To identify the knowledge of ionising radiation doses and radiation-related risk in common cardiac procedures among cardiology trainees, cardiologists and general practitioners with a specialist interest in cardiology, a face-to-face questionnaire survey of 47 cardiac specialists, both regular referrers and practitioners of radiation-based procedures, was conducted at the British Cardiovascular Society Annual Conference 2006.
Of the 47 medical professionals surveyed, 21 (45%) provided the correct radiation dose for at least one imaging procedure. Most reported doses were below the lower limit of the reference range: the median (interquartile range) radiation dose reported by the respondents was 2 mSv (0.4 to 10 mSv) for coronary angiography (CA) and 6 mSv (1 to 15.8 mSv) for percutaneous coronary intervention (PCI); 2 mSv (0.5 to 15 mSv) and 6 mSv (1 to 20 mSv) for myocardial perfusion scintigraphy (MPS) and computed tomographic angiography (CTA), respectively. A risk of malignancy from ionising radiation exposure of one in 10,000 for CA (actual risk 1:5,000) and of one in 5,000 for MPS and CTA (actual risk 1:1,000) was reported by the majority of respondents.
We conclude that there is significant underestimation of both dose and radiation-related risk to patients. Patients are unable to make informed decisions when consenting for these common procedures, as clinical staff are unaware of the correct radiation dose and associated risk, and therefore are unable to advise patients properly.
Introduction
The use of ionising radiation within cardiology is widespread with both myocardial perfusion scintigraphy (MPS) and conventional invasive coronary angiography (CA) being common diagnostic investigations for coronary artery disease. In the UK, some 70,000 MPS were performed in 20001 and over 205,000 CA in 2005.2 The use of ionising radiation is likely to increase further with the advent of cardiac multi-detector X-ray computed tomography (MDCT) and X-ray computed tomographic angiography (CTA). Furthermore, all these investigations are deemed to involve moderate- or high-dose radiation.3 Previous studies have shown poor knowledge of the risks of ionising radiation among both medical staff4,5 and patients5 within general radiology.
The purpose of this study was to investigate the knowledge of radiation doses among clinical staff that frequently perform, refer, or advise patients on common cardiac diagnostic investigations. We conducted a survey of cardiologists, cardiology specialist registrars (SpR) and general practitioners with a special interest (GPSI) in cardiology to evaluate their knowledge of both ionising radiation dose and risk of malignancy for common diagnostic cardiac investigations.
Subjects and methods
A questionnaire was devised asking what ionising radiation dose was associated with common cardiac diagnostic investigations including echocardiography, X-ray CA, percutaneous coronary intervention (PCI), MPS, CTA and cardiac magnetic resonance imaging (CMR). The dose for a plain chest radiograph (0.02 milliSieverts [mSv])6 was given as a guide to aid completion. Respondents were also asked the additional risk of malignancy at 20 years from three investigations; CA, MPS and CTA. Finally, they were asked for an estimate of the annual ionising radiation dose from background radiation in the UK.
The questionnaire was conducted at the British Cardiovascular Society conference in 2006; all participants had daily contact with patients undergoing these cardiac investigations. Participants were surveyed individually and face-to-face to prevent collaboration bias. Professional grade and year of training was documented for cardiology SpRs.
The study group comprised over 8% of all cardiology SpRs in the UK,7 all of whom are required to undergo radiation protection training as part of The Ionising Radiation (Medical Exposure) Regulations 20008 (IR[ME]R) and Ionising Radiations Regulations 19999 and to gain an IR(ME)R certificate of training prior to personally exposing patients to ionising radiation.
The reference ranges for the investigations were: echocardiography (0 mSv); CA (2–5 mSv);10,11 PCI (5–40 mSv);10–12 MPS (8–21 mSv);13 CTA (8–15 mSv)14,15 and CMR (0 mSv). The potential risk of malignancy was calculated for each procedure using the value 0.05 Sv-1, i.e. a risk of inducing fatal cancer following a 1 mSv whole body exposure of one in 20,000 for a population of all ages.16 For an MPS scan of dose range 8–21 mSv the risk would be 1:2,500 to 1:950. For the purpose of this study a risk per procedure of one in 1,000 was used as reference, which is equivalent to 20 mSv. The mean annual background dose of ionising radiation in the UK is 2.2 mSv.6
Statistical analysis
The data were summarised using the median (interquartile range) and differences between groups analysed with the use of the Kruskal-Wallis test. Categorical variables were studied using the chi-square test. Probabilities less than 0.05 were considered statistically significant.
