Draft guidance on statins
The National Institute for Health and Care Excellence (NICE) is recommending that the threshold for starting statins for the preventive treatment of cardiovascular disease (CVD) is halved from a 20% risk of developing CVD over 10 years to a 10% risk. This draft guidance – an update on its 2008 lipid modification guidance – follows new evidence for CVD risk assessment tools and the availability of generic statins.
According to NICE, CVD is still the leading cause of death in England and Wales, accounting for one in three deaths in the UK despite the huge fall in CVD death rates since the 1970s.
The draft guidance is currently out for public consultation. Key recommendations include:
- Using a systematic strategy to identify people aged 40–74 likely to be at high risk for the primary prevention of CVD in primary care.
- Using the QRISK2 risk assessment tool to assess CVD risk in primary prevention.
- Routinely recording ethnicity, body mass index and family history of premature CVD in medical records.
Before starting lipid modification therapy for the primary prevention of CVD, taking at least one lipid sample to measure a full lipid profile. This should include measurement of total cholesterol, high-density lipoprotein (HDL) cholesterol, non-HDL cholesterol, and triglyceride concentrations. A fasting sample is not needed.
Offering a high-intensity statin treatment for the primary prevention of CVD to people who have a 10% or greater 10-year risk of developing CVD. Estimate the level of risk using the QRISK2 assessment tool.
Offering statin treatment for the primary prevention of CVD with atorvastatin 20 mg.
Starting statin treatment in people with established CVD, type 1 diabetes or type 2 diabetes with atorvastatin 80 mg. Using a lower dose of atorvastatin If there are potential drug interactions, risk of adverse effects, comorbidities, or patient preference.
Post-MI guidance updated
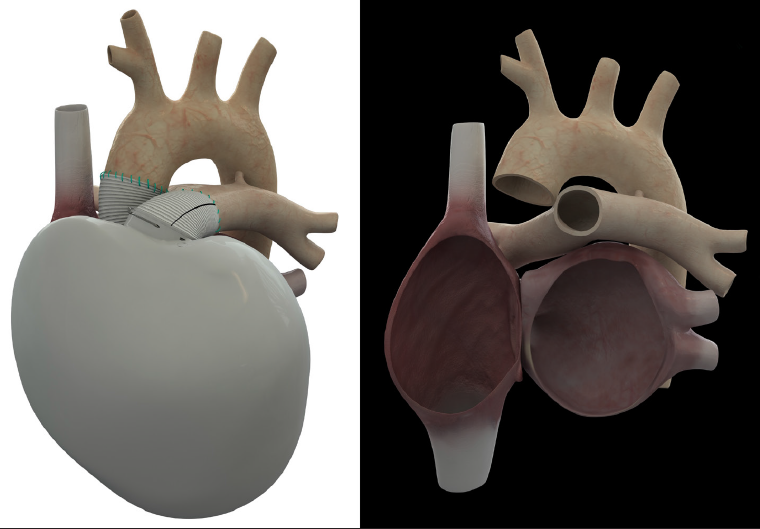
The National Institute for Health and Care Excellence (NICE) has updated its secondary prevention of myocardial infarction (MI) guidance.
Clinical guidelines CG172 replace NICE clinical guideline 48, published in 2007. The new guidelines reflect major changes in the treatment of acute MI, ST-elevation MI (STEMI) and non-ST-elevation MI (NSTEMI), particularly the use of primary percutaneous coronary intervention which has replaced thrombolysis in most cases of STEMI.
Key factors for implementation include:
- Improving uptake of cardiac rehabilitation programmes which are currently only started by 46% of people post-MI.
- Offering all people who have had an acute MI, angiotensin-converting enzyme (ACE) inhibitors, dual antiplatelet therapy, beta blockers, and statins; and titrating doses where necessary.
- Offering an assessment of left ventricular function to all people post-MI.
- No longer recommending eating oily fish or omega-3 capsules/supplements to prevent further MI.
- Recommending a Mediterranean-style diet.
- Stressing the importance of lifestyle changes including encouraging exercise for 20-30 minutes daily.
The draft guidance on statins is available at http://guidance.nice.org.uk/CG/WaveR/123
The full guidance on secondary prevention of myocardial infarction is available at http://guidance/nice.org.uk/CG172