In primary care, the significant burden of heart failure is exacerbated by problematic, inaccurate diagnosis that may produce inefficient triaging of patients to echocardiography. UK guidelines recommend using natriuretic peptides in the diagnostic pathway. The costs and consequences of providing a definitive diagnosis for symptomatic heart failure have not been established for peptide testing in primary care. We provide a cost-consequence analysis to compare alternative diagnostic strategies for symptomatic heart failure patients presenting to their GP.
Health economic evaluation using decision-tree modelling taking a cohort of patients presenting in primary care with symptomatic heart failure to a definitive diagnosis was performed. The model compared a diagnostic strategy using electrocardiograms (ECGs) interpreted by consultants with the use of B-type natriuretic peptide (BNP) assays. The base-case used data from the UK Natriuretic Peptide (UKNP) study, which used a ‘point-of-care’ assay. Two alternative scenarios were modelled reflecting data from key studies, as was sensitivity to costs. The model demonstrates that, for the base-case scenario, an initial diagnostic strategy of BNP is superior to ECG in terms of diagnosis of symptomatic heart failure in patients presenting in primary care, despite slightly more initial false negatives and a marginally higher cost. The alternative scenarios and sensitivity analyses show that the results are very sensitive to test accuracies and costs, but that, under plausible assumptions, BNP could be both cheaper and clinically superior.
The model suggests that, despite parameter uncertainty, the adoption of BNP in primary care is likely to be clinically preferable, be more satisfactory for most patients, and lead to fewer unnecessary echocardiography referrals, at a very small increase in cost.
Introduction
Heart failure is a serious syndrome accounting for around 4% of UK general practitioner (GP) consultations in patients over 45 years.1 Diagnosis is complex with frequent co-existing symptoms; misdiagnosis may lead to inappropriate treatment and inefficient use of scarce healthcare resources.2
The National Institute for Health and Clinical Excellence (NICE) guidelines for chronic heart failure state that the 12-lead electrocardiogram (ECG) and/or natriuretic peptides tests (where available) may be used to help exclude heart failure.3 Abnormal ECGs are usually observed in heart failure cases, although in one study, around 20% of patients with heart failure had normal ECGs.4Subsequently, echocardiography is recommended to consolidate the diagnosis and provide further diagnostic information. Echocardiography, however, is costly, and it requires skill in interpretation. There are also significant accessibility problems in many regions, with patients having to wait several months for echocardiography in many cases.5
B-type natriuretic peptide (BNP) is a neurohormone produced in the heart exacerbated by vascular wall stress, with high blood plasma concentrations of BNP strongly suggestive of heart failure.6‑8There are two quite distinct BNP test technologies that may be available to the GP when ordering a BNP test: automated immunoassays performed on standard clinical laboratory equipment – ‘laboratory-assayed BNP’; and rapid fluorescence immunoassays test kits – ‘point-of-care’ BNP. Point-of-care BNP tests produce test results in around 15 minutes. The trade off is poorer test-to-test precision, and higher costs, than laboratory assays.
Few studies have directly compared BNP with ECG in the primary care setting. A review published in 2006 stated that there was no diagnostic evidence to justify the use of natriuretic peptides over ECG.9 However, several studies since this review have provided supporting evidence for natriuretic peptides to refute symptomatic heart failure.
A pioneering trial by Cowie and colleagues in 1997 studied natriuretic peptide concentrations in 122 symptomatic patients referred from primary care to a rapid access cardiology clinic for diagnosis.10 Laboratory-assayed BNP was concluded to be a useful heart failure rule-out test in this study where the cardiologists exercised tight control on the final definition of heart failure. In 2005, the multi-centre UK Natriuretic Peptide (UKNP) study compared diagnostic accuracies of point-of-care BNP testing with those of ECG to refute heart failure in 306 symptomatic patients referred to a secondary care clinic after being triaged by their GP from primary care.4 The report further strengthened the case for BNP as a rule-out test with negative predictive value (NPV) and positive predictive value (PPV) of 0.87 and 0.59, respectively.