Results
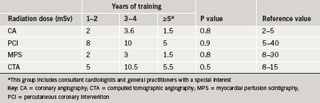
Of the 47 medical professionals surveyed, all were practising physicians and of these, 91% were cardiology SpRs. Of these 47 respondents, 21 (45%) provided the correct radiation dose for at least one imaging procedure. Only two physicians reported the correct dose for all the imaging procedures. Most reported doses were below the lower limit of the reference range, and this was more marked for the non-invasive procedures MPS and CTA. The median (interquartile range) radiation dose reported by the surveyed physicians was 2 mSv (0.4 to 10 mSv) and 6 mSv (1 to 15.8 mSv) for CA and PCI, respectively. The estimated median (interquartile range) radiation dose for MPS was 2 mSv (0.5 to 15 mSv) and 6 mSv (1 to 20 mSv) for CTA. Physicians were divided into three groups according to years of specialised training: years 1 and 2 (group 1), 3 and 4 (group 2) and 5 or more including consultant cardiologists and GPSI (group 3). No difference was found between the groups for the estimated radiation doses (table 1).
The estimated median (interquartile range) annual background dose of ionising radiation was 0.5 mSv (0.03 to 2.5 mSv), and this was much lower than the reference value of 2.2 mSv.6
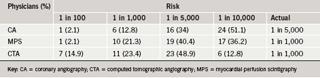
Over half of respondents reported a risk of malignancy from ionising radiation exposure during diagnostic imaging procedures of one in 10,000 for CA (actual risk 1:5,000) and of one in 5,000 for MPS and CTA (actual risk 1:1,000) (table 2).
Discussion
This study shows that cardiology trainees and specialists significantly underestimate the radiation doses that patients receive from commonly performed cardiac imaging procedures involving ionising radiation, particularly non-invasive diagnostic imaging. Moreover, most physicians underestimate the risk of malignancy from radiation exposure, despite the conservative reference risk of malignancy used in this study (1:1,000 per procedure, equivalent to 20 mSv). This lack of knowledge prevails across all levels of training. The fact that background doses of radiation are also underestimated by the great majority of respondents suggests a lack of general knowledge on radiation exposure. Up to 250 deaths per year are attributed to medical exposure to ionising radiation.17
It is therefore important that those individuals involved with referring patients for, or advising patients on, these procedures have knowledge of which investigations use ionising radiation, the correct doses involved and the potential risk.
Ionising radiation exposure and the risk associated with its use must, however, be put into the context of the population being investigated. The benefits of these investigations in detecting or excluding coronary artery disease are significant and early treatment and intervention will prevent far more harm than delivered by the use of ionising radiation.
As with previous general surveys of knowledge of radiation exposure,4 few respondents had any knowledge of the ionising radiation dose to which their patients were being exposed. However, previous surveys assessed only general physicians’ knowledge of a full spectrum of general radiological procedures whereas this study highlights the lack of knowledge among specialists who are often performing procedures that expose their patients to ionising radiation, as well as referring for, and advising patients on, these investigations. It appears that attendance at an IR(ME)R training course is insufficient given the lack of knowledge across all years of specialist training.
Cardiac nurses also have poor knowledge of ionising radiation exposure for common cardiac investigations and in particular are unaware of those that do not use radiation such as echocardiography and CMR.18 This lack of knowledge undermines their role as the patient’s advocate helping to ensure that they are aware of the correct information on dose and risk that allows them to give properly informed consent. The concept of fully informed consent is even further undermined by the findings of this study.
