Reducing morbidity and mortality among post-myocardial infarction (MI) patients requires the implementation of effective secondary measures. This survey examined current practice by assessing the view on, and adherence to, National Institute for Health and Clinical Excellence (NICE) guidance on MI secondary prevention in a sample of general practitioners (GPs) and cardiologists. There were 303 respondents from Scotland and England, including at least 10 GPs and one cardiologist from each English Strategic Health Authority. Although drug treatment post-MI generally complied with NICE recommendations, diet and lifestyle aspects were not implemented fully. There appeared to be sub-optimal integration between primary and secondary healthcare providers. Both GPs and cardiologists underestimated the importance of tailoring secondary prevention services to the individual and the role of omega-3 fatty acid treatments (where required) to supplement dietary intake. There is a clear need to improve compliance of healthcare professionals with many of the key priorities for implementation outlined in the NICE guidelines. In addition, patient-centred cardiac rehabilitation services should be standardised and include strategies to improve patient uptake.
Introduction
Myocardial infarction (MI) is a common condition, estimated to affect almost 150,000 people per year in the UK.1 Without effective treatment, the immediate mortality of MI approaches 40% with a further 10% of patients dying in the subsequent year.2 In those who survive the initial post-MI period, an increased risk of death from cardiovascular causes (5% per year) persists indefinitely.2 However, effective secondary prevention measures can significantly reduce this risk.3
An estimated 1.4 million people in the UK have had an MI.4 Reducing morbidity and mortality among this group requires effective secondary prevention measures. In 2007, the National Institute for Health and Clinical Excellence (NICE) published guidelines on a range of secondary prevention interventions proven to improve outcomes after MI.5 NICE identified the key priorities as: regular physical activity; smoking cessation; Mediterranean-style diet, including two tofour portions of oily fish a week (or omega-3 fatty acid supplementation if appropriate); weight loss where indicated; optimisation of drug treatment; and coronary revascularisation where indicated.5
NICE guidelines recommend delivery of these lifestyle changes through cardiac rehabilitation programmes that are accessible and relevant to all post-MI patients.5 However, implementation of such programmes is inconsistent despite the evidence that rehabilitation reduces cardiac mortality by
27% and has other significant morbidity and quality-of-life benefits.3 The National Audit of
Cardiac Rehabilitation (NACR) estimates that only approximately one-third of post-MI patients enter these programmes, partly due to the variable provision of services across the UK.6 Patient groups, such as women, older patients and ethnic minorities, are underrepresented,7 suggesting that specific patient preferences and requirements are unmet.
Drug therapy for post-MI patients is included in the Quality and Outcomes Framework (QOF) for primary care, and broadly follows the NICE guidance.8 However, limited information is available on the specific implementation of lifestyle recommendations. Thus, the survey reported here explored the care of post-MI patients in England and Scotland, focusing particularly on the specific lifestyle and dietary support, including the prescription of omega-3 fatty acid supplements, offered by general practitioners (GPs) and specialist cardiologists.
Materials and methods
The survey was designed to help understand current patterns of care, highlight opportunities for improving the management of post-MI patients and improve medical education initiatives. A comprehensive series of questions covered all aspects of secondary prevention post-MI. Respondents’ demographic data were also collected. The survey used a combination of dichotomous, multiple-choice and Likert scale formats plus free-text comments, and was conducted within the code of conduct of the Market Research Society and the British Healthcare Intelligence Association. An independent steering committee validated the survey.
Respondents were recruited by Doctors.net.uk, the UK’s largest independent network of primaryand secondary-care physicians. An initial pilot survey with seven respondents (five GPs and two cardiologists) identified any potential ambiguities in the questionnaire. The final survey was released and hosted by Doctors.net.uk during July and August 2009. Survey results were independently analysed.
