A 52-year-old woman, referred for transoesophageal echocardiography, developed acute Takotsubo cardiomyopathy during the examination as a result of emotional distress beforehand. Asymptomatic left ventricular apical ballooning with severe systolic dysfunction within minutes of the emotional trigger was the first sign of any abnormality.
Presentation
A 52-year-old woman with a background of alpha-1-antitrypsin deficiency and severe emphysema underwent transthoracic echocardiography (TTE) that demonstrated an apparent right atrial mass adhering to the inter-atrial septum. She was referred for transoesophageal echo (TOE) to investigate further. Additionally, she had been noted to desaturate on exercise, raising the possibility of intra-cardiac shunting. She was thus also referred for saline-bubble contrast TTE.
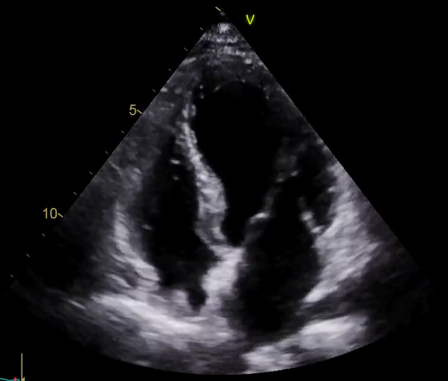
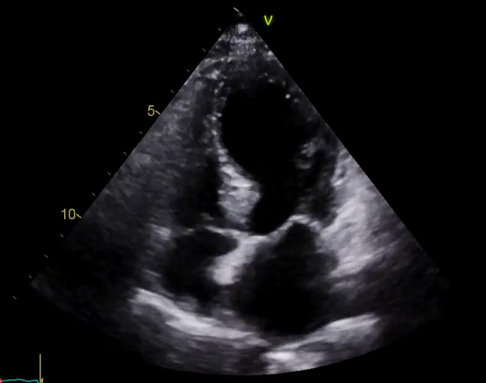
Informed consent for TOE was obtained, but immediately prior to administration of intravenous sedation she became emotionally distressed. After appropriate reassurance she was happy to proceed. Oesophageal intubation was straightforward, and the TOE was well tolerated. The TOE demonstrated that the right atrial mass reported on TTE was a combination of a prominent Eustachian valve and lipomatous hypertrophy of the inter-atrial septum. The inter-atrial septum appeared intact. A saline-bubble contrast TTE immediately after TOE was negative. However, TTE revealed new left ventricular (LV) dysfunction, with global mid-to-apical hypokinesia and preserved basal function, in a typical apical ballooning pattern, with overall severely impaired LV systolic function (figures 1 and 2). She did not describe chest discomfort suggestive of myocardial ischaemia, but did report some minor throat discomfort, which was initially felt to be related to oesophageal intubation.
Differential diagnosis
The considered differential diagnoses were type 1 myocardial ischaemia due to plaque rupture and Takotsubo cardiomyopathy (TC) due to emotional distress.
Investigations
Electrocardiogram (ECG) initially demonstrated sinus rhythm with no acute ischaemic changes. High-sensitivity troponin I was mildly elevated at 23 ng/L (normal <16 ng/L) and rose to 317 ng/L. Deep anterior, lateral and inferior T-wave inversion was evident on the 12-lead ECG at day two. Brain natriuretic peptide was normal at 16 ng/L. Blood tests were otherwise unremarkable including haemoglobin (15.1 g/dL) and estimated glomerular filtration rate (>60 ml/min/1.73 m2).
Management
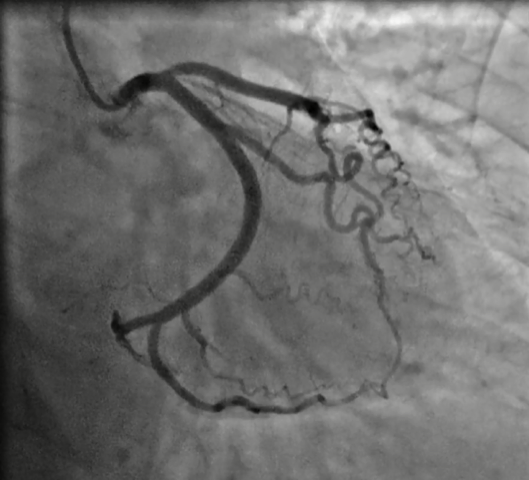
She was initially treated as having had a non-ST elevation myocardial infarction, with dual antiplatelet therapy, a factor Xa inhibitor and appropriate secondary prevention drugs. She was referred for invasive coronary angiography, which was undertaken within seven days, showing only minor ostial left anterior descending artery plaque with nothing to suggest recent instability, and otherwise angiographically smooth coronary arteries (figure 3). The ECG changes had resolved completely by the time of the angiogram. A repeat TTE two months after initial presentation showed full resolution of LV regional and global function.
