Sustainability of health benefits from cardiac rehabilitation (CR) requires adequate changes in lifestyles. Preventive medicine highlights a triadic guideline referring to cardioprotective behaviour, avoidance of associated polymorbid developments (e.g. depression), and improvement of life-quality. To assess the influence of long-term CR management (in Austria phase 4) offered by the Austrian Heart Association (ÖHV) on changes in lifestyles according to the INTERHEART CHD-risk parameters, a questionnaire measuring the extent of phase 4 influences on lifestyle modifications according to the INTERHEART parameters physical activity, stress, nutrition, body mass index (BMI), smoking, and alcohol was developed. Data were gained from a non-preselected sample of cardiac patients with various diagnoses (n=204; age 41–91, average 71.8; standard variation 7.8, 48% cardiovascular).
ÖHV activities were found to exert a strong influence on health sports (various indoor and outdoor aerobic activities and mobility exercises), stress-reduction, and nutritional adjustment, contrasting low influence on the awareness of diabetes risks and alcohol/nicotine consumption. Social inclusion is considered an important life-quality factor supporting also the sense of security.
Long-term CR management is an efficient instrument for cardioprotective lifestyle modification. The important influence on patients requires especially high sports cardiologic standards and psycho-educational competence. Close collaboration between different phases/stages of CR, as well as similar international organisation should be fostered.
Introduction

In 2009, Willmer and Waite1 published a study on the effectiveness of phase 4 cardiac rehabilitation (CR), suggesting that there are observable benefits in participating in long-term phase 4 CR. Those who decline phase 4 CR clearly do less well. In Austria, the Austrian Heart Association (Österreichischer Herzverband/ÖHV) is in charge of long-term CR management providing a nationwide network of heart support groups.
Long-term management in CR: International heterogeneity
Cardiac prevention, acute cardiology, and CR are interacting disciplines. Historically speaking, it took decades to establish cardiac prevention awareness in the general population and to provide comprehensive CR services. After a ‘step change’ in one’s cardiac condition, such as myocardial infarction (MI), acute coronary heart disease (CHD) or first diagnosed heart failure and subsequent acute care, formerly patients were usually told to change their lifestyles and to protect their hearts, though clinicians could not give precise advice, e.g. concerning sports cardiologic guidelines, nor did patients find long-term support by specialised rehabilitation organisations. In Austria, this problem led to the foundation of the Austrian Heart Association approximately four decades ago.
Though in those early times there was doubt about the effectiveness of community-based long-term rehabilitation,2 today, long-term secondary prevention and heart support groups have become an international standard.3 Due to different health systems and medical credos in the world there is no standardised terminology in cardiac rehabilitation,4 a problem causing misunderstandings and restricting transferability.
The Austrian phase 4 is equivalent to stage 6 of the new UK stage model. American guidelines define three phases:5
- Inpatient CR (also known as phase 1 CR)
- Early outpatient CR (phase 2)
- Long-term outpatient CR (also known as phase 3 or phase 4 CR): a programme that provides longer-term delivery of preventive and rehabilitative services for patients in outpatient settings.
Other countries are reforming systems, e.g. China, which looks back to an outstandingly good healthcare practice, is today about to integrate traditional and Western approaches. Nevertheless, we also find very Western ways of CR, e.g. in Hong Kong.6 This programme consists of four phases:
- Inpatient ambulation programme for 7–14 days
- A twice-weekly outpatient education and exercise programme lasting for eight weeks
- A community-based home exercise programme
- Long-term maintenance for another 12 months.
Germany and Switzerland share similar systems, phase 1 referring to early mobilisation at hospital, phase 2 subsequent treatment in a CR clinic or in smaller specialised outpatient centres, phase 3 long-term rehabilitation in heart support groups.
