Introduction
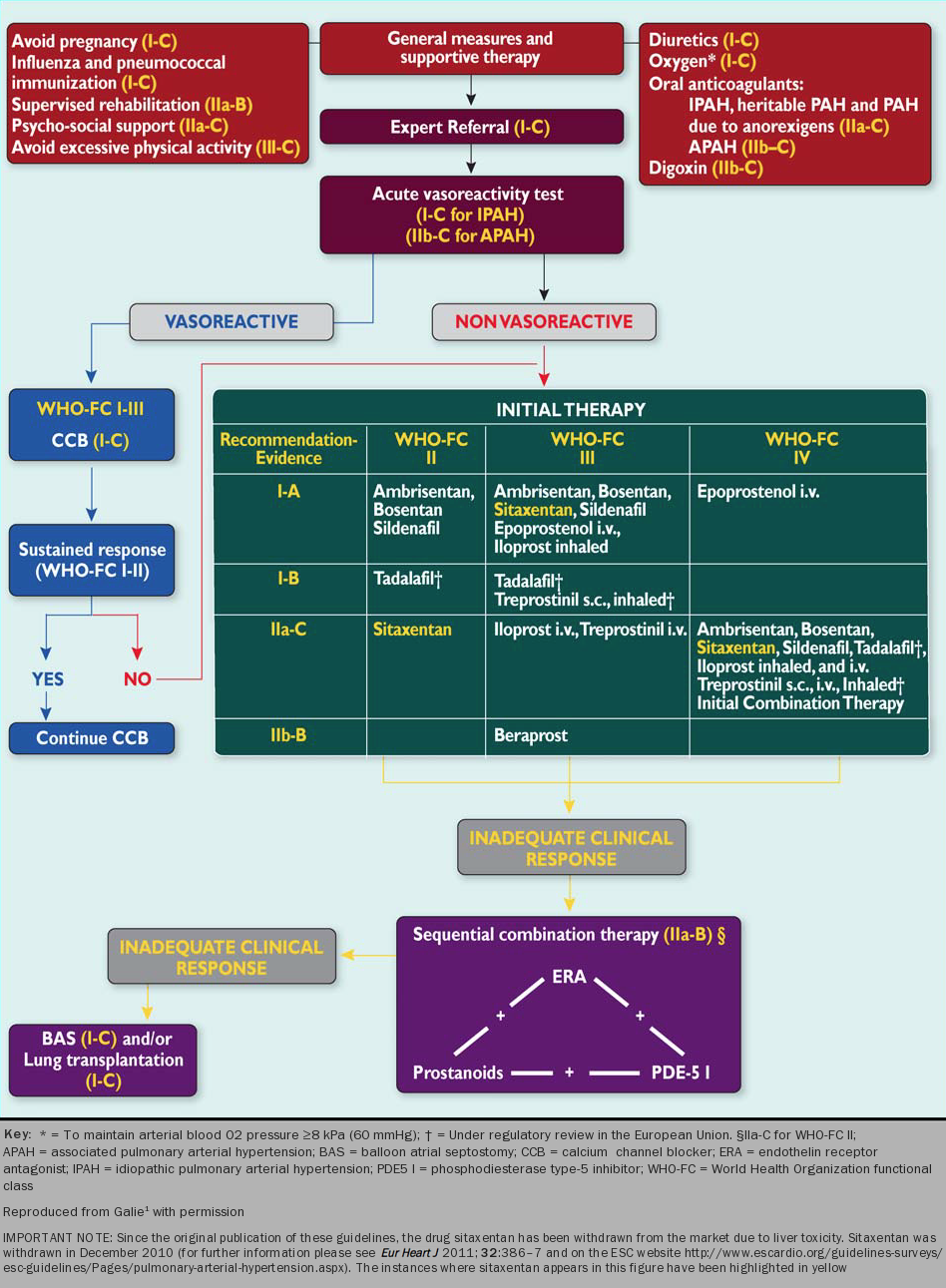
Once the patient has undergone all investigations necessary to establish a precise diagnosis of pulmonary hypertension, with any associated conditions identified and a clear haemodynamic profile understood, then a treatment plan can be arranged. Patients with pulmonary arterial hypertension will be considered for evidence-based disease-targeted drug therapy, as shown in figure 1.