Discussion
TC, or ‘apical ballooning syndrome’, is probably more aptly termed ‘stress cardiomyopathy’ due to its typical precipitating factors and likely pathophysiology. The majority of patients have either a physical or emotional precipitant. However, some can have no obvious trigger. In a recent registry study of 265 patients diagnosed with TC (95% women; mean age 70 years), 45% of cases were triggered by a physical stressor, 23% by emotional stress and 32% had no obvious trigger.1 Women, and those with advancing age and comorbidities, including chronic lung disease and cancer, seem to be at greatest risk of both developing TC and of having a poor clinical outcome.1,2
The pathophysiology is generally accepted to be related to inappropriate catecholamine excess, resulting in sympathetic overdrive and subsequent detrimental effects on myocardial function.3 In-hospital morbidity and mortality are similar, if not worse, than in patients with acute coronary syndrome,4 with comparable long-term mortality.5
There have been multiple reported iatrogenic triggers for the onset of TC including various drugs,6 and procedures.7,8 Indeed, there has been one other documented case of TOE triggering TC.9 This was in a female patient who, unlike in our case, showed evidence of ST elevation (STE) in the absence of pain. A variety of initial ECG patterns can be present in TC: STE and ST/T-wave changes are the most common presenting abnormalities (39% each; 78% total) while 11% have no initial ECG changes, as in our case.2 Interestingly, in our opinion, the magnitude of troponin rise was not reflective of the degree of acute LV dysfunction witnessed. This phenomenon is well recognised in TC.2
This is only the second case of TOE-induced TC reported in the literature. The progressive regional LV dysfunction was an incidental finding of the planned follow-on saline-bubble contrast study. Our case differs from other reported procedure-induced TC cases in that progressive LV regional dysfunction on TTE was the first sign of any abnormality. This was noted immediately on terminating the TOE and within 10 minutes of onset of emotional disturbance. This is similar to the time of onset of regional wall motion abnormalities reported in animal models of induced myocardial infarction.10
On reflection, the reported throat discomfort post-TOE may have represented myocardial ischaemia rather than just recent oesophageal intubation.
Conclusion
Our case emphasises that common elective procedures, such as TOE, and the potential emotional upset associated with them, can lead to TC.
Key messages
- Takotsubo cardiomyopathy can be a potential complication of any elective procedure, particularly when preceded by emotional distress
- Electrocardiographic (ECG) changes may be minimal or absent acutely in Takotsubo cardiomyopathy, and the degree of left ventricular dysfunction often out-weighs the rise in troponin
- Throat discomfort following a transoesophageal echo (TOE) should not automatically be attributed to oesophageal intubation, particularly in those with typical risk factors for Takotsubo cardiomyopathy, such as those present in our case (female sex, lung disease, emotional distress)
Conflicts of interest
None declared.
Funding
None.
Patient consent
Written consent was obtained from the patient for submission and publication of this manuscript including anonymised images.
References
1. Kim H, Senecal C, Lewis B et al. Natural history and predictors of mortality of patients with takotsubo syndrome. Int J Cardiol 2018;267:22–27. https://doi.org/10.1016/j.ijcard.2018.04.139
2. Dawson DK. Acute stress-induced (takotsubo) cardiomyopathy. Heart 2018;104:96–102. https://doi.org/10.1136/heartjnl-2017-311579
3. Wittstein IS, Thiemann DR, Lima JAC et al. Neurohormonal features of myocardial stunning due to sudden emotional stress. N Engl J Med 2005;352:539–48. https://doi.org/10.1056/NEJMoa043046
4. Templin C, Ghadri JR, Diekmann JL et al. Clinical features and outcomes of takotsubo (stress) cardiomyopathy. N Engl J Med 2015;373:929–38. https://doi.org/10.1056/NEJMoa1406761
5. Tornvall P, Collste O, Ehrenborg E, Järnbert-Petterson H. A case-control study of risk markers and mortality in takotsubo stress cardiomyopathy. J Am Coll Cardiol 2016;67:1931–6. https://doi.org/10.1016/j.jacc.2016.02.029
6. Keskin A, Winkler R, Mark B et al. Tako-tsubo cardiomyopathy after administration of ergometrine following elective caesarean delivery: a case report. J Med Case Reports 2010;4:280. https://doi.org/10.1186/1752-1947-4-280
7. Meydan C, Rimon U, Fefer P, Nissan A, Segev L. Takotsubo cardiomyopathy induced by CT-guided percutaneous biopsy of a paraganglioma. J Vasc Interv Radiol 2016;27:926–8. https://doi.org/10.1016/j.jvir.2016.02.015
8. Patel A, Namn Y, Shah SL, Scherl E, Wan DW. Takotsubo cardiomyopathy after an upper and lower endoscopy: a case report and review of the literature. J Med Case Reports 2019;13:81. https://doi.org/10.1186/s13256-019-2014-y
9. Boukantar M, Cueff C, Brochet E, Vahanian A, Messika-Zeiton D. Transoesophogeal echocardiography: an unusual trigger to Takotsubo cardiomyopathy. Eur Heart J Cardiovasc Imaging 2012;13:445. https://doi.org/10.1093/ejechocard/jer295
10. Gillam LD, Franklin TD, Foale RA et al. The natural history of regional wall motion in the acutely infarcted canine ventricle. J Am Coll Cardiol 1986;7:1325–34. https://doi.org/10.1016/S0735-1097(86)80154-1
