There are currently limited data regarding multi-detector computed tomography (MDCT) coronary angiography in very elderly patients. This study reviews the utility of MDCT coronary angiography in octogenarians examined at our institution.
We reviewed 26 patients (mean age 83.1 ±4.6 years, range 80–96; 13 male) who attended for MDCT coronary angiography at our institution between January 2005 and January 2008. Scan indications, findings and clinical outcomes were recorded. Studies were graded according to overall image quality.
One patient was excluded because of contrast extravasation. Of the 25 complete studies, image quality was at least adequate in 72% of patients. A total of 35 significant (>50% diameter narrowing) stenoses were detected. The mean Agatston score was 1182.7 ±1080.2 in the 14/25 patients evaluated. In 6/25 patients (24%) MDCT excluded significant stenoses; in 12/25 patients (48%) one or more potentially significant stenoses were identified, a diagnosis confirmed in the four patients who underwent further investigations; in 7/25 patients (28%) the MDCT scans were of insufficient diagnostic quality.
In conclusion, MDCT coronary angiography is feasible in the majority of very elderly patients. Diagnostic scans were obtained in most octogenarian patients, allowing detection of potentially flow-limiting stenoses or exclusion of significant disease.
Introduction
 Very elderly individuals are the fastest growing segment of most Western populations, with those aged 80 and older projected to triple in number by the middle of this century.1,2 The prevalence of coronary artery disease is high in this age group, and diagnostic investigations are being used with increasing frequency when angina is poorly controlled by medical therapy. However, due to more extensive disease and less functional reserve, invasive investigations have a higher complication rate in the very elderly than in younger patients.3 Therefore, non-invasive tests that identify those patients most likely to benefit from invasive angiography would seem particularly appropriate in older individuals. Multi-detector computed tomography (MDCT) has emerged as such a technique. Currently there are only limited data regarding the use of MDCT in very elderly patients. The aim of this study was to evaluate the diagnostic yield and clinical utility of non-invasive 64-MDCT coronary angiography in octogenarians referred to our institution.
Very elderly individuals are the fastest growing segment of most Western populations, with those aged 80 and older projected to triple in number by the middle of this century.1,2 The prevalence of coronary artery disease is high in this age group, and diagnostic investigations are being used with increasing frequency when angina is poorly controlled by medical therapy. However, due to more extensive disease and less functional reserve, invasive investigations have a higher complication rate in the very elderly than in younger patients.3 Therefore, non-invasive tests that identify those patients most likely to benefit from invasive angiography would seem particularly appropriate in older individuals. Multi-detector computed tomography (MDCT) has emerged as such a technique. Currently there are only limited data regarding the use of MDCT in very elderly patients. The aim of this study was to evaluate the diagnostic yield and clinical utility of non-invasive 64-MDCT coronary angiography in octogenarians referred to our institution.
Materials and methods
Patients aged 80 years and over who underwent MDCT coronary angiography at our institution between January 2005 and January 2008 were retrospectively identified. Twenty-six patients (mean age 83.1 ±4.6 years, range 80–96; 13 male and 13 female) were included. All the MDCT studies were requested on a non-urgent out-patient basis. The hospital ethical review board approved the study, and informed consent was not required.
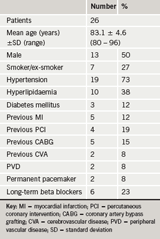
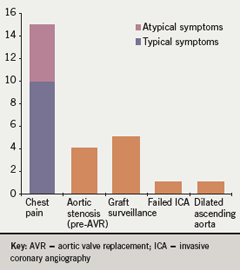
Baseline patient characteristics are listed in table 1. The clinical indications for MDCT of the study population are reported in figure 1. Exclusion criteria for MDCT included sustained arrhythmia, a heart rate greater than 90 beats per minute despite beta-blockade, allergy to contrast, poor renal function (estimated glomerular filtration rate [eGFR] <30 ml/min) and severe chronic congestive cardiac failure (New York Heart Association [NYHA] class IV).
