Patient knowledge and understanding of their condition is important in every field of medicine. It is particularly relevant in cardiology where choices between treatment options must be made and where patient participation in prevention of disease progression is a key part of therapy. In this study, knowledge and understanding of angina patients on options for revascularisation was explored. The aim was to reveal trends that may identify opportunities to improve care. This was a qualitative study utilising depth semi-structured interviews of angina patients who have had revascularisation (excluding primary percutaneous coronary intervention [PCI] for ST elevation myocardial infarction). The main outcome measure was patient perception on revascularisation options. It was conducted in an out-patient setting at the cardiac prevention and rehabilitation centre at Charing Cross Hospital, West London. Angina patients are referred to the centre before and after their revascularisation for rehabilitation and education sessions.
Several themes emerged from this study. First, patients are not fully aware of angina pathophysiology. Second, awareness of options for angina treatment is limited and their understanding heavily relies on the recommended option of the doctor. Other options are only briefly mentioned by healthcare professionals, and patients tend to turn to other sources, such as the internet and family/friends, for information. Despite the lack of understanding, all patients were happy with the way their treatment was chosen and were not too concerned about the level of information they had received.
In conclusion, patients have limited understanding of angina and options for treatment but are generally satisfied with their care. However, it is likely that impaired patient understanding will impact on their ability to maintain secondary prevention, especially lifestyle changes and medication concordance.
Introduction
 Angina is the most common presentation of coronary heart disease (CHD).1 Effective treatment requires appropriate medical care, but also patient participation in lifestyle changes and medication concordance. Patient understanding of their disease and its treatment is desirable to enhance patient participation.
Angina is the most common presentation of coronary heart disease (CHD).1 Effective treatment requires appropriate medical care, but also patient participation in lifestyle changes and medication concordance. Patient understanding of their disease and its treatment is desirable to enhance patient participation.
Angina may be treated with medication only, through percutaneous coronary intervention (PCI) or coronary artery bypass surgery (CABG). Although there are some circumstances where there is a preferred treatment option, research increasingly shows that in many situations the different treatment options for angina have similar long-term outcomes.2 Therefore, the opinion of an informed patient is not only good medical practice but increasingly important to support decisions about their care. At present, there are few data on patients’ understanding of the pathophysiology of angina and the treatment options. We designed this study to investigate patients’ understanding of angina and their knowledge and participation in decisions about their treatment.
Methods
Consecutive patients newly attending the Cardiac Prevention and Rehabilitation Service (CPRS) at Imperial College Hospitals NHS Trust were invited to participate. The CPRS sees all first presentations of coronary artery disease within the trust. The only exclusion was patients who had received primary PCI treatment for ST elevation myocardial infarction, because PCI is the proven most effective treatment and the emergent nature means patient education may sometimes, of necessity, be limited. Since we wished to explore knowledge and understanding we chose a qualitative methodology using semi-structured interviews based on open-ended questions.3 All patients approached agreed to participate. Semi-structured interview method is the most widely used form of interview method in qualitative research.4 All were interviewed in their first out-patient appointment at the CPRS. The interviews lasted approximately 25–30 minutes. Conducted interviews were undertaken using initially open-ended questions with follow-up questioning used, as appropriate, to gain understanding of the interviewees answers.
All interviews were conducted in the same conditions; patients were seen at the same point during their first appointment at the CPRS.
Interviews were conducted before education sessions, so their baseline knowledge and understanding of angina and options for revascularisation were measured and assessed. Detailed handwritten notes were made for subsequent analysis.
In accordance with techniques used in
action research, review of the questionnaire was carried out after one interview and a further review after three.5 The details of patients were sent to a consultant cardiologist (KF), to confirm what they had mentioned during the interview matched their patient file and to confirm what type of treatment they had received.
Findings
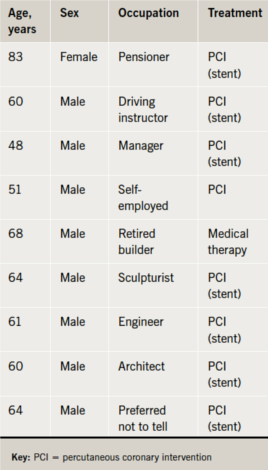
The interviewed patients consisted of eight males and one female. Age range was 48–83 years (table 1).
Patient knowledge about angina
You have been treated for coronary artery disease – may I ask what you understand by the condition?
No patient had a good understanding of angina. Most knew that the coronary arteries had narrowed due to lifestyle, however, they were not sure of where the artery was supplying the blood or what its function was. An indicative quote was “Artery is narrowed”, but when followed up by asking about the function of that artery, “takes blood somewhere in the body”. This poor physiological knowledge was common.
How did you learn about these treatments?
All patients have said they learnt about the treatments and options through doctors and nurses. However, other sources from where patients gained information were explored. Patients had acquired the most knowledge (other than doctors and nurses) through family and friends. Three patients mentioned that they used the internet to research other options (figure 1).