Respondents were recruited by speciality and geographical location to ensure a sample size of at least 250 GPs and 50 secondary-care specialists/specialist cardiologists representing Scotland and each of the 10 English Strategic Health Authorities. To be eligible to participate, respondents needed to be a GP Principal or Salaried GP, or a cardiologist at Specialist Registrar grade or above (with at least three years’ experience). Respondents received a small honorarium for taking part in the survey.
Results
Respondent demographics
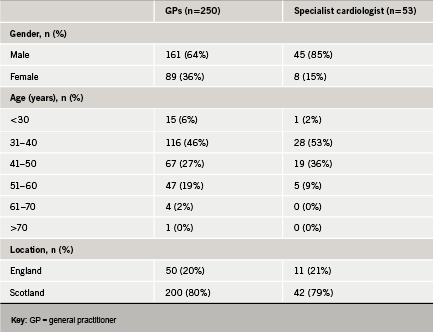
There were a total of 303 respondents (table 1). The majority of GP respondents qualified before 2000, and averaged 1,640 patients on their personal lists. Most of the cardiology specialists were at consultant level or were Specialist Registrars with at least five years’ experience.
General aspects of secondary prevention post-MI
Overall, 81% of GP respondents used the NICE guidelines or Scottish Intercollegiate Guidelines Network (SIGN) guidelines to obtain current information on the appropriate care and rehabilitation of post-MI patients. Most cardiologists (>90%) favoured medical journals or conferences for current information but 74% also used the NICE or SIGN guidelines.
Approximately 90% of respondents used regular consultations or involved other healthcare professionals (HCPs) to motivate post-MI patients to pursue a healthy lifestyle. These consultations were most commonly scheduled monthly. However, there was a perception that patient reluctance to engage with HCPs, together with a lack of support from family and friends, were important barriers to the success of lifestyle interventions.
In terms of tailoring secondary prevention programmes to the individual, gender had a minimal influence (mean scores 2.0–2.7 on a scale of 1 [no influence] to 5 [strongly influenced]). By contrast, age was thought more important, particularly when considering exercise (mean score 3.6). Ethnicity was perceived as having little influence on secondary prevention; however, respondents were more likely to take ethnicity into account when delivering dietary advice (mean score 3.1), addressing health and social needs (mean score 2.7–3.0), and tailoring advice to health beliefs or culture (mean score 3.2–3.5).
Dietary and weight loss advice
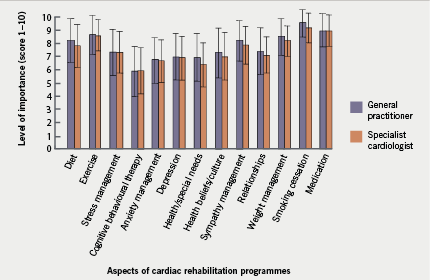
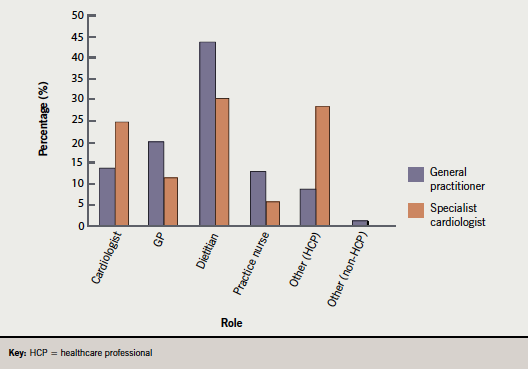
Of the 13 aspects of post-MI secondary prevention, respondents ranked diet as
fifth in importance after smoking cessation, medication, weight management and exercise (figure 1). There was considerable discrepancy among respondents regarding the primary responsibility for providing dietary advice in the immediate post-MI period. Although ‘dietitian’ was the most frequent response (figure 2), over half of GPs and one-third of cardiologists referred fewer than 20% of their patients to a dietitian. The most common reasons for non-referral were: patient reluctance; long waiting lists; and a perception that patients can make dietary changes without assistance.
