A 37-year-old man presented with palpitations and recurrent episodes of pre-syncope. He had a past medical history of atrial septal defect (ASD) repair aged seven.
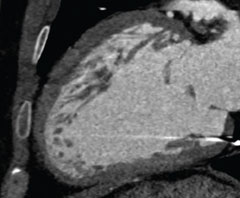
At age 16, he started to suffer with recurrent attacks of pre-syncope and a 24-hour tape documented runs of broad complex tachycardia for which he was commenced on sotalol and fitted with a single-chamber rate-responsive pacing system. Electrocardiogram (ECG) on admission showed an unusual pattern of right bundle branch block, extreme left axis deviation and first-degree heart block. Transthoracic echocardiogram demonstrated biventricular dilatation, moderately impaired left ventricular systolic function and prominent trabeculations, which raised the suspicion of left ventricular non-compaction (LVNC). Interestingly, his twin brother also had an ASD repair in childhood, suffered with recurrent syncopal episodes and was fitted with an implantable cardiac defibrillator (ICD) at age 36 following documented ventricular tachycardia. Cardiac magnetic resonance (CMR) imaging was precluded due to the pacemaker and ECG-gated cardiac computed tomography (CT) was instead performed. This showed increased ventricular trabeculations along the apical and mid-ventricular segments of the anterior and lateral walls (figures 1 and 2). The coronary arteries were normal and functional analysis showed regional wall motion abnormality with an estimated ejection fraction of 44%. The CT appearances were consistent with a diagnosis of LVNC. He was treated with ICD implantation and both he and his brother remain well.

Discussion
LVNC is a rare congenital cardiomyopathy caused by an arrest of myocardial morphogenesis. Imaging studies reveal a dilated hypocontractile left ventricle, which has a two-layered wall. The subepicardial myocardium is thin and normally compacted with a thicker non-compacted subendocardial layer. A ratio of non-compacted:compacted myocardium greater than 2:1 is considered diagnostic. Prompt recognition of LVNC is mandatory because of its clinical manifestations, which include heart failure, thromboembolic events and ventricular arrhythmias. CMR is the imaging modality of choice for LVNC with a high diagnostic accuracy. It provides clear delineation of the extent of non-compaction and also helps distinguish pathological LVNC from lesser degrees of trabeculation, which may be seen in healthy subjects. CMR is, however, contraindicated in patients with a pacemaker or other implanted electrical device. There have been tremendous advances in CT technology in recent years with the advent of multi-detector scanners and ECG-gated acquisition. Cardiac CT is widely used for the investigation of coronary artery disease in selected patient groups and can also provide a comprehensive assessment of cardiac morphology. The high spatial resolution of CT can readily demonstrate the prominent trabeculations in cases of LVNC as shown in this case.
Conflict of interest
None declared.