Treatment received
What treatment did you receive?
Interviewed patients were treated with the following strategies: PCI and medical therapy (table 1). However, patients lacked perception on the name of the procedures. The answers varied from describing stents as “umbrellas” to “lithium mesh tubes”. Endarterectomy was described by one patient as “hoovering out the blockage”.
Choice of treatment
Was just one treatment option explained to you, or were different types of treatments explained?
With almost all patients the method recommended by the doctor was explained, other treatments were mentioned but not in depth. This caused a lack of perception among patients on different options for revascularisation. A sample quote was “Other options were mentioned but only briefly by the doctor”. This was the common answer received from four out of nine patients where other options were mentioned but not explained in full. Five out of nine patients stated that no other option was explained. One patient stated “To aid my curiosity on other methods I searched the internet for more information”.
Who explained this to you?
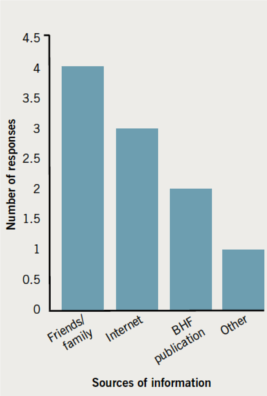
All patients said that the doctor explained the methods of revascularisation, with some mentioning nurses alongside doctors. However, three patients mentioned that they used the internet to gain further information. Two other patients also mentioned the British Heart Foundation booklets as good sources of information (figure 1).
May I ask a little more detail about what was explained to you?
Patients were explained the procedure most suitable to them, so in the case of angioplasty the procedure was explained in full together with benefits and why it was done. The duration, together with recovery time and complications that may arise, were explained. However, all patients failed to give a detailed answer to what was explained.
Choice of treatment where more than one option was offered
Was one treatment suggested as the right one for you?
All patients mentioned a doctor recommending one treatment option and briefly mentioning others.
Were you offered more than one treatment option and asked to choose?
Patients whom had the choice, chose to accept the doctor’s recommendation as they did not take an active part in the decision-making process.
How were the options explained?
Risks and benefits were explained to the patients together with complications that may arise during or after the procedure. Patients were happy in general with the information they received about the procedure.
Who talked to you about this?
All patients stated that this was the doctor.
Tell us about the final choice – did you make this, was it joint with the doctors, did they suggest a preferred option?
Most patients made their choice joint with doctors (five out of nine). However, four out of nine had no part in the decision-making process and left it completely to doctors from start to finish. Doctor’s preference was seen as correct so, hence, they accepted it as such. One patient stated “Left it completely to doctors, I wouldn’t know I am not a doctor.”
Overall perception of treatment
How do you feel about the way your treatment was chosen (good or not so good comments are very welcome)?
All patients, regardless of how much information they received and their perception, were happy with the way their treatment method was chosen.
Finally, is there anything else you want to add about any of the things we have talked about?
All patients were happy with the procedure and made it clear that they were happy with the care and information they received. “Very happy with all the team.”
However, one patient asked about the latest research on revascularisation and more information regarding latest breakthroughs in the field. Some specific questions were later forwarded to their consultant for an answer.
Summary
In summary, the following themes emerged:
- One revascularisation method is explained in detail to patients. However, other options are mentioned but only briefly.
- Normally, the one option mentioned in detail is the option that is recommended by the doctor.
- The way information is given to patients appears to follow a standard pattern, and is not tailored towards individual needs.
- Despite everything, patients are happy with their treatment, choice and care, and this is independent of their knowledge level.
- Only two patients played an active role in the decision-making process. The two patients who did take part in the decision-making process were the ones with the highest level of knowledge and understanding.
- Older patients had lower levels of knowledge and understanding and less role in the decision-making process.
Discussion
This study has shown that patient’s knowledge of angina is poor, and their knowledge and participation in choice of treatment limited, but this does not alter their high levels of satisfaction with the care they received.
The technique of qualitative research conducted through focused semi-structured interviews combined with an iterative process of question modification is ideally suited to establish patient’s knowledge and perception of the management of angina. This methodology is widely used, for example in the field of cardiology, and was chosen to understand patient and carers perceptions of end-of-life care in heart failure,5 and the primary care attitudes to a rapid access cardiology service.6
Patients’ understanding of the disease process and why certain treatments are applied in each case facilitates a balanced decision on options if treatment choice is available.7 Furthermore, if the patients are not informed, it would be unreasonable to expect them to adopt the lifestyle modifications that are essential in terms of prevention of disease progression. Knowledge and participation in decision making impacts on outcomes, this was demonstrated in a study by Brady et al.8 Patients were categorised either as playing an ‘active’ or ‘passive’ role in the decision-making process of treatment. In follow-up, ‘active’ patients reported less discomfort and more improvement in their general medical condition compared with ‘passive’ patients. Woolf et al. also showed that patients who are more involved in the decision-making process are likely to experience better outcomes.9
Other studies have identified knowledge gaps about angina and its treatment among patients. In a study by Haugbolle et al.7, one-third of the patients said that they knew nothing at all about angina. Patient understanding of benefits and risks of invasive procedures was measured in a study of 633 patients who had been offered CABG or PCI. Patients responded to questions regarding risks and benefits of each procedure and their perception of risks and benefits was analysed. Overall, patients were more optimistic than physicians about the benefits of revascularisation: 83% of the patients expected the revascularisation method to alleviate their symptoms and improve survival. However, this was different to expectations of the physicians: their expectation was that revascularisation would alleviate the symptoms in 76% of the patients and improve survival in 53%.7 Similarly, Rothberg et al.10 showed that 88% of patients thought PCI would reduce their risk of myocardial infarction.
