To see whether a nurse-led clinic might be useful we audited how often patients discharged from follow-up were elsewhere seen in the community and how often events were picked up in patients being seen in a nurse-led valve clinic. We audited patients implanted with an OnX bileaflet mechanical heart valve between 1999 and 2010 by postal audit asking for details of follow-up and adverse events. We also analysed the outcome and adverse events from our nurse-led clinic over 30 months between 2009 and 2011 using our valve clinic audit database.
There were 188 OnX patients of whom only 125 (66%) were receiving regular cardiology follow-up. Of those in regular follow-up, there were 16 (13%) valve-related adverse events, and this was similar to those not receiving follow-up, 9 (14%). Only 126 (67%) had regular dental surveillance. In the valve clinic, there were 199 visits by 132 patients. Echocardiograms were required on eight visits (4%). There were three hard events (as defined by International Guidelines), 19 visits (10%) revealed adverse events requiring a cardiologist and six (3%) revealed events not requiring a cardiologist.
In conclusion, a nurse-led clinic provides effective long-term monitoring of valve patients. Large proportions of patients are discharged from cardiology/surgical units and are at risk of adverse valve-related events
Introduction
 Whether asymptomatic patients with a normally functioning replacement heart valve require routine follow-up remains uncertain. The European Society of Cardiology (ESC)1 and American Heart Association (AHA)2 guidelines recommend life-long annual follow-up by a cardiologist. However, pressure on out-patient space means that such patients are often discharged with the expectation that their GP will follow them or that they will return should a valve-related or other cardiac problem develop.3 This trend is likely to be accentuated by planned re-organisations within the National Health Service (NHS).4
Whether asymptomatic patients with a normally functioning replacement heart valve require routine follow-up remains uncertain. The European Society of Cardiology (ESC)1 and American Heart Association (AHA)2 guidelines recommend life-long annual follow-up by a cardiologist. However, pressure on out-patient space means that such patients are often discharged with the expectation that their GP will follow them or that they will return should a valve-related or other cardiac problem develop.3 This trend is likely to be accentuated by planned re-organisations within the National Health Service (NHS).4
To investigate whether regular monitoring in a nurse-led clinic was likely to be useful we addressed two questions: how many patients receive regular follow-up after valve replacement; and how often adverse valve-related events are picked up by patients being seen regularly in a nurse-led valve clinic?
Methods
Guy’s and St Thomas’ Hospital Trust (GSTT) performs between 555 and 728 valve operations annually, predominantly for patients within the South-East of England. Almost all patients are seen six weeks after discharge, but are then referred back for local follow-up unless they live in the GSTT catchment area. GSTT local patients are increasingly referred to a multi-disciplinary valve clinic.5 Within this, the nurse-led component is designed predominantly for asymptomatic patients with mechanical valves and normally functioning replacement biological valves five years and earlier after implantation. These cases do not require routine echocardiography.6 Simultaneous sonographer-led and cardiologist clinics allow immediate echocardiography or cardiology opinions should these be necessary for new valve-related or other cardiac or extracardiac symptoms or abnormal findings. A direct help-line also allows patients to report symptoms or discuss problems outside the clinic time with the nurse. This was not audited formally, but typically one patient each week reports new symptoms and two need advice from the nurse. Appropriate rapid-access appointments for the valve clinic can then be arranged.
Whether follow-up occurs was addressed by a postal audit of patients implanted with an OnX bileaflet mechanical heart valve between 1999 and 2010. This also included questions about clinical events as defined internationally,7 dental surveillance, the use of antibiotic prophylaxis, warfarin management and valve noise. To assess how often clinical events or symptoms requiring a cardiologist’s opinion are picked up in patients being seen regularly in a nurse-led valve clinic, we audited our nurse-led clinic over 30 months between 2009 and 2011. This clinic included all valve types implanted at GSTT and not just the OnX. End points were defined as:
- hard events as defined by international guidelines,7 e.g. death, transient ischaemic attack (TIA) and myocardial infarction
- events requiring a cardiology opinion
- other events not requiring cardiology opinion.
- In addition, a list was kept of questions and concerns raised by patients.