In total, 98% of respondents personally provided their patients with dietary advice that broadly adhered to NICE guidance. Specifically, more than 80% of respondents advised patients to: reduce consumption of dairy products and replace with unsaturated fats; eat a Mediterranean-style diet containing more bread, fruit and vegetables; increase consumption of oily fish; decrease consumption of salt; and restrict weekly alcohol consumption. Fewer respondents (approximately 50%) advised patients to reduce meat consumption. Less than half felt that their dietary advice was successfully adopted, but only 11% used a food diary to assess patient dietary changes objectively; the majority relied on subjective patient feedback or on indirect measures such as body mass index (BMI) or cholesterol and lipid levels
Despite ranking weight management as the fourth most important component of secondary prevention post-MI, the majority (55%) of respondents provided weight loss counselling to fewer than 60% of obese patients. However, more than 90% advised their patients to take up some form of physical activity.
Smoking cessation
Smoking cessation was considered the most important aspect of secondary prevention. Overall, 99% of respondents assisted with smoking cessation, which correlates with the perceived importance of smoking cessation post-MI. The most common support methods were advice and encouragement, nicotine replacement therapy, and referral to an intensive support service, all of which were used by more than two-thirds of respondents.
Drug therapy
The majority of respondents followed the recommended drug treatment for most post-MI patients (angiotensin-converting enzyme [ACE] inhibitor, aspirin, beta blocker and statin). For patients with left ventricular systolic dysfunction and heart failure, cardiologists were more likely than GPs to prescribe aldosterone antagonists (e.g. eplerenone), in accordance with NICE guidelines. More than half of the cardiologists prescribed aldosterone antagonists for the majority of such patients, compared with just 16% of GPs. Similarly, for patients with ST or non-ST-segment-elevation acute coronary syndrome, cardiologists were more likely than GPs to prescribe clopidogrel in combination with low-dose aspirin.
Despite NICE guidance that omega-3 fatty acid treatment should be considered for patients within three months of an MI who are not achieving the recommended dietary intake of omega-3 fatty acids, more than half of all respondents never prescribed such treatments. Only 11% prescribed them to all or nearly all eligible patients. The primary reason for not prescribing this treatment was adherence to local prescribing recommendations, which do not support use of this treatment despite NICE guidance. However, the perception that patients can consume sufficient omega-3 fatty acids in their diet or can buy products of an adequate strength over-the-counter also contributed. In addition, among doctors who did not prescribe omega-3 fatty acid treatment, there was only mediocre awareness of the clinical benefit (mean score 2.6).
Discussion
The results of this survey indicate that the majority of GPs and cardiology specialists endeavour to follow NICE guidance regarding secondary prevention post-MI. However, these results may be biased towards motivated clinicians with an interest in cardiovascular medicine and may overestimate the application of the NICE guidelines in everyday practice. Furthermore, significant aspects of the NICE guidelines are not being implemented effectively, particularly those relating to diet and lifestyle changes. This may be due to a lack of consistent service provision and confusion over responsibility for initiating rehabilitation measures, suggesting an inadequate integration between primary and secondary healthcare. Similarly, the NACR audit,6 found that a major factor in the poor uptake of cardiac rehabilitation was the failure to deliver a robust patient pathway. This failure is unsurprising as none of the UK cardiac rehabilitation programmes audited by NACR are staffed at the professional level recommended in SIGN guideline 57.9
Our survey also suggests that there is underestimation of the importance of tailoring secondary prevention to the individual – a ‘menu-based’ approach – which may further impact on the uptake and success of rehabilitation programmes. Patients have hugely variable expectations about rehabilitation, and differing motivations for engaging in the services. Health status can also influence uptake of rehabilitation programmes: depression and anxiety are predictors of programme non-attendance.10 Management of these conditions and better support for affected patients within the programmes may improve uptake in some cases. Although not a key point in the NICE guidance, the survey responders perceived management of stress, anxiety and depression as important aspects of secondary prevention (each scoring ≥6.6 out of 10). Patients, therefore, need a comprehensive rehabilitation programme that is appropriate for their individual needs and circumstances. A lack of customisation could be responsible for the reported under-representation of certain patient groups (e.g. women and ethnic minorities) in current rehabilitation programmes.6,7
The importance of dietary change in secondary prevention is particularly under-promoted, despite being a priority in the NICE guidelines. This may arise primarily from confusion over responsibility for providing and assessing dietary advice. Dietitians are underfunded despite evidence of their greater success at effecting dietary change than doctors or other HCPs.11,12 Indeed, NACR reports that 34% of UK cardiac rehabilitation programmes have no dietetic input at all,6 a situation that is likely to worsen in future, with healthcare funding cuts. A perception that dietary advice is not effective in post-MI secondary prevention may also demotivate doctors.