From our interviews, one of the major themes was a lack of patient understanding of the heart and circulation. While patients all knew and could repeat that their artery was narrowed or blocked, they did not entirely know what an artery was or did. This highlights the strong need to assess baseline knowledge. Some patients had the thought a PCI was a quick fix and a simplified version of a CABG and were unaware that they had to change their lifestyle in order to prevent further adverse events (interviews were conducted prior to the rehabilitation programme education sessions). We did not explore their knowledge of lifestyle changes as this study focused on choices for revascularisation and the CPRS focused heavily on lifestyle education and change. In the absence of information, patients researched for themselves, including using the internet, where information is of uncertain quality and accuracy. Some patients also mentioned the use of British Heart Foundation booklets for understanding different options for revascularisation. Patients will fill a vacuum of information and it is important we provide it personally or through quality assured sources.
Typically, one revascularisation option was explained, and this was done by their physician, which may create a possible bias towards physician performed interventional cardiology options (PCI).
A key finding of this study was that patients, regardless of their perception of the different options available, were happy with the treatment they had received and were not complaining about lack of information. There are important limitations to the study and its methodology. The need for detailed interviewing means that the number of subjects is reduced. The lack of quantitative data limits (but does not exclude) statistical analysis. There were also situations whereby patients found it difficult to recall the advice of doctors or nurses, so, hence, some may also forget that doctors did explain the other options for revascularisation.
Conclusion
Patients’ knowledge of the pathophysiology of angina is limited. While they are given information about the particular treatment option assigned to them, they are much less informed about other options. This does not impact on the high levels of patient satisfaction with their care but may adversely effect participation in long-term prevention of progression of their coronary artery disease.
Acknowledgements
I would like to thank the staff of the CPRS at Imperial College for their support. The authors of this manuscript have certified that they comply with the Principles of Ethical Publishing in the British Journal of Cardiology.
Conflict of interest
None declared.
Key messages
- Patients’ understanding of the pathophysiology of angina is limited
- Patients typically receive information about the physician’s recommended form of revascularisation with limited information about other options
- Patients are generally happy with their care and the information they receive
References
- World Health Organization. Cardiovascular prevention and control. Available from: http://www.who.int/dietphysicalactivity/publications/facts/cvd/en/ [accessed 2 July 2010].
- Serruys PW, Morice MC, Kappetein AP et al. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N Engl J Med 2009;360:961–72. http://dx.doi.org/10.1056/NEJMoa0804626
- Sutcliffe JS, Fox KF, Wood DA et al. Incidence of coronary heart disease in a health authority in London review of a community register. BMJ 2003;326:20. http://dx.doi.org/10.1136/bmj.326.7379.20
- DiCicco-Bloom B, Grabtree FB. The qualitative research interview. Med Educ 2006;40:314–21. http://dx.doi.org/10.1111/j.1365-2929.2006.02418.x
- Rogers AE, Addington-Hall JM, Abery AJ et al. Knowledge and communication difficulties for patients with chronic heart failure: qualitative study. BMJ 2008;321:605–07. http://dx.doi.org/10.1136/bmj.321.7261.605
- Fox KF, Tenkorang J, Rogers A, Wood DA. Are rapid access cardiology clinics a valued part of a district cardiology service? Int J Cardiol 2009;137:42–6. http://dx.doi.org/10.1016/j.ijcard.2008.06.026
- Haugbolle LS, Sorensen WE, Herborg H, Henriksen HH. Medication and illness-related factual knowledge, perceptions and behaviour in angina pectoris patients. Patient Educ Couns 2001;47:281–9. http://dx.doi.org/10.1016/S0738-3991(01)00229-4
- Brady DS, Miller SM, Lerman CE. Patient perception of involvement in medical care: relationship to illness attitudes and outcomes. J Gen Intern Med 1989;4:506–11.
- Woolf SH, Chan EC, Harris R. Promoting informed choice: transforming health care to dispense knowledge for decision making. Ann Intern Med 2005;143:293–300.
- Rothberg M, Sivalingham SK, Ashraf J et al. Patients’ and cardiologists’ perceptions of the benefits of percutaneous coronary intervention for stable coronary disease. Ann Intern Med 2010;153:307–13.