MDCT coronary angiography was performed with a 64-slice scanner (Somatom Sensation 64, Siemens, Forchheim, Germany). If necessary, beta blockers were utilised to achieve an optimal heart rate <65 beats per minute. Coronary artery calcium quantification was performed in cases of suspected coronary artery disease, but not when a diagnosis of coronary artery disease had been previously established. Images were interpreted by two consultant radiologists with more than 10 years’ experience in cardiothoracic imaging. Coronary arteries were examined using multi-phase axial datasets, multi-planar reconstructions, curved multi-planar reformation, maximal intensity projections and 3D volume-rendered images. A significant stenosis was defined as narrowing of the coronary lumen greater or equal to 50%. Image quality was graded as excellent (no artefacts, unrestricted evaluation), good (minor artefacts, good diagnostic quality), adequate (moderate artefacts, acceptable for routine clinical diagnosis), and poor (severe artefacts impairing accurate evaluation).
Clinical usefulness of the MDCT examinations were classified as follows:
- Complete diagnostic information or specific clinical question answered, no further tests needed
- High likelihood of >50% stenosis, potential targets for coronary revascularisation identified
- Inadequate diagnostic quality, other non-invasive tests or angiography recommended.
- For statistical analysis, the frequency and percentage are reported for
discrete variables, and mean and standard deviation for continuous variables.
Results
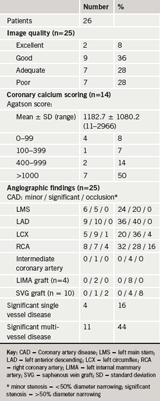
One examination was aborted due to contrast extravasation and this patient was excluded from further analysis. Complete MDCT studies were acquired in 25/26 (96%) patients. MDCT findings are summarised in table 2.
A total of 70 stenoses were identified in 23 (92%) patients: 28 (40%) non-significant (<50% diameter stenosis), 35 (50%) significant (≥50% diameter stenosis) and seven (10%) total occlusions.
Of the 7/25 (28%) studies graded as poor, motion artefacts were responsible in all cases, usually due to breathing and/or frequent ectopic beats. Artefacts related to pacing wires in two patients and massive calcium deposits in two patients additionally contributed to image deterioration. Coronary calcification restricted complete evaluation to some degree in 15/25 (60%) patients, but image quality was still at least adequate for diagnostic purposes in the majority of these cases (87%).
A total of eight stented segments were detected in four patients who underwent previous percutaneous coronary intervention (PCI). Assessment was possible in all cases. No significant in-stent restenosis was detected, although two stented saphenous vein grafts (SVGs) were occluded beyond the patent stents.
A total of four left internal mammary arteries (LIMA) and 10 SVGs were identified in five patients who underwent previous coronary artery bypass grafting (CABG). The LIMA grafts were fully assessable to the distal anastamosis in 2/4 (50%), of which one was determined to be patent and the other had a >50% narrowing at the distal anastamosis. Of the other LIMA grafts, artefact from metallic clips precluded complete evaluation in 1/4 (25%) and obscured the origin in 1/4 (25%) beyond which there was poor distal run-off. Among the 10 SVGs, all demonstrated at least adequate image quality. Seven/10 (70%) were recognised to be patent (normal or <50% stenosis), 1/10 (10%) showed a significant stenosis (>50%) and 2/10 (20%) contained patent intra-luminal stents but were occluded distally.
In 6/25 (24%) patients (group 1), no further examinations were required as the MDCT provided complete diagnostic information and no significant stenoses were detected. In 12/25 (48%) patients (group 2), one or more potentially significant stenoses were identified. Of these, three patients underwent invasive coronary angiography, which confirmed the presence of significant stenoses and fully correlated with the location of the lesions. One patient had a positive adenosine single photon emission computed tomography (SPECT), which demonstrated perfusion abnormalities in the territory of the MDCT-detected stenosis, but the decision was made to treat medically. Another patient proceeded to aortic valve replacement, but concomitant coronary bypass grafting was not performed despite two stenoses >50% being identified on the pre-operative MDCT. In seven patients, no further investigations were performed, and the patients were managed medically in the context of other clinical problems. In 7/25 (28%) patients (group 3), the MDCT angiogram was of insufficient diagnostic quality to enable full evaluation; in 6/7 (86%) some information was available (five potentially significant stenoses identified in three patients) but data were missing in important areas; in 1/7 (14%) the MDCT provided totally non-interpretable images.