A health technology assessment (HTA) report from NHS Quality Improvement Scotland (QIS) provided a comprehensive evaluation of BNP and ECG testing using the pooled accuracies from 18 studies for both point-of-care BNP and laboratory-assayed BNP.5 Support for BNP as a rule-out test was further strengthened by Fuat et al. in 2006, which used both ‘point-of-care’ BNP and laboratory N-terminal prohormone BNP (NT-proBNP) assays in a population-based study to detect left ventricular systolic dysfunction (LVSD).11 The study showed slightly better performance from a laboratory NT-proBNP assay than a ‘point-of-care’ BNP test, with the NPV and PPV for point-of-care BNP being 0.88 and 0.49, respectively, at their defined optimal decision cut-point of 40 pg/ml. This decision cut-off point differs from the manufacturer’s recommended cut-off and previously published cut-off points of 100 pg/ml.4,5
There have been few economic evaluations of BNP. The HTA report from NHS QIS included an economic analysis, which suggested that if GPs’ decisions, made without the assistance of BNP testing, to refer patients for echocardiography had a specificity better than 50%, the addition of BNP would add to cost, but that the cost of £500 per additional true-positive detected might be acceptable.5 This report, however, does not present an explicit underlying economic model and contains a number of flaws. For example, it uses the number of true-positive cases detected alone as the diagnostic effectiveness measure and the interpretation of its results depend upon how much the decision makers would be willing to pay for each additional true-positive result – a parameter unlikely to be known. Moreover, the analysis does not take all patient groups to a definitive diagnosis: real-life strategies would incur subsequent costs, when patients who, for example, had false-negative test results returned to primary care with unresolved symptoms requiring further investigation.
Nielsen et al. examined costs of BNP screening at-risk patients in Glasgow and concluded that BNP testing could reduce the number, hence costs, of echocardiograms in a general population below 75 years old.12 Sim et al., in a small study in Wales concluded that using BNP could reduce costs without compromising diagnostic accuracy.13 Heidenreich et al. modelled cost-effectiveness of screening breathless patients for heart failure presenting at the emergency room in the US and estimated that, while BNP added to total cost, the incremental cost per Quality-Adjusted-Life-Year (QALY) ratio of $22,300 per QALY was acceptable in a male population.14
We provide a UK relevant study that uses a cost-consequences analysis approach to compare alternative diagnostic strategies for symptomatic heart failure patients in a primary care setting.15 We use a model that takes all patients to the point of a definitive diagnosis of heart failure or not.
Methods
Designing the economic model
Our model uses diagnostic pathways consistent with the NICE guidelines.3 We compare:
- Consultant-read ECG: ECGs are taken by the GP and sent for cardiologist interpretation.
- BNP: patients receive BNP as a rule-out test. Patients with positive BNP tests are additionally given an ECG interpreted by a consultant cardiologist.
We assume that all test positive patients receive hospital-based echocardiography for confirmation of underlying cardiac dysfunction and that, on average, patients wait two months for echocardiography.5 Meanwhile, they are prescribed diuretics to relieve congestive symptoms, as recommended.3 We also assume that false-negative patients are initially untreated and will re-present to their GP, receive a further ECG, and be finally sent for confirmatory echocardiogram.
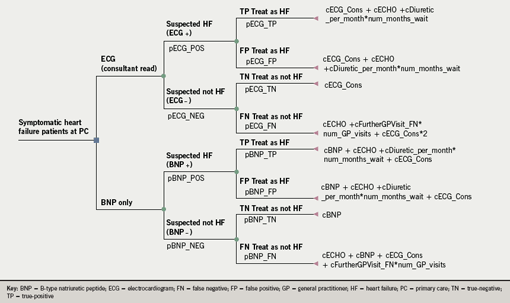
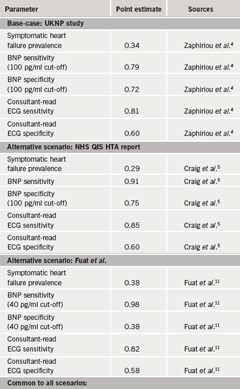
The decision-tree model (figure 1) was constructed using TreeAge® decision analysis software.16 Each strategy branches horizontally with the four possible true- and false-positive/negative test results (TP, FP, TN, FN). The base-case model was populated with parameters obtained from the UKNP study and costs obtained from relevant sources, as summarised in table 1. Path probabilities were calculated using Bayes revision formulae, using point estimates for the test accuracy and disease prevalence variables.17
Data on prevalence, and test sensitivities and specificities
