Statins are ‘HMG-CoA reductase’ (3-hydroxy-3-methylglutaryl-CoA reductase) inhibitors and attenuate the intracellular levels of cholesterol. By virtue of their multiple pleiotropic modes of action in cardiovascular diseases, statins have also been considered and used for treating various other disorders, with convincing beneficial results, though a few contradictory reports do exist. Taking into account the positive and negative effects of statins, the data need to be viewed with a ‘pinch of salt’ for statins to be labelled as wonder drugs.
Introduction
 Since their discovery in the 1970s, statins are widely used in clinics for the treatment of atherosclerosis and other cardiovascular diseases (CVD). Statins attenuate the intracellular levels of cholesterol by inhibiting the rate-limiting enzyme 3-hydroxy-3-methylglutaryl (HMG)-CoA reductase, either by competing with the normal substrate in the enzyme’s active site, or by altering the conformation of the enzyme by binding to its active site.
Since their discovery in the 1970s, statins are widely used in clinics for the treatment of atherosclerosis and other cardiovascular diseases (CVD). Statins attenuate the intracellular levels of cholesterol by inhibiting the rate-limiting enzyme 3-hydroxy-3-methylglutaryl (HMG)-CoA reductase, either by competing with the normal substrate in the enzyme’s active site, or by altering the conformation of the enzyme by binding to its active site.
Lipid-mediated effects
Statins exert their lipid-mediated action by decreasing the production of cholesterol and low-density lipoproteins (LDL), by up-regulation of LDL-receptors and uptake of circulatory LDL. Reduction in intracellular cholesterol induces activation of a protease, causing release of sterol regulatory element binding proteins (SREBPs) from the endoplasmic reticulum. SREBPs are then translocated to the nucleus, where they increase the expression of the LDL-receptor gene that controls the cholesterol homeostasis.1,2
Extended follow-up of the Heart Protection Study (HPS) documented long-term efficacy and safety of lowering LDL-cholesterol (LDL-C) with statins, in 20,536 patients who were at high risk of vascular and non-vascular outcomes with 40 mg simvastatin.3 Atorvastatin at high pharmacologic dose increased LDL-receptor-related protein 1 (LRP1) in both in vitro and in vivo studies.4 Statins further reduce the oxidation of LDL and, thereby, inhibit foam cell formation. Early atorvastatin therapy in 2,341 inpatients after acute coronary syndrome (ACS) was shown to significantly enhance mobilisation and clearance of oxidised phospholipids (OxPL) from the arterial wall,5 and statin therapy was also shown to be an independent predictor of low oxidised LDL (OxLDL) levels in 687 patients with angiographically proven CAD by multi-variable analysis.6
Statins vary in their high-density lipoprotein (HDL)-cholesterol (HDL-C) raising ability. Rosuvastatin and simvastatin demonstrated a positive relation with HDL-C, but the same was not applicable for atorvastatin.7 The increase in HDL-C levels is mediated by reductions in cholesteryl ester transfer protein (CETP) activity.8 Recently, it was shown that for potent statin therapy, instead of chemical assay for HDL-C, HDL particle number may be a better marker of residual risk after statin therapy.9 A post-hoc analysis of intravascular ultrasound data from 1,455 people showed that statin-associated changes in HDL-C were inversely associated with the progression of coronary atherosclerosis, even in patients with low levels of LDL-C via stimulation of the ‘reverse cholesterol transport’ pathway.10,11
Non-lipid-mediated pleiotropic effects
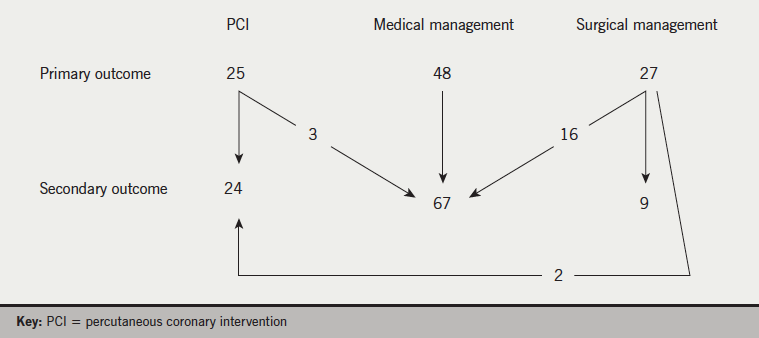
Statins empower multiple pleiotropic modes of action (figure 1), independent of lipid-mediated effects, mediated by their ability to block the generation of isoprenoid intermediates like farensyl pyrophosphate (FPP) and geranyl-geranylphosphate (GGPP) in vascular cells, which serve as lipid attachments for a variety of intracellular signalling molecules, like Rab and Rho.