Results
Survey of patients with an OnX replacement heart valve
There were 188 patients of whom only 125 (66%) were receiving regular follow-up. Of those in regular follow-up, there were 16 (13%) valve-related events and this was similar to those not receiving follow-up, 9 (14%). The nature of the event was similar. In those receiving follow-up there were five TIA, two strokes (one haemorrhagic and one thrombotic), six bleeds and three dehiscences. In those without follow-up, there were four TIA, one thrombotic stroke, three bleeds and one case of endocarditis. Of the whole group, only 126 (67%) had regular dental surveillance and 86 of these (68% of 126) took prophylactic antibiotics. Valve noise was noticed by 136 (72%) and the noise was described as a continuous nuisance by six (3%), a nuisance some of the time by 40 (19%), rarely a nuisance by 37 (20%) and not a nuisance by the remaining 53 (28%).
The valve clinic
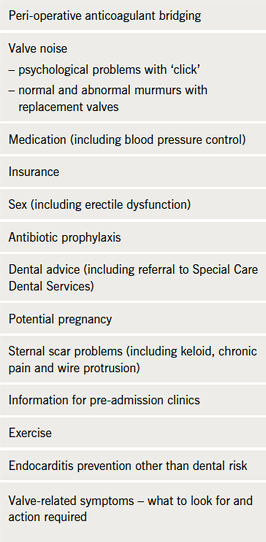
There were 199 clinic visits by 132 patients of whom 97 had a mechanical and 35 had a biological replacement valve. Each visit consisted of a clinical history and physical examination including auscultation. Echocardiograms were required because of a missing postoperative study or a clinical change (e.g. new heart failure, new breathlessness, new murmur) on eight visits (4%). One patient required admission because of ascites secondary to a co-existent malignancy. There were three hard events (two deaths, one with a haemorrhagic stroke, the other with pneumonia and one minor bleed despite therapeutic international normalised ratio [INR]). There were 19 visits (10%) revealing events requiring a cardiologist’s review (four with new breathlessness, one possible endocarditis, six arrhythmia, two inadequate blood pressure control, two chest pain and one each of: stopped all medications; need to assess fitness for general anaesthesia; falls; need to decide INR range). There were six (3%) events not requiring the clinic cardiologist (four wound or sternal wire problems and one TIA and paroxysmal atrial fibrillation [AF] already seen by another cardiologist). In addition, patients discussed a wide range of topics (table 1).
Discussion
We found that one-third of patients do not receive regular follow-up after valve replacement either in the community or at a hospital. International guidelines1,2 stipulate annual follow-up by a cardiologist after valve implantation. However, the hard event rate is low in patients with normally functioning valves without significant cardiac comorbidity, leading to the suggestion that these can be discharged8 provided that rapid access to a cardiologist is available should symptoms develop.3 This could be ensured using a telephone help-line.
We found no obvious difference in hard events between patients who did and did not receive serial follow-up after implantation of an OnX valve. However, this was not a formal comparison of the two strategies and we would have expected a significant difference had we investigated valves shown to be prone to early failure.9 Furthermore, a much larger proportion of patients had less severe problems for which serial follow-up would still have been likely to reduce the risk of a hard event. This follow-up can be devolved to a nurse-led clinic freeing the cardiologist to see new patients or those that have clinical problems.5 For example, the nurse in our clinic resolved problems with INR or rhythm control, discussed dental surveillance and gave lifestyle advice (table 1). As many as one-third of the OnX valve patients never saw a dentist, while all guidelines stipulate the need for regular surveillance to prevent endocarditis. Reminding about dental issues, and perhaps helping arrange a dentist, may arguably be one of the most important roles of a nurse-led clinic. Prosthetic valve endocarditis has a high mortality and there is evidence that antibiotic prophylaxis is effective.10,11 Despite this the National Institute for Health and Clinical Excellence (NICE) guidelines recommend avoiding antibiotic prophylaxis for any dental work. Our observation that the NICE guideline is not followed in two-thirds of patients suggests that a registry may establish the efficacy of antibiotics in preventing prosthetic valve endocarditis without the need for a randomised-controlled trial.