Discussion
Very elderly patients with coronary artery disease display extreme heterogeneity in terms of biological/physiological fitness and, therefore, pose unique diagnostic and therapeutic challenges.4 The current ‘gold standard’ investigation is invasive coronary angiography, but in older patients this is associated with increased risk of periprocedural complications.3,5 Establishing objective criteria for determining which octogenarian patients are most likely to benefit from invasive procedures is a difficult task, but one that will become increasingly important as elderly patients with advanced coronary disease in which it is feasible to perform revascularisation will become more numerous.4 Although several non-invasive tests have shown high prognostic value to predict future coronary events, coronary angiography is often eventually required due to inconclusive results or persistent symptoms.6 MDCT permits non-invasive visualisation of the coronary arteries with high precision. The technique avoids many of the procedural risks associated with invasive angiography, and in this regard would seem to be of benefit to very elderly patients.
We found that MDCT coronary angiography was technically feasible in the majority of octogenarians. MDCT provided complete diagnostic information in 72% of 25 patients studied. Of those with fully diagnostic studies, only 3/12 (25%) patients with significant stenoses went on to invasive angiography, which included 2/5 (40%) with left main stem disease. Since angiography is primarily indicated to plan management in octogenarians who are not responding to medical therapy, it can be argued that the results of revascularisation procedures are central to the decision whether or not to recommend an angiographic study.4 There is questionable value in performing such a test, albeit non-invasive, if subsequent intervention is unlikely to be feasible. The relatively low follow-on rate to invasive angiography in our study may have been partly due to the perception of an adverse risk–benefit relationship in some cases.
Perhaps the octogenarian subset with the most to gain from MDCT are those with known coronary artery disease, in whom non-invasive angiography can answer specific clinical questions. For example, patients with previous coronary artery stenting or CABG who present with chest pain may benefit from a first screening with MDCT, thus potentially avoiding repeated invasive procedures. In our study group, 100% of stented segments and 86% of grafts could be adequately evaluated for patency.
For the majority of patients in this study, we have no independent verification of the MDCT findings by conventional angiography. The absence of a routine diagnostic gold standard is a limitation, but reflects actual management decisions in this particular patient population. MDCT coronary angiography is also not completely without risk. Older patients are especially vulnerable to contrast-related nephrotoxity, although we did not encounter any cases in our series.
In conclusion, MDCT coronary angiography is feasible in the majority of very elderly patients, allowing detection of potentially flow-limiting stenoses or exclusion of significant disease. However, the test is unlikely to be helpful
in patients who would not be suitable candidates for subsequent invasive coronary angiography. Thus, to maximise the diagnostic yield and clinical utility, appropriate patient selection is likely to be even more important in very elderly patients than in younger individuals. Nevertheless, we feel that the technique may have a valuable role in older patients if a specific clinical question, such as coronary stent or graft patency, is addressed.
Conflict of interest
None declared.
Key messages
- Multi-detector computed tomography (CT) coronary angiography avoids many of the risks associated with invasive angiography but there are currently limited data regarding use of this technique in the very elderly
- Diagnostic images are obtained in the majority of octogenarian patients
- Heavy calcification and motion artefacts are most frequently responsible for non-diagnostic scans
- The test is most likely to be of benefit in very elderly patients if a specific clinical question is addressed
References
- Johnson WM, Smith JM, Woods SE, Hendy MP, Hiratzka LF. Cardiac surgery in octogenarians: does age alone influence outcomes? Arch Surg 2005;140:1089–93.
- Peterson ED, Alexander KP, Malenka DJ et al. Multicenter experience in revascularization of very elderly patients. Am Heart J 2004;148:486–92.
- Ricou FJ, Suilen C, Rothmeier C, Gisselbaek A, Urban P. Coronary angiography in octogenarians: results and implications for revascularization. Am J Med 1995;99:16–21.
- Friesinger GO. Coronary angiography in octogenarians: problems and possibilities. Am J Med 1995;99:13–15.
- Reynen K, Bachmann K. Coronary arteriography in elderly patients: risk, therapeutic consequences and long-term follow-up. Coron Artery Dis 1997;8:657–66.
- Conti A, Sammicheli L, Gallini C, Costanzo EN, Antoniucci D, Barletta G. Assessment of patients with low-risk chest pain in the emergency department: head to head comparison of exercise stress echocardiography and exercise myocardial SPECT. Am Heart J 2005;149:894–901.