Rho activates a number of nuclear transcription factors such as nuclear factor-kappa B, and reduces endothelial nitric oxide synthetase (eNOS). Statins up-regulate eNOS by inhibiting Rho, and also inhibit the 5-lipoxygenase (5-LO) pathway and chemokine CCL3, thereby, curbing inflammatory processes in atherosclerosis.12 Activation of sphingosine-1-phosphate (S1P) signalling via up-regulation of S1P receptor expression,13 and up-regulation of small GTP-binding protein GDP dissociation stimulator (SmgGDS) followed by Rac1 degradation due to statins, may also account for the pleiotropic effects of statins.14
Various in vivo and in vitro studies, as well as human clinical trials, have successfully demonstrated that statins reduce cardiovascular events,15,16 diabetes,17 progression of nephropathy18 and fracture rates.19 Simvastatin treatment significantly decreased frequency and occurrence of mammary tumours in chemo-carcinogen induced mammary tumours in rats.20 Important pleiotropic and cardioprotective effects of statins could be visualised as improvement in endothelial dysfunction, anti-oxidant, anti-inflammatory and antithrombotic effects, and their ability to up-regulate mitophagy, autophagy and down-regulation of Akt/mTOR signalling.21 Statins benefit in hypertension due to their role in maintaining endothelial function and their interaction with the renin–angiotensin system.22 Statins attenuate occurrence of pulmonary hypertension via the RhoA/Rho-kinase signalling pathway.23 Atorvastatin at a dose of 80 mg and a 50% LDL-C reduction showed large effects on blood pressure, whereas lesser effects were seen in other studies where LDL-C reductions were smaller.24,25 In a cross-sectional study of 2,584 hypertensive adults aged 40 years and older with no known CVD, statin-medicated subjects significantly had their blood pressure under control.26 The Study to Evaluate the Effect of Rosuvastatin on Intravascular Ultrasound-Derived Coronary Atheroma Burden (ASTEROID) demonstrated that rosuvastatin therapy resulted in significant regression of atherosclerosis in patients with CAD, 95% of whom had a history of hypertension.27 However, controversial reports do exist, as the Cholesterol and Recurrent Events (CARE) trial documented that pravastatin in a dose of 40 mg had no significant effects on blood pressure in 4,128 patients.28 In the Plaque Hypertension Lipid-Lowering Italian Study (PHYLLIS) trial, pravastatin did not demonstrate additional blood pressure-lowering effect29 in hypertensive hypercholesterolaemics.
The West of Scotland Coronary Prevention Study (WOSCOPS) showed that pravastatin therapy reduced the risk of type 2 diabetes mellitus (T2DM) by 30%.30 Subgroup analysis of the Scandinavian Simvastatin Survival Study (4S) demonstrated that cholesterol lowering with simvastatin improved prognosis of diabetic patients with coronary heart disease.31 Simvastatin had a favourable effect on leukocyte activation markers in patients with T2DM.32 Meta-analysis of 10 placebo-controlled trials, with 16,000 patients who had diabetes and 54,000 subjects without diabetes, demonstrated a 30% reduction in coronary heart disease and a 12% reduction in mortality.33 Results of the Collaborative Atorvastatin Diabetes Study (CARDS) showed that atorvastatin inhibited the development of CVD in diabetics.34
Contradictory reports also exist, wherein administration of statins lead to onset of diabetes. Rosuvastatin increased the hazard ratio for newly diagnosed diabetes by 25% versus a placebo group.35 A meta-analysis of 13 randomised statin trials with 91,140 participants demonstrated an odds ratio of 1.09 for incident diabetes.36 Annual rates of diabetes were shown to be significantly higher in statin users versus control subjects.37 Also, administration of atorvastatin, rosuvastatin and simvastatin to patients without diabetes increased the risk of incident diabetes, regardless of whether statins were used for primary or secondary prevention of CVD.38
Though these drugs have shown encouraging beneficial results in the primary and secondary prevention of CVD, there is a considerable residual risk in patients receiving statins, for example in the 4S study, where statins reduced the death rate only by 30%, which leaves a considerable number of patients still at risk of events. However, it has been safely documented that statin use among people without evidence of CVD reduced all-cause mortality and other major vascular events without any adverse outcomes.