Consistent with the findings of the Myocardial Ischaemia National Audit Project (MINAP),8 this survey demonstrates generally high compliance with NICE guidance on drug therapy for secondary prevention post-MI. In more complex clinical scenarios, cardiologists adhere better to the guidelines than GPs. However, both GPs and cardiologists underrecognise the role of omega-3 fatty acid dietary supplementation. Cost containment through local prescribing restrictions should be resisted to maximise the proven long-term benefits and cost-effectiveness of omega-3 fatty acid treatments in the secondary prevention of MI.13,14 The erroneous belief that dietary intake of omega-3 fatty acids is sufficient, or that over-the-counter formulations are of adequate strength, may also contribute to their lack of use. In reality, patients rarely consume the recommended two-to-four portions of oily fish every week, and over-the-counter preparations typically contain only one-third of the dose of prescription products.15
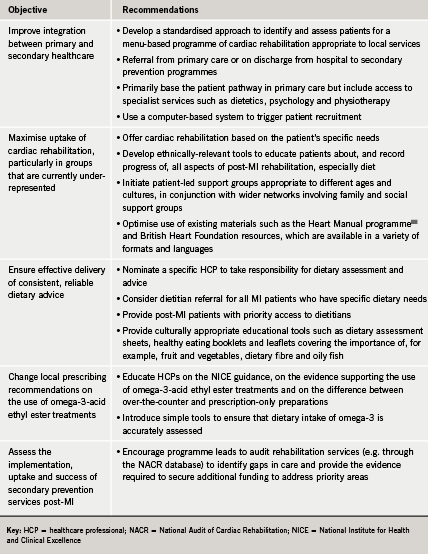
The cost implications of the NICE guidelines for secondary prevention post-MI are considerable,16 but compelling evidence supports these recommendations3 and they should not be ignored. There is a real and urgent need to comply with key priorities for implementation. Recommended approaches to increase compliance include: improve and standardise provision of patient-centred cardiac rehabilitation services (which may require further development of rehabilitation programmes and increasing staff numbers), use of strategies to improve uptake of these services by patients, and improve adherence by HCPs to the guidelines (table 2).
Conclusion
In contrast to other chronic disease management initiatives, which are actively promoted and significantly funded, the potential of dietary and lifestyle interventions to reduce morbidity and mortality in post-MI patients is undervalued despite its huge evidence base. It is imperative to improve compliance with the key priorities for implementation outlined in the NICE guidelines, particularly those relating to dietary and lifestyle changes.
Acknowledgement
This survey was funded via an educational grant from Solvay Healthcare.
Conflict of interest
Pope Woodhead and Associates Ltd recruited the Steering Committee, developed the survey and retained full editorial control of the content, including questionnaire development and data analysis. The Steering Committee validated the questionnaire and developed the recommendations arising from the results. Doctors.net.uk hosted the questionnaire and was responsible for independent recruitment. Solvay Healthcare has not had any editorial input into the survey and the opinions expressed in this publication are not necessarily those of Solvay Healthcare. JH, SL, AB, KG, AM, BB: none declared.