Patients with chronic thromboembolic hypertension should be discussed with a pulmonary endarterectomy surgeon.
Patients with pulmonary hypertension related to left heart disease, lung disease and hypoxia should be managed by a cardiologist or respiratory physician. Disease-targeted therapy for PAH may potentially cause harm in these patients: there is currently no evidence for the use of the disease-targeted therapies discussed below in these patients.
The management of PAH consists of general and supportive measures plus selection of evidence-based drug treatment. Modern drug therapy leads to a significant improvement in patient symptoms and a slower rate of clinical deterioration (ESC 2009 guidelines).1
Various treatment algorithms to guide drug treatment for PAH have been published, both in Europe and North America. The significant trial results for the individual drug classes are discussed below. It should be appreciated that this algorithm is based mainly on clinical trials in patients with idiopathic, heritable and anorexigen-induced PAH. Some trials have included CTD, congenital heart disease with a shunt and HIV. Although some drugs are licensed for use in PAH as a group, they do not necessarily have an evidence base in each of the subclasses.
There are no large head-to-head trials of disease-targeted therapies. The choice of therapy depends on the circumstances of an individual patient as well as drug availability and licensing. The algorithm shows drugs for which there is evidence by WHO functional class. The trials of individual agents have included heterogeneous patient populations with variable severity of PAH. For this reason it is not useful to compare agents between trials. Most RCTs of drug therapies have been conducted in stable patients for a short duration. Since unstable patients who were deteriorating were not enrolled, it is not surprising to find that clinical trials underestimate the mortality in a real-life patient population. This difference is highlighted by the lower mortality rate in patients with prevalent disease compared to those who present for the first time. The short duration of trials is being addressed in current studies. Recent event-driven trials have been conducted with larger populations of patients over longer periods.
General measures in treating PAH

The objectives for treatment of pulmonary hypertension are to improve survival, to return the patient to work, education or to a useful role in society, to enable the patient to live independently, and to improve symptoms and quality of life. Patients need general support and specific advice about the general activities of daily life, time off work, travel and insurance.
The diagnosis brings with it a degree of social isolation, and many patients develop psychological symptoms such as depression and anxiety.2 Patient support groups can help patients and their families to cope with the disease, and by providing helpful and practical information. Some may need referral to a psychologist.
Selected patients can be encouraged to be physically active, within safe limits: mild exertion and breathlessness are acceptable, but exercise that leads to severe dyspnoea, dizziness or chest pain is excessive. Caution with exercise prescription should be taken in patients who drop their systemic arterial pressure on exercise. Heavy physical exercise and isometric exercise are not recommended since they can lead to syncope. Tai Chi and yoga may be of benefit in some patients. In those who are physically unfit, supervised rehabilitation may be considered.
One randomised study investigated exercise training in 30 stable adult patients over three weeks while in hospital. Patients received intensive training plus psychological support. Longer 6MWT distances, better quality of life and improved functional class were observed in those patients who received exercise training.3 In a subsequent study different types of pulmonary hypertension appeared to respond equally well to exercise training, but there was a significant proportion of patients who developed a complication of this intervention.4
A sodium-restricted diet is advised in patients with right ventricular failure. Fluid restriction is sometimes needed also but should not normally be less than 1.5 litres per day. Renal function may suddenly deteriorate dramatically as a consequence of a reduction of cardiac output if patients become even mildly dehydrated. Routine immunisations for patients against influenza and pneumococcal pneumonia are also advised.
In patients who undergo elective surgery, care must be taken to ensure maintenance of oxygenation, a stable circulating volume and avoidance of acid-base disturbance. Systemic hypotension and large swings in circulating volume may precipitate dangerous haemodynamic instability. All patients should be managed by an anaesthetist with experience in managing these patients. Regional anaesthesia is probably better tolerated than general anaesthesia but this depends on the surgery being undertaken. Disease-targeted therapies for PAH must not be discontinued in the perioperative period. Consideration should be given to admitting these patients to the intensive care unit in the immediate postoperative period. Elective surgery carries a significantly higher risk in PAH patients than in the general population.
Learning points
- The psychological wellbeing of PH patients is fundamental
- Lifestyle advice may include a physical exercise programme tailored to individual patients