Effect of statins in other disorders
Besides their role in CVD, statins are reported to play a crucial role in other diseases as well. Both in vitro and in vivo studies demonstrate that statin use results in a significant reduction in different forms of cancer by inducing apoptosis and cell growth.39 Further, the addition of statins to the therapeutic regimen has allowed for the use of lower doses of chemotherapeutic drugs, resulting in milder side effects.40 However, a few trials41 demonstrated no significant differences in the percentage of cancer cases in patients treated with simvastatin or atorvastatin.42 In a retrospective analysis in 1,117 non-muscle-invasive bladder cancer (NMIBC) patients, statin use was not related to regression, recurrence or cancer specific mortality.43
Statins are shown to attenuate renal injury in both in vivo and in vitro studies.44 Statins ameliorated structural and functional changes of diabetic nephropathy in diabetic rat models.45,46 A meta-analysis with 39,704 subjects reported that statins reduced the rate of renal function loss by 76%.47 In non-diabetic patients with chronic kidney disease, statins improved the tubular status,48 reduced urinary albumin excretion,18 urinary podocyte number and proteinuria, which benefited patients with chronic glomerulonephritis (CGN).49
By virtue of their anti-inflammatory and immunomodulatory properties, statins have also drawn much attention as promising agents in the treatment of many disorders, e.g. rheumatic disease, multiple sclerosis, uveitis, colitis, autoimmune encephalomyelitis and systemic lupus erythematosus.50,51
Negative effects
Considering the overall positive impacts and pleiotropic effects of statins, it may be fair to think that statins are a benefit to society and could easily pass as a cure-all drug, but one also needs to consider their side effects. Numerous pleiotropic effects of statins may add to desirable or undesirable effects. Statins bear the same mode of action, but differ between each other in the extent of lowering LDL-cholesterol. Due to limited cholesterol synthesis, other important inflammatory proteins, endogenous synthesis of coenzyme Q10 and selenoproteins are also inhibited. Evidence from experimental and human studies also suggests that statin withdrawal rapidly abrogates the beneficial effects of statins, and results in rebound inflammation, increased Rho activity, reduced endothelial NO production, increased C-reactive protein (CRP) and induces prothrombotic pathways.52-56The Controlled Rosuvastatin Multi-national Study in Heart Failure (CORONA), Gruppo Italiano per lo Studio della Sopravvivenza nell’Infarto Miocardico – Heart Failure (GISSI-HF) and A Study to Evaluate the Use of Rosuvastatin in Subjects on Regular Haemodialysis – An Assessment of Survival and Cardiovascular Events (AURORA) trials yielded unexpected negative results, wherein, statin administration showed adverse effects in patients with heart failure.57,58
Data from 14 randomised controlled trials has also demonstrated that in people with low cardiovascular risk, caution is needed while prescribing statins for primary prevention use as there was evidence of failure in reporting adverse events, selective reporting of outcomes, and inclusion of people with cardiovascular disease.59 Furthermore, another meta-analysis with the primary objective of investigating all-cause mortality in a high-risk primary prevention set up reported no benefit of statin therapy.60
Conclusion
In summary, accumulating evidence from basic research and clinical trials document that statins have pleotropic effects and, in addition to their applicability in cardiovascular diseases, mark their use in various other diseases as well. Data from large randomised clinical trials clearly demonstrate that statin use results in reduced all-cause mortality, and reduction in clinical end points, such as major vascular events and revascularisation with limited adverse effects. Evidence also shows statins to be cost-effective and of benefit in improving quality of life in primary prevention in people with low cardiovascular risk. Some side effects, such as risk of incident diabetes, increased activity in liver enzymes, (e.g. hepatic transaminases and myopathy) should be re-evaulated in randomised and controlled population-based large trials.
Conflict of interest
None declared.