There are other models of valve surveillance clinic that are solely nurse led.12 Based on our experience of providing a ‘one-stop’ valve clinic, we believe that a valve clinic should be multi-disciplinary and include a cardiologist and sonographer, since 10% of visits required a cardiologist opinion and 4% an echocardiogram. This allows any problems identified to be promptly managed, usually within that clinic visit. However, in normally functioning mechanical valves and biological valves five years and earlier after implantation, routine echocardiography is not recommended,6 and devolving follow-up from a registrar to a specialist nurse is expected to save requests for unnecessary echocardiograms.13 Therefore, having a nurse-led component in a valve clinic provides long-term monitoring of the valve and general care for a larger number of patients than can be seen by a cardiologist. Arguably, a GP could provide the surveillance, but in practice this does not usually occur. Many problems detected by the nurse are clinically minor but could reduce the risk of a hard event, e.g. dental advice.
Conclusion
We conclude that a nurse-led clinic is useful. A large proportion of patients discharged from cardiology clinics do not receive any follow-up and are at risk of events. The nurse-led clinic found a clinically significant number of medical and other concerns of importance to the patient. We suggest that a formal comparison of event rates in a nurse-led surveillance clinic compared with usual care, which may often include no formal follow-up, is warranted.
Conflict of interest
None declared.
Key messages
- Only two-thirds of patients have regular follow-up after valve replacement
- Only two-thirds of patients have regular dental surveillance
- The National Institute for Health and Clinical Excellence (NICE) 2008 endocarditis guideline tends not to be followed
- A large proportion of patients have concerns, especially valve noise
References
- Vahanian A, Baumgartner H, Bax J et al. Guidelines on the management of valvular heart disease. Eur Heart J 2007;28:230–68. http://dx.doi.org/10.1093/eurheartj/ehm095
- Bonow RO, Carabello BA, Chatterjee K et al. ACC/AHA 2006 guidelines for the management of patients with valvular heart disease. J Am Coll Cardiol 2006;48:e1–e148. http://dx.doi.org/10.1016/j.jacc.2006.05.021
- Mahy IR, Dougall H, Buckley H et al. Routine hospital based follow up for patients with mechanical valve prostheses: is it worthwhile? Heart 1999;82:520–2.
- Hughes ML, Leslie SJ, McInnes GK, McCormac K, Peden NR. Can we see more outpatients without more doctors? J Roy Soc Med 2003;96:333–7. http://dx.doi.org/10.1258/jrsm.96.7.333
- Chambers J, Lloyd G, Rimington HM et al. The case for a specialist multidisciplinary valve clinic. J Heart Valve Dis 2012;21:1–4
- Zoghbi WA, Chambers JB, Dumesnil JG et al. American Society of Echocardiography recommendations for evaluation of prosthetic valves with two-dimensional and Doppler echocardiography. J Am Soc Echo 2009;22:975–1014. http://dx.doi.org/10.1016/j.echo.2009.07.013
- Akins CW, Miller DC, Turina MI et al. Guidelines for reporting mortality and morbidity after cardiac valve interventions. J Thorac Cardiovasc Surg 2008;135:732–8. http://dx.doi.org/10.1016/j.jtcvs.2007.12.002
- Mahmood I, Kallingal J, Sabtu N et al. “Routine” approach to follow-up and echocardiogram after a valve replacemnent surgery is not a clinically effective strategy. Heart 2009;95(suppl I):A36–A37.
- Pavoni D, Badano LP, Ius F et al. Limited long-term durability of the Cryolife O’Brien stentless porcine xenograft valve. Circulation 2007;116(suppl I):I-307–I-313. http://dx.doi.org/10.1161/CIRCULATIONAHA.107.688564
- Horstkotte D, Rosin H, Friedrichs W, Loogen F. Contribution for choosing the optimal prophylaxis of bacterial endocarditis. Eur Heart J 1987;8(suppl J):379–81.
- Chambers J, Shanson D, Hall R, Venn G, Pepper J, McGurk M. Antibiotic prophylaxis of endocarditis: the rest of the world and NICE. J Roy Soc Med 2011;104:138–40. http://dx.doi.org/10.1258/jrsm.2011.100356
- Anscome A, Cadet J. Follow-up of patients after heart valve surgery: setting up a nurse-led clinic. Br J Cardiac Nursing 2008;3:320–3.
- Taggu W, Topham A, Hart L et al. A cardiac sonographer led follow up clinic for heart valve disease. Int J Cardiol 2009;132:240–3. http://dx.doi.org/10.1016/j.ijcard.2007.11.076