Key messages
- Significant aspects of the National Institute for Health and Clinical Excellence (NICE) guidelines for secondary prevention post-MI are not being implemented effectively
- Only a minority of GPs and cardiologists prescribe omega-3 fatty acid supplements to eligible patients
- While rehabilitation services focus on patient-centred strategies to improve uptake and success, only one-third of post-MI patients currently take part in cardiac rehabilitation programmes
- Better integration between primary and secondary healthcare throughout the UK could improve the provision of a consistent, standardised cardiac rehabilitation service
References
- British Heart Foundation. Incidence of myocardial infarction. British Heart Foundation Statistics Website. Available from: http://www.heartstats.org/datapage.asp?id=1085 [accessed 24 March 2010].
- Law MR, Watt HC, Wald NJ. The underlying risk of death after myocardial infarction in the absence of treatment. Arch Intern Med 2002;162:2405–10.
- Taylor RS, Brown A, Ebrahim S et al. Exercise-based rehabilitation for patients with coronary heart disease: systematic review and meta-analysis of randomized controlled trials. Am J Med 2004;116:682–92.
- British Heart Foundation. Prevalence of myocardial infarction. British Heart Foundation Statistics Website. Available from: http://www.heartstats.org/datapage.asp?id=1119 [accessed 29 March 2010].
- Cooper A, Skinner J, Nherera L et al. Clinical guidelines and evidence review for post myocardial infarction: secondary prevention in primary and secondary care for patients following a myocardial infarction. London: National Collaborating Centre for Primary Care and Royal College of General Practitioners, 2007.
- The National Audit of Cardiac Rehabilitation. Annual statistical report 2009. British Heart Foundation. Available from: http://www.cardiacrehabilitation. org.uk/nacr/index.htm [accessed 29 March 2010].
- Beswick AD, Rees K, Griebsch I et al. Provision, uptake and cost of cardiac rehabilitation programmes: improving services to under-represented groups. Health Technol Assess 2004;8:1–152.
- MINAP Steering Group. How the NHS manages heart attacks. Myocardial Ischaemia National Audit Project. Available from: http://www.rcplondon.ac.uk/ clinical-standards/organisation/ partnership/Documents/minap_public_report_2009.pdf [accessed 29 March 2010].
- Scottish Intercollegiate Guidelines Network. Cardiac rehabilitation: a national clinical guideline. Available from: http:// www.sign.ac.uk/pdf/sign57.pdf [accessed 31 March 2010].
- Lane D, Carroll D, Ring C, Beevers DG, Lip GY. Predictors of attendance at cardiac rehabilitation after myocardial infarction. J Psychosom Res 2001;51:497–501.
- Thompson RL, Summerbell CD, Hooper L et al. Dietary advice given by a dietitian versus other health professional or self-help resources to reduce blood cholesterol. Cochrane Database Syst Rev 2003;(3):CD001366.
- Thompson RL, Summerbell CD, Hooper L et al. Relative efficacy of differential methods of dietary advice: a systematic review. Am J Clin Nutr 2003;77:1052S–1057S.
- Gruppo Italiano per lo Studio della Sopravvivenza nell’Infarto miocardico. Dietary supplementation with n-3 polyunsaturated fatty acids and vitamin E after myocardial infarction: results of the GISSI-Prevenzione trial. Lancet 1999;354:447–55.
- Quilici S, Martin M, McGuire A, Zoellner Y. A cost-effectiveness analysis of n-3 PUFA (Omacor) treatment in post-MI patients. Int J Clin Pract 2006;60:922–32.
- Shuman J. Helping patients sort through the conundrum of dietary supplements. Primary Issues 2009;11:2–6.
- National Institute for Health and Clinical Excellence. MI: secondary prevention. Costing report: Implementing NICE guidance. London: NICE, 2007.
- The Heart Manual. Post-Myocardial Infarction (MI) Edition. Edinburgh: NHS Lothian, 2008.
