Management of arrhythmias in PAH
Sinus rhythm is important to maintain atrial transport in these patients with fixed limited cardiac output. Loss of atrial transport cause by arrhythmias often results in marked clinical deterioration.35 Arrhythmias are an increasing clinical problem in patients with pulmonary arterial hypertension1 as patients with PAH live longer. Arrhythmias should always be considered as a cause of deterioration, even if the patient does not report palpitations. The arrhythmia observed most commonly is atrial flutter, which may be slow. Atrial fibrillation is dangerous in severe pulmonary hypertension. The aim in PAH patients should be to maintain stable sinus rhythm.
Patients who are deteriorating, with atrial tachyarrhythmias, may require urgent DC cardioversion. Treatment of atrial flutter with antiarrhythmic drugs without negative inotropic effects, such as amiodarone, may be beneficial. In atrial flutter, ablation is helpful. Beta blockers are poorly tolerated in patients with pulmonary hypertension and should not be used.
Learning point
- Antiarrhythmic drugs which do not affect myocardial contractility may be useful in selected PAH patients
Drug-drug interactions
A number of drugs are normally contra-indicated in pulmonary hypertension:
- Beta blockers
- Non-steroidal anti-inflammatory drugs
- Oestrogens
The following drugs should be avoided wherever possible:
- Flecainide, mexilitene, propafenone, disopyramide
- Beta-blockers (at low doses, with caution)
- Tricyclic antidepressants (SSRIs preferred)
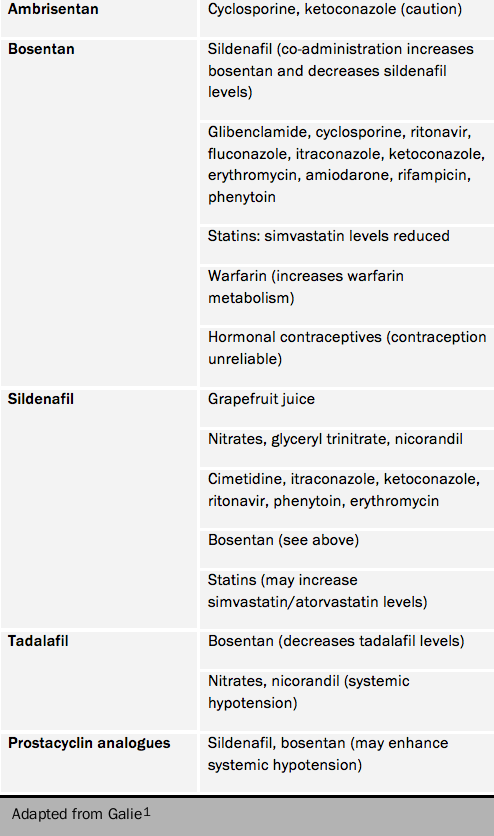
Table 5 lists potentially significant drug-drug interactions.
Surgical treatment for PAH
Lung transplantation
Many patients experience progressive decline in function despite medical treatment. Symptoms such as progressive dyspnoea, ascites, oedema and syncope relate mainly to worsening right heart failure.
The ultimate treatment for PAH is lung transplantation. PAH is not known to recur in transplanted lungs. Patients exchange the management of severe PAH for that of transplanted lungs, and the risks of rejection. With the median survival of transplanted patients at about 50% at five years and the very limited availability of donor organs, the timing of transplantation is difficult. It is important to refer patients who may be suitable for transplantation in good time so that they may placed on a transplant list and transplanted while on combination therapy. Bilateral lung transplantation is preferred to heart-lung transplantation unless there is a reason to transplant the heart itself. In most patients the right ventricle will recover post-operatively. To achieve optimum care, close collaboration between the PH centre and their transplant unit is essential.
In selected patients with end-stage PAH, the quality of life, exercise capacity and long-term survival are improved by lung transplantation.
Atrial septostomy
Atrial septostomy is used to create a right-to-left shunt between the atria: it decompresses the failing right ventricle by creating a pressure release valve for the right side of the heart. It increases left ventricular preload and cardiac output. This improves systemic oxygen transport despite a decrease in systemic oxygen saturation.36,37
The procedure may be considered in patients with syncope, persistent right heart failure and failed medical treatment. It has not been the subject of a randomised controlled trial. In practice, the main group of patients receiving this procedure has been patients with IPAH. This procedure has a significant mortality, and it should only be performed in experienced centres in patients who have been rigorously assessed beforehand.
The procedure improves haemodynamic indices immediately after septostomy, with a significant decline in mRAP and functional class accompanied by an increase in mean left atrial pressure and cardiac index. Improvements in six-minute walk distance have also been seen. In the longer term, haemodynamic and echocardiographic improvements have been noted, and in one case series mean survival (excluding procedural deaths) was 63 months. Procedural mortality is still about 5%.
Learning points
- A number of surgical options remain for patients who fail medical treatment
- These include atrial septostomy, lung transplantation, and other measures such as ventricular assist devices
- These are high-risk interventions associated with high attrition rates