Key messages
- Statins are effective in primary and secondary prevention of cardiovascular disease and significantly reduce the risk of major cardiovascular events without significant adverse outcomes
- Studies, however, exist, wherein statin therapy has been associated with a small increased risk of new-onset diabetes, and muscle pain with no significant effects on blood pressure
References
1. Paumelle R, Staels B. Peroxisome proliferator-activated receptors mediate pleiotropic actions of statins. Circ Res 2007;100:1394–5. http://dx.doi.org/10.1161/01.RES.0000269334.42814.d2
2. Sehayek E, Butbul E, Avner R, Levkovitz H, Eisenberg S. Enhanced cellular metabolism of very low density lipoprotein by simvastatin. A novel mechanism of action of HMG-CoA reductase inhibitors. Eur J Clin Invest 1994;24:173–8. http://dx.doi.org/10.1111/j.1365-2362.1994.tb00984.x
3. Heart Protection Study Collaborative Group, Bulbulia R, Bowman L et al. Effects on 11-year mortality and morbidity of lowering LDL cholesterol with simvastatin for about 5 years in 20,536 high-risk individuals: a randomised controlled trial. Lancet 2011;378:2013–20. http://dx.doi.org/10.1016/S0140-6736(11)61125-2
4. Moon JH, Kang SB, Park JS et al. Up-regulation of hepatic low-density lipoprotein receptor-related protein 1: a possible novel mechanism of antiatherogenic activity of hydroxyl methylglutaryl-coenzyme A reductase inhibitor atorvastatin and hepatic LRP1 expression. Metabolism 2011;60:930–40. http://dx.doi.org/10.1016/j.metabol.2010.08.013
5. Tsimikas S, Witztum JL, Miller ER et al. High-dose atorvastatin reduces total plasma levels of oxidized phospholipids and immune complexes present on apolipoprotein B-100 in patients with acute coronary syndromes in the MIRACL trial. Circulation 2004;110:1406–12. http://dx.doi.org/10.1161/ 01.CIR.0000141728.23033.B5
6. Ndrepepa G, Braun S, Beckerath N et al. Oxidized low density lipoproteins, statin therapy and severity of coronary artery disease. Clin Chim Acta 2005;360:178–86. http://dx.doi.org/10.1016/j.cccn.2005.04.032
7. Barter PJ, Brandrup-Wognsen G, Palmer MK, Nicholls SJ. Effect of statins on HDL-C: a complex process unrelated to changes in LDL-C. Analysis of the VOYAGER database. J Lipid Res 2010;51:1546–53. http://dx.doi.org/10.1194/jlr.P002816
8. McTaggart F, Jones P. Effects of statins on high-density lipoproteins: a potential contribution to cardiovascular benefit. Cardiovasc Drugs Ther 2008;22:321–38. http://dx.doi.org/10.1007/s10557-008-6113-z
9. Mora S, Glynn RJ, Ridker PM. High-density lipoprotein cholesterol, size, particle number, and residual vascular risk after potent statin therapy. Circulation 2013;128:1189–97. http://dx.doi.org/10.1161/CIRCULATIONAHA.113.002671
10. Kontush A, Chapman MJ. Antiatherogenic small, dense HDL – guardian angel of the arterial wall? Nat Clin Pract Cardiovasc Med 2006;3:144–53. http://dx.doi.org/10.1038/ncpcardio0500
11. Nicholls SJ, Tuzcu EM, Sipahi I et al. Statins, high-density lipoprotein cholesterol, and regression of coronary atherosclerosis. JAMA 2007;297:499–508. http://dx.doi.org/10.1001/jama.297.5.499
12. Yang LX, Heng XH, Guo RW et al. Atorvastatin inhibits the 5-lipoxygenase pathway and expression of CCL3 to alleviate atherosclerotic lesions in atherosclerotic ApoE knockout mice. J Cardiovasc Pharmacol 2013;62:205–11. http://dx.doi.org/10.1097/FJC.0b013e3182967fc0
13. Egom EE, Rose RA, Neyses L, Soran H, Cleland JG, Mamas MA. Activation of sphingosine-1-phosphate signalling as a potential underlying mechanism of the pleiotropic effects of statin therapy. Crit Rev Clin Lab Sci 2013;50:79–89. http://dx.doi.org/10.3109/10408363.2013.813013
14. Tanaka S, Fukumoto Y, Nochioka K et al. Statins exert the pleiotropic effects through small GTP-binding protein dissociation stimulator upregulation with a resultant Rac1 degradation. Arterioscler Thromb Vasc Biol 2013;33:1591–600. http://dx.doi.org/10.1161/ATVBAHA.112.300922
