicorandil minus control) with 95% confidence intervals. All differences were statistically insignificant (P>0.05, Student’s t, Mann-Whitney and Fisher’s exact tests as appropriate). Patients taking ATDs plus nicorandil were well matched demographically with controls taking ATDs alone. The confidence intervals place a modest upper limit on any exacerbation of NVUGIB by nicorandil as manifested by reduced haemoglobin and increased need for transfusion. The intake of nicorandil does not seem to worsen the severity or the outcomes of NVUGIB.
While acknowledging the limitations of observational analysis, these findings do not justify discontinuing nicorandil in patients with angina and presenting with NVUGIB while taking ATDs.
Conflict of interest
None declared.
Ali S Taha
Consultant and Senior Lecturer in Gastroenterology
University Hospital Crosshouse, Kilmarnock, and The School of Medicine, University of Glasgow
(ali.taha1@btinternet.com)
Caroline McCloskey
Specialist Nurse Practitioner
University Hospital Crosshouse, Kilmarnock
Wilson J Angerson
Senior Statistician
The School of Medicine, University of Glasgow
References
1. Taha AS, Kelly C, McCloskey C, et al. Upper gastrointestinal bleeding in hospital inpatients: the role of antithrombotic drugs. Postgrad Med J 2014;90:429–33. http://dx.doi.org/10.1136/postgradmedj-2013-132231
2. Harman C. Nicorandil use restricted over ulceration risk. MIMS 2015. http://www.mims.co.uk/nicorandil-use-restricted-ulceration-risk/cardiovascular-system/article/1373133 (accessed 5 January 2016).
3. Robinson M. Nicorandil is now firmly second line. Prescribing advice for GPs – an NHS prescribing advisers’ blog. http://www.prescriber.org.uk/2015/11/nicorandil-now-firmly-second-line/ (accessed 5 January 2016).
4. Taha AS, Angerson WJ, Knill-Jones RP, et al. Clinical outcome in upper gastrointestinal bleeding complicating low-dose aspirin and antithrombotic therapy. Aliment Pharmacol Ther 2006;24:633–6. http://dx.doi.org/10.1111/j.1365-2036.2006.03017.x
5. Taha AS, McCloskey C, Craigen T, et al. Antithrombotic versus ulcer effects in non-variceal bleeding in users of antithrombotic drugs. Gut 2014;63:A45–A46. http://dx.doi.org/10.1136/gutjnl-2014-307263.93