In our base-case model, we use the evidence from the UKNP multi-centre trial, which provides the most substantive and realistic evidence of relevance to UK primary care practice. The presenting population had an average age of 74 years and 58% were females with 6% of patients recorded as New York Heart Association (NYHA) Class I; 63.1% NYHA Class II (symptomatically mild heart failure); 25.5% NYHA Class III (symptomatically moderate heart failure) and 4.6% NYHA Class IV (symptomatically severe heart failure).4 Over half of the patients had associated hypertension. All patients referred were examined by a cardiologist who recorded their medical history as well as ECG, radiograph and echocardiogram test results. BNP and standard blood chemistry tests were also performed on venous blood. Patients with a previously documented history of heart failure were excluded.4 The trial showed a symptomatic heart failure prevalence of 34%.4 The diagnostic accuracies for BNP and ECG testing in the UKNP study are shown in table 1 for a cut-off point of 100 pg/ml. Cardiologist-interpreted ECGs were deemed test positive if there was any abnormality observed.4
The test specificity and sensitivity are uncertain parameters dependent upon various factors such as skill of interpretation, type of assay used, the disease prevalence and the population studied. To indicate possible variability we modelled two alternative scenarios using data from the Scottish HTA report and from the 2006 study by Fuat et al.5,11 Diagnostic accuracy values are summarised in table 1. The prevalence in the HTA study was assumed to be the same as that in the study by Cowie et al., i.e. 29%, while Fuat et al. used point-of-care BNP in a population study with a prevalence of symptomatic heart failure due to LVSD of 38%.10,11 In the latter publication, the optimal BNP cut-off was determined to be 40 pg/mL, since it gave the highest NPV.
Cost estimates
An NHS cost perspective was adopted with all costs, summarised in table 1, expressed in UK pounds sterling (2004 prices). We estimated that each GP consultation costs £38.40, based on 20 minutes of GP time at a unit cost per minute of £1.92, inclusive of direct care staff costs and excluding qualification costs.18 The total cost of ECGs is estimated at £30.70, based on 10 minutes of GP time plus 10 minutes of consultant time at a unit cost of £1.15 per minute, excluding qualification costs.18 The base cost of both point-of-care and immunoassay BNP assays is £15.00.5,19 The total cost of an immunoassay BNP test (includes reagents, transport, laboratory staff time, quantitative analysis and calibration, and communication with patient) is £21.00.5 The total costs of point-of-care assay have been reported between £15.00–£30.00 and we make the assumption that the total average cost of BNP point-of-care tests is also £21.00. The cost of echocardiography was obtained from the average 2004 NHS Reference Cost of £51.00 and monthly cost of diuretic treatment per positive patient is £1.70, (based on 1 mg bumetanide which is comparable to 40 mg furosemide at £1.00).20,21
Results

The results of the base-case model are presented in table 2 for a 1,000 patient cohort in terms of total resource usage, average costs per patient, and consequences in terms of true and false positives referred to echocardiography and initial and delayed correct diagnoses. Additionally, we show results for BNP and ECG in two alternative scenarios.
For the base-case, the average cost per patient is £70.28 and £70.90 for ECG and BNP, respectively. The average incremental cost for BNP of £0.62 is offset by the higher proportion of definitive diagnoses and heart failure patients correctly diagnosed after initial presentation as well as fewer total echocardiography referrals that BNP offers. Correspondingly, there is a marginally higher proportion of patients who are correctly diagnosed only after a further symptomatic period that leads them to revisit their GP.
Model sensitivity to BNP test type and diagnostic test accuracies
We modelled two alternative scenarios. Using the HTA QIS data, table 2 shows that, the average cost per patient for BNP would then be cheaper by £3.75 relative to ECG. Clearly, BNP becomes the cheapest option, involving both considerably fewer echocardiography referrals and fewer GP consultations. In this scenario, since BNP is preferable in terms of all consequences, and given that it costs less, it is the ‘dominant’ strategy.15
When the data from Fuat and colleagues are used in our model to detect LVSD, BNP costs £22.44 per patient. This reflects the increased costs associated with managing the higher proportion of false-positive patients, combined with fewer true-negative test results.
Base-case model sensitivity to key costs
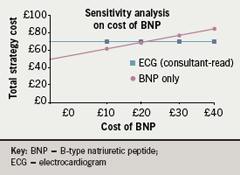
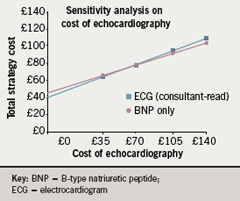
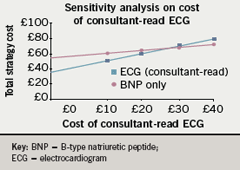
Figure 2 shows that, all other factors unchanged, BNP testing will be cost saving when the total BNP test cost falls to below £20.40, only £0.60 below the base-case value. Figure 3 shows that BNP is cost-saving if the cost of echocardiography rises above £58.80. Similarly the choice is sensitive to ECG cost, shown in figure 4. When the cost of ECGs rises slightly above the base-case value of £31.00, BNP is cost-saving.