15. Scandinavian Simvastatin Survival Study Group.Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study (4S). Lancet 1994;344:1383–9. http://dx.doi.org/10.1016/S0140-6736(94)90566-5
16. Shepherd J, Cobbe SM, Ford I et al. Prevention of coronary heart disease with pravastatin in men with hypercholesterolemia. West of Scotland Coronary Prevention Study Group. N Engl J Med 1995;333:1301–07. http://dx.doi.org/10.1056/NEJM199511163332001
17. Freeman DJ, Norrie J, Sattar N et al. Pravastatin and the development of diabetes mellitus: evidence for a protective treatment effect in the West of Scotland Coronary Prevention Study. Circulation 2001;103:357–62. http://dx.doi.org/10.1161/01.CIR.103.3.357
18. Tonolo G, Melis MG, Formato M et al. Additive effects of simvastatin beyond its effects on LDL cholesterol in hypertensive type 2 diabetic patients. Eur J Clin Invest 2000;30:980–7. http://dx.doi.org/10.1046/j.1365-2362.2000.00735.x
19. Meier CR, Schlienger RG, Kraenzlin ME, Schlegel B, Jick H. HMG-CoA reductase inhibitors and the risk of fractures. JAMA 2000;283:3205–10. http://dx.doi.org/10.1001/jama.283.24.3205
20. Kubatka P, Kajo K, Zihlavnikova K et al. Immunohistochemical and histomorphological analysis of rat mammary tumors after simvastatin treatment. Neoplasma 2012;59:516–23. http://dx.doi.org/10.4149/neo_2012_066
21. Andres AM, Hernandez G, Lee P et al. Mitophagy is required for acute cardioprotection by simvastatin. Antioxid Redox Signal 2013;published online. http://dx.doi.org/10.1089/ars.2013.5416
22. Straznicky NE, Howes LG, Lam W, Louis WJ. Effects of pravastatin on cardiovascular reactivity to norepinephrine and angiotensin II in patients with hypercholesterolemia and systemic hypertension. Am J Cardiol 1995;75:582–6. http://dx.doi.org/10.1016/S0002-9149(99)80621-3
23. Xing XQ, Gan Y, Wu SJ et al. Statins may ameliorate pulmonary hypertension via RhoA/Rho-kinase signaling pathway. Med Hypotheses 2007;68:1108–13. http://dx.doi.org/10.1016/j.mehy.2006.09.034
24. Ferrier KE, Muhlmann MH, Baguet JP et al. Intensive cholesterol reduction lowers blood pressure and large artery stiffness in isolated systolic hypertension. J Am Coll Cardiol 2002;39:1020–5. http://dx.doi.org/10.1016/S0735-1097(02)01717-5
25. Glorioso N, Troffa C, Filigheddu F et al. Effect of the HMG-CoA reductase inhibitors on blood pressure in patients with essential hypertension and primary hypercholesterolemia. Hypertension 1999;34:1281–6. http://dx.doi.org/10.1161/01.HYP.34.6.1281
26. King DE, Mainous AG, Egan BM, Player M, Geesey ME. The use of statins and blood pressure. Am J Hypertens 2007;20:937–41. http://dx.doi.org/10.1016/j.amjhyper.2007.03.018
27. Nissen SE, Nicholls SJ, Sipahi I et al. Effect of very high-intensity statin therapy on regression of coronary atherosclerosis: the ASTEROID trial. JAMA 2006;295:1556–65. http://dx.doi.org/10.1001/jama.295.13.jpc60002
28. Tonelli M, Isles C, Curhan GC et al. Effect of pravastatin on cardiovascular events in people with chronic kidney disease. Circulation 2004;110:1557–63. http://dx.doi.org/10.1161/01.CIR.0000143892.84582.60
29. Mancia G, Parati G, Revera M et al. Statins, antihypertensive treatment, and blood pressure control in clinic and over 24 hours: evidence from PHYLLIS randomised double blind trial. BMJ 2010;340:c1197. http://dx.doi.org/10.1136/bmj.c1197
30. Freeman DJ, Norrie J, Sattar N. Pravastatin and the development of diabetes mellitus: evidence for a protective treatment effect in the West of Scotland Coronary Prevention Study. Circulation 2001;103:357–62. http://dx.doi.org/10.1161/01.CIR.103.3.357
31. Pyorala K, Pedersen TR, Kjekshus J, Faergeman O, Olsson AG, Thorgeirsson G. Cholesterol lowering with simvastatin improves prognosis of diabetic patients with coronary heart disease: a subgroup analysis of the Scandinavian Simvastatin Survival Study (4S). Diabetes Care 1997;20:614–20.
