The ESC 2009 guidelines1 include a clinical classification into four categories:
- Einsenmenger’s syndrome. Large defects causing systemic-to-pulmonary shunts, increased pulmonary vascular resistance (PVR), reversal or bidirectional shunts, cyanosis, erythrocytosis and multiple organ involvement
- PAH associated with systemic-to-pulmonary shunts. Moderate to large defect, moderate increase in PVR, no cyanosis at rest
- PAH associated with small defects (approximately VSD <1cm or ASD<2cm), with similar clinical picture to IPAH
- PAH after corrective surgery, either immediately after surgery or recurrent at a later stage
Key learning point
- Pulmonary hypertension is defined as an increase in mean pulmonary arterial pressure (PAP) ≥25 mmHg at rest as assessed by right heart catheterization. It is found in many different clinical conditions
Pathophysiology of pulmonary arterial hypertension
This section of the programme looks at PAH. Clearly, the pathology of PH will vary according to the underlying cause (figure 2), and the clinical picture and molecular findings will be different in PAH and PH due to lung disease, left heart disease and chronic thromboembolic pulmonary hypertension, for example.
Structural changes
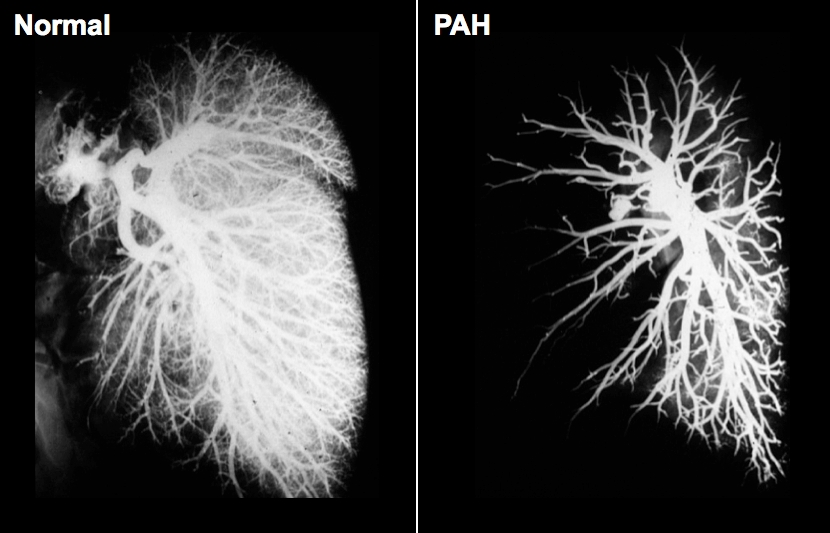
PAH is a disease of the pulmonary blood vessels, which results in narrowing and loss of small vessels predominantly on the arterial side of the circulation. The effect of PAH on the pulmonary circulation can be seen in figure 3, which demonstrates a dramatic loss of blood vessels compared to the normal lung. The normal pulmonary circulation is a low-pressure, low-resistance circuit through which the entire cardiac output must pass. It is supported by the right ventricle. The embryological origin of the right ventricle is different from that of the left ventricle. The myocardial structure and geometry of the right ventricle differ from that of the left ventricle. The right ventricle works efficiently against a low (normal) afterload.

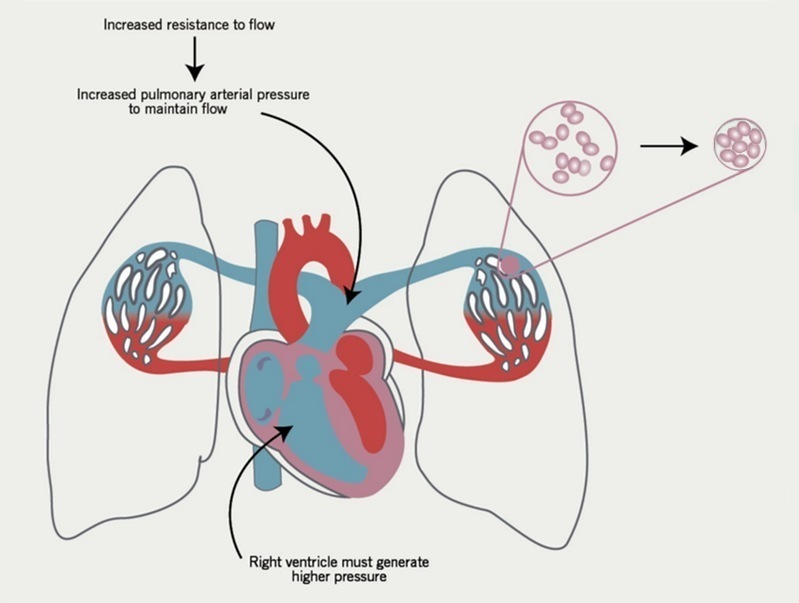
The consequence of these structural changes in the lung circulation is that
- the overall cross-sectional area of the pulmonary vascular bed is reduced
- when this reduction reaches about 60-70% of the normal cross-sectional area, it presents a significantly increased resistance against which the right ventricle must work (figure 4)
- this is predicted by Ohm’s Law, which describes in this situation how increased resistance requires the generation of higher pressure to maintain cardiac output