Discussion
This study adopted an economic model to help identify the costs and consequences of diagnostic strategies to identify referrals for new, symptomatic heart failure patients presenting in primary care.
Our base-case model used data from the multi-centre UKNP study; the most relevant study of primary care BNP diagnostic accuracy. We assumed that all BNP positive patients received confirmatory ECG and echocardiography tests, in accordance with good clinical practice. The results indicate that, in taking all patient groups to a definitive diagnosis, BNP has the advantage of more efficiently triaging patients to echocardiography with more initial positive test results than ECG testing, and that the benefits occur at a very small increased total cost of £0.62 per patient. This result holds despite the relatively low sensitivity and specificity of the point-of-care assay used. Scenario analysis suggests that the case for BNP adoption is likely to be significantly strengthened if more accurate, possibly laboratory-assayed BNP tests, are used. When BNP accuracies from point-of-care and laboratory assays were combined, as in the Scottish HTA report, BNP was shown to dominate ECGs, i.e. it was cheaper and superior throughout all consequences. On the other hand if higher sensitivity is traded for lower specificity, as in the Fuat study, costs are considerably increased and BNP looks much less attractive. All scenarios were sensitive to the relative costs of the tests and any significant cost variations of the assays across the UK could affect the attractiveness of testing to primary care trusts (PCTs).
We used best available evidence to populate an economic model that, for the first time, has taken all symptomatic heart failure patients to a definitive diagnosis. Our model is, of course, subject to some caveats. First, the model population is mainly moderate-to-severe symptomatic patients and the results may not be generalisable to very low prevalence situations, such as patients with very mild symptomatic heart failure or population screening. Also, as is frequently the case, we assume that echocardiography is a gold standard, 100% sensitive and specific, while in practice it is subject to variable technical skill. Finally, there is uncertainty in the parameter values and a deterministic modelling approach has been used here because of its simplicity in presentation and interpretation. Probabilistic sensitivity analysis could be undertaken to better characterise the overall decision uncertainty and as a basis for a Value of Information analysis to inform further research.22
Misdiagnosis of heart failure can lead to inappropriate patient management. It is well recognised that the ideal case of referring all suspected cases to echocardiography would overwhelm healthcare services with the substantial demand, and this is reflected in UK NICE guidance recommending ECG and/or natriuretic peptide tests to help exclude heart failure. We have shown that it may be preferable for GPs to take the choice of laboratory BNP assays over point-of-care, not only in terms of the increased quality control and technical performance that the former tests offer, but also in terms of costs and consequences, a conclusion shared by Fuat et al.11
Further research studying the use of BNP in an everyday, ordinary NHS primary care environment, taking patients to a definitive diagnosis, would be beneficial in defining optimal decision cut-points and to optimise test accuracy and practicality within a real-world setting. A study of point-of-care versus laboratory-assay BNP testing within that patient population would provide useful comparative evidence.
Conclusions
This work has demonstrated the usefulness of a cost-consequences approach built on a simple economic model that takes a cohort of symptomatic heart failure patients to a definitive diagnosis. The base-case model indicates that, while there remains significant uncertainty about a number of key parameters, the adoption of BNP in primary care is likely to lead to fewer delayed diagnoses for symptomatic patients at a very small increased cost relative to ECG. In the cases where more accurate assays are used or the relative costs of BNP and ECG testing changes marginally, the case for BNP adoption is significantly strengthened.
Conflict of interest
MAS was funded through the MATCH Programme (EPSRC Grant GR/S29874/01 and support from a number of commercial companies including Bayer HealthCare LLC, Diagnostics Division, Tarrytown, NY, USA). The Health Economics Rsearch Group receives a programme grant from the Department of Health’s Policy Research Programme. The views expressed in the article are entirely those of the authors and should not be attributed to other parties.
Editors’ note
An editorial by Ahmet Fuat on this subject is published on pages 179–80.