32. Stulc T, Ceska R, Marinov I, Skrha J. The effect of simvastatin and fenofibrate on the expression of leukocyte adhesion molecules and lipopolysaccharide receptor CD14 in type 2 diabetes mellitus. Neuro Endocrinol Lett 2012;33(suppl 2):73–7.
33. Brugts JJ, Yetgin T, Hoeks SE et al. The benefits of statins in people without established cardiovascular disease but with cardiovascular risk factors: meta-analysis of randomised controlled trials. BMJ 2009;338:b2376. http://dx.doi.org/10.1136/bmj.b2376
34. Colhoun CM, Betteridge DJ, Durrington PN et al. Primary prevention of cardiovascular disease with atorvastatin in type 2 diabetes in the Collaborative Atorvastatin Diabetes Study (CARDS): multicentre randomised placebo-controlled trial. Lancet 2004;364:685–96. http://dx.doi.org/10.1016/S0140-6736(04)16895-5
35. Ridker PM, Danielson E, Fonseca FA et al. Rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein. N Engl J Med 2008;359:2195–207. http://dx.doi.org/10.1056/NEJMoa0807646
36. Sattar N, Preiss D, Murray HM et al. Statins and risk of incident diabetes: a collaborative meta-analysis of randomised statin trials. Lancet 2010;375:735–42. http://dx.doi.org/10.1016/S0140-6736(09)61965-6
37. Wang KL, Liu CJ, Chao TF et al. Statins, risk of diabetes, and implications on outcomes in the general population. J Am Coll Cardiol 2012;60:1231–8. http://dx.doi.org/10.1016/j.jacc.2012.05.019
38. Carter AA, Gomes T, Camacho X, Juurlink DN, Shah BR, Mamdani MM. Risk of incident diabetes among patients treated with statins: population based study. BMJ 2013;346:f2610. http://dx.doi/org/10.1136/bmj.f2610
39. Kawata S, Yamasaki E, Nagase T et al. Effect of pravastatin on survival in patients with advanced hepatocellular carcinoma. A randomized controlled trial. Br J Cancer 2001;84:886–91. http://dx.doi.org/10.1054/bjoc.2000.1716
40. Agarwal B, Bhendwal S, Halmos B, Moss SF, Ramey WG, Holt PR. Lovastatin augments apoptosis induced by chemotherapeutic agents in colon cancer cells. Clin Cancer Res 1999;5:2223–9. Available from: http://clincancerres.aacrjournals.org/content/5/8/2223.full.pdf+html
41. Teo KK, Burton JR, Buller CE et al. Long-term effects of cholesterol lowering and angiotensin-converting enzyme inhibition on coronary atherosclerosis: the Simvastatin/Enalapril Coronary Atherosclerosis Trial (SCAT). Circulation 2000;102:1748–54. http://dx.doi.org/10.1161/ 01.CIR.102.15.1748
42. Pedersen TR, Faergeman O, Kastelein JJ et al. High-dose atorvastatin vs usual-dose simvastatin for secondary prevention after myocardial infarction: the IDEAL study: a randomized controlled trial. JAMA 2005;294:2437–45. http://dx.doi.org/10.1001/jama.294.19.2437
43. Crivelli JJ, Xylinas E, Kluth LA et al. Effect of statin use on outcomes of non-muscle-invasive bladder cancer. BJU Int 2013;112:E4–E12. http://dx.doi.org/10.1111/bju.12150
44. Mirzaii-Dizgah I, Salmanyan B. Renal function in a rat model of neurogenic bladder, effect of statins and phosphodiesterase-5 inhibitors. Eur Spine J 2013;22:2766–9. http://dx.doi.org/10.1007/s00586-013-2927-x
45. Yokota T, Utsunomiya K, Murakawa Y, Kurata H, Tajima N. Mechanism of preventive effect of HMG-CoA reductase inhibitor on diabetic nephropathy. Kidney Int Suppl 1999;71:S178-S181.