Conclusion
This study highlights poor knowledge of ionising radiation among cardiac-trained healthcare professionals, and suggests that current training may be insufficient. Accurate patient information is compromised and fully informed consent undermined.
Conflict of interest
None declared.
Key messages
- The knowledge of ionising radiation burden for common diagnostic and therapeutic cardiac procedures is poor among cardiac trainees
- As both referrers and practitioners it is essential that cardiologists should have a sound knowledge of ionising radiation burden as many common procedures are deemed to have a ‘significant’ ionising radiation burden (>10 mSv) and during the investigation of coronary artery disease, more than one investigation involving radiation is not uncommon
- IR(ME)R training does not appear to sufficiently allow an understanding of either ionising radiation burden or its potential health effects
- Patients should be advised of both the ionising radiation burden and potential consequences to health as part of their consent to medical procedures involving ionising radiation. The risk will likely be small compared with their risk of undiagnosed or untreated coronary artery disease
References
- Kelion AD, Anagnostopoulos C, Harbinson M, Underwood SR, Metcalfe M. Myocardial perfusion scintigraphy in the UK: insights from the British Nuclear Cardiology Society Survey 2000.Heart 2005;91(suppl 4):iv2–5.
- British Cardiovascular Intervention Society Audit 2005. Available from: http://www.bcis.org.uk/resources/documents/returns2005.ppt#856,23,UK Interventional and Diagnostic centres 2005
- Health Protection Agency. Radiation Exposure of the UK Population from Medical and Dental X-ray Examinations. NRPB-W4. Didcot: NRPB, 2001.
- Shiralkar S, Rennie A, Snow M, Galland RB, Lewis MH, Gower-Thomas K. Doctors’ knowledge of radiation exposure: questionnaire study. BMJ 2000;327:371–2.
- Lee CI, Haims AH, Monico EP, Brink JA, Forman HP. Diagnostic CT scans: assessment of patient, physician, and radiologist awareness of radiation dose and possible risks. Radiology2004;231:393–8.
- Royal College of Radiologists. Making the Best Use of a Department of Clinical Radiology. 4th ed. London: Royal College of Radiologists, 1998.
- Royal College of Physicians Workforce Planning Department. Census of Consultant Physicians in the UK, 2005. London: Royal College of Physicians. (IBSN: 978 1860162954)
- The Ionising Radiation (Medical Exposure) Regulations 2000 (SI 2000 No 1059). London: HMSO, 2000.
- The Ionising Radiations Regulations 1999 (SI 1999 No 3232). London: HMSO, 1999.
- Efstathopoulos EP, Karvouni E, Kottou S et al. Patient dosimetry during coronary interventions: a comprehensive analysis. Am Heart J 2004;147:468–75.
- Cioppa A, Picano V, Ambrosini G et al. Radiation dose exposure during cardiac catheterisation. Eur Heart J 2005;26(supp1 1):476–7, P2925.
- Vano E, Gonzalez L, Guibelalde E et al. Evaluation of risk of deterministic effects of fluoroscopically guided procedures. Radiat Prot Dosimetry 2006;117:190–4.
- Notes for guidance on the clinical administration of radiopharmaceuticals and use of sealed radioactive sources. ARSAC, December 2006.
- Morin RL, Gerber TC, McCullough CH. Radiation dose in computed tomography of the heart. Circulation 2003;107:917–22.
- Hausleiter J, Meyer TS, Hadamitzky M, Martinoff S, Schoemig A. Effective radiation dose of cardiac computer tomography angiography. A comparison between 64- and 16-slice technology. Eur Heart J 2005;26(suppl 1):P3155.
- ICRP. Recommendations of the International Commission on Radiological Protection. ICRP: Publication 60, 1990; Volume 21, No. 1–3.
- Royal College of Radiologists and National Radiological Protection Board. Patient dose reduction in diagnostic radiology. Documents of the National Radiological Protection Board 1990;1:No. 3.
- Stanbridge K, Latus K, Robinson C, Reyes E, Nicol ED. Radiation dose from cardiac investigations: a survey of cardiac nurses. Br J Cardiac Nursing, in press, 2007; 2:147–90