Key messages
- Heart failure is associated with a significant burden of care that is exacerbated by problematic and inaccurate diagnosis that may lead to inefficient triaging of patients to echocardiography; a scarce and costly resource
- Natriuretic peptides are known to be useful in ruling-out heart failure and are recommended in the diagnostic pathways of national guidelines, although there is a lack of health economic evidence
- The costs and consequences of taking patients to a definitive diagnosis have not been established for the adoption of peptide testing in primary care to improve a rule-out diagnosis for symptomatic heart failure
- This paper provides an analysis that takes patients to a definitive diagnosis and helps to fill this evidence gap for the application of this important test in the primary care setting
References
- Mortality and survival from heart failure. 2005, London Heart Failure Study, Office for National Statistics. Available from: http://www.heartstats.org
- Dickstein K. Diagnosis and assessment of the heart failure patient: the cornerstone of effective management. Eur J Heart Fail 2005;7:303–08.
- NICE. CG5 Chronic heart failure: Management of chronic heart failure in adults in primary and secondary care – Full guideline. London: National Institute for Health and Clinical Excellence. Available from: http://www.nice.org.uk/page.aspx?o= CG005fullguideline
- Zaphiriou A, Robb S, Murray-Thomas T et al. The diagnostic accuracy of plasma BNP and NT-proBNP in patients referred from primary care with suspected heart failure: results of the UK natriuretic peptide study. Eur J Heart Fail 2005;7:537–41.
- Craig J, Bradbury I, Cummins E, Downie S, Foster L, Stout A. Health Technology Assessment Report 6: The use of B-type natriuretic peptides (BNP and NT-proBNP) in the investigation of patients with suspected heart failure. NHS Quality Improvement Scotland, 2005.
- Cowie MR, Mendez GF. BNP and congestive heart failure. Prog Cardiovasc Dis 2002;44:293–321.
- Sagnella GA. Measurement and importance of plasma brain natriuretic peptide and related peptides. Ann Clin Biochem 2001;38:83–93.
- Iwanaga Y, Nishi I, Furuichi S et al. B-type natriuretic peptide strongly reflects diastolic wall stress in patients with chronic heart failure: comparison between systolic and diastolic heart failure. J Am Coll Cardiol 2006;47:742–8.
- Davenport C, Cheng EY, Kwok YT et al. Assessing the diagnostic test accuracy of natriuretic peptides and ECG in the diagnosis of left ventricular systolic dysfunction: a systematic review and meta-analysis. Br J Gen Pract 2006;56:48–56.
- Cowie MR, Struthers AD, Wood DA et al. Value of natriuretic peptides in assessment of patients with possible new heart failure in primary care. Lancet 1997;350:1349–53.
- Fuat A, Murphy JJ, Hungin AP et al. The diagnostic accuracy and utility of a B-type natriuretic peptide test in a community population of patients with suspected heart failure. Br J Gen Pract 2006;56:323–4.
- Nielsen OW, McDonagh TA, Robb SD, Dargie HJ. Retrospective analysis of the cost-effectiveness of using plasma brain natriuretic peptide in screening for left ventricular systolic dysfunction in the general population. J Am Coll Cardiol 2003;41:113–20.
- Sim V, Hampton D, Phillips C et al. The use of brain natriuretic peptide as a screening test for left ventricular systolic dysfunction – cost-effectiveness in relation to open access echocardiography. Fam Pract 2003;20:570–4.
- Heidenreich PA, Gubens MA, Fonarow GC, Konstam MA, Stevenson LW, Shekelle PG. Cost-effectiveness of screening with B-type natriuretic peptide to identify patients with reduced left ventricular ejection fraction. J Am Coll Cardiol 2004;43:1019–26.
- Drummond MF, Sculpher MJ, Torrance GW, O’Brien BJ, Stoddart GL. Methods for the Economic Evaluation of Health Care Programmes. 3rd Ed. Oxford: Oxford University Press, 2005.
- TreeAge Software Inc., MA USA. TreeAge Pro Suite. 2005.
- Bullard F. A Brief Introduction to Bayesian Statistics. 2001. Available from: http://courses.ncssm.edu/math/TALKS/PDFS/BullardNCTM2001.pdf
- Curtis L, Netten A. Unit costs of Health and Social Care 2004. University of Kent 2004.
- Biosite Ltd. BNP Triage Kit panel cost. Private Communication, October 2006.
- Department of Health. NHS reference costs. 2005.
- British Medical Association and Royal Pharmaceutical Society of Great Britain. British National Formulary No 49.
- Claxton K. Bayesian approaches to the value of information: implications for the regulation of new pharmaceuticals. Health Economics 1999;18:269–74.