46. Usui H, Shikata K, Matsuda M et al. HMG-CoA reductase inhibitor ameliorates diabetic nephropathy by its pleiotropic effects in rats. Nephrol Dial Transplant 2003;18:265–72. http://dx.doi.org/10.1093/ndt/18.2.265
47. Sandhu S, Wiebe N, Fried LF, Tonelli M. Statins for improving renal outcomes: a meta-analysis. J Am Soc Nephrol 2006;17:2006–16. http://dx.doi.org/10.1681/ASN.2006010012
48. Renke M, Tylicki L, Rutkowski P et al. Atorvastatin improves tubular status in non-diabetic patients with chronic kidney disease – placebo controlled randomized, cross-over study. Acta Biochim Pol 2010;57:547–52. Available from: http://www.actabp.pl/pdf/4_2010/547.pdf
49. Nakamura T, Ushiyama C, Hirokawa K et al. Effect of cerivastatin on proteinuria and urinary podocytes in patients with chronic glomerulonephritis. Nephrol Dial Transplant 2002;17:798–802. http://dx.doi.org/10.1093/ndt/17.5.798
50. Mihos CG, Artola RT, Santana O. The pleiotropic effects of the hydroxy-methyl-glutaryl-CoA reductase inhibitors in rheumatologic disorders: a comprehensive review. Rheumatol Int 2012;32:287–94. http://dx.doi.org/10.1007/s00296-011-2008-6
51. Abeles AM, Pillinger MH. Statins as antiinflammatory and immunomodulatory agents: a future in rheumatologic therapy? Arthritis Rheum 2006;54:393–407. http://dx.doi.org/10.1002/art.21521
52. Grundy SM, Cleeman JI, Bairey Merz NC et al. Implications of recent clinical trials for the NCEP Adult Treatment Panel III Guidelines.J Am Coll Cardiol 2004;44:720–2. http://dx.doi.org/10.1016/j.jacc.2004.07.001
53. Kashani A, Phillips CO, Foody JM et al. Risks associated with statin therapy: a systematic overview of randomized clinical trials. Circulation 2006;114:2788–97. http://dx.doi.org/10.1161/CIRCULATIONAHA.106.624890
54. Baigent C, Landray MJ, Reith C et al. The effects of lowering LDL cholesterol with simvastatin plus ezetimibe in patients with chronic kidney disease (Study of Heart and Renal Protection): a randomised placebo-controlled trial. Lancet 2011;377:2181–92. http://dx.doi.org/10.1016/S0140-6736(11)60739-3
55. Lai WT, Lee KT, Chu CS et al. Influence of withdrawal of statin treatment on proinflammatory response and fibrinolytic activity in humans: an effect independent on cholesterol elevation. Int J Cardiol 2005;98:459–64. http://dx.doi.org/10.1016/j.ijcard.2003.11.023
56. Sposito AC, Carvalho LS, Cintra RM et al. Rebound inflammatory response during the acute phase of myocardial infarction after simvastatin withdrawal. Atherosclerosis 2009;207:191–4. http://dx.doi.org/10.1016/j.atherosclerosis.2009.04.008
57. Ridker PM. Statin therapy for low-LDL, high-hsCRP patients: from JUPITER to CORONA. Clin Chem 2010;56:505–07. http://dx.doi.org/10.1373/clinchem.2009.142653
58. Barrios V, Escobar C. Rosuvastatin along the cardiovascular continuum: from JUPITER to AURORA. Expert Rev Cardiovasc Ther 2009;7:1317–27. http://dx.doi.org/10.1586/erc.09.119
59. Taylor F, Ward K, Moore TH et al. Statins for the primary prevention of cardiovascular disease. Cochrane Database Syst Rev 2011;19:1:CD004816. http://dx.doi.org/10.1002/14651858.CD004816.pub5/
60. Ray KK, Seshasai SR, Erqou S et al. Statins and all-cause mortality in high-risk primary prevention: a meta-analysis of 11 randomized controlled trials involving 65,229 participants. Arch Intern Med 2010;170:1024–31. http://dx.doi.org/10.1001/archinternmed.2010.182/