In Austria, CR consists of four phases:
- Phase 1: acute hospital, early mobilisation and preparing further steps of rehabilitation
- Phase 2: CR clinic, usually three to four weeks
- Phase 3: outpatient CR, one year, carried out by the Agakar (Arbeitsgemeinschaft für ambulante kardiologische Rehabilitation)
- Phase 4: long-term CR, carried out by the Austrian Heart Association.7
In 1992, the World Health Organization (WHO) held consultations in Udine (Italy) and Tours (France) on the issue of needs and action priorities in CR and secondary prevention in patients with CHD, stipulating a comprehensive CR programme should include endurance training, educational counselling, risk factor behaviour modification, vocational guidance, relaxation and training in stress management. Patients can be stratified for their level of coronary risk so that CR can be individualised.8
These guidelines are, in general, still valid for the Austrian Heart Association programme, of course permanently readjusted according to cardiological standards.
Cardiac risk factor control and the problem of long-term risk stratification
Controlling cardiac risk factors, reducing recurrent pathological events and improving life quality are evident aims of long-term CR management. Nevertheless, these important constituents of comprehensive CR usually encounter four main problems:
- As there is no regular obligation to join heart support groups, adherence and sustainable rehabilitation benefits depend on individual motivation.
- The huge behavioural impact on cardiovascular processes is no longer doubted. Still there is the question, whether or not long-term CR activities cause cardioprotective changes in lifestyles.
- Sufficiently extensive networks for local long-term CR availability depend on national healthcare policies.
- These programmes are partly not as rigorously assessed, as for example heart surgery. Nevertheless, optimised outcomes require highest medical standards.
Such issues still pose questions about effects and outcomes of long-term CR programmes,9 which refer also to the interventions’ adequacy, such as intensities of physical activity.10
The INTERHEART study,11 which is taken as reference for this study, identified CHD risks by retrospective analyses. Direct longitudinal studies on cardiac risk stratification and long-term CR, however, are rare. Hard data refer, for example, to the comparison between fatal and non-fatal re-infarction within 30 days,12,13 three or six months,14-16 one year,17,18 or phase 1 and 2.19
Risk adjustment models on the basis of long-term studies20 are rare, and for the discussion of long-term CR effectiveness, as important as such famous studies like Framingham.21,22 Combining results from both study types, however, allows us to hypothesise behavioural long-term coronary risks and secondary preventive mechanisms. The lack of longitudinal research on CR is evident, the few cardiologic long-term studies tend to overlook behavioural and environmental factors.23
CHD risk factor profile
Various studies elucidated the aggressiveness of CHD-related behavioural risk factors, highlighting the effectiveness of lifestyle changes in heart patients.24 As well as that,25 in addition to exercise training, a comprehensive secondary prevention programme for cardiac patients requires aggressive reduction of risk factors through nutritional counselling, weight management, and adherence to prescribed drug therapy. Clinical trials during the past two decades have provided conclusive evidence of reduced mortality in patients with CHD via reduction of individual risk factors by pharmacological and nonpharmacological interventions. The proven salutary impact of comprehensive lifestyle modification often has been overlooked and underemphasised as a first-line approach to secondary prevention.
Referring to behavioural and environmental risk factors of cardiovascular diseases the INTERHEART study,11 identifying smoking, lipids, hypertension, diabetes, obesity, diet, physical activity, alcohol consumption, and psychological factors as outstanding foci in preventive and rehabilitative medicine, became a cornerstone for the cardiology of the new millenium.26 Most strikingly, it showed that the PAR (population attributable risk, indicating the proportion of cases that would not occur in a population if the risk factors were eliminated) of 90.4% for all nine risk factors suggests that, statistically, the nine risk factors combined accounted for basically all of the risk of acute MI in this study population – a truly startling and unanticipated result. Consequently, behaviour and psyche lost their marginal position and gained central interest.
Materials and methods
This cross-sectional questionnaire study investigates how cardiac patients perceive the effect of long-term CR programme attendance on health behaviour changes. In order to evaluate the measurable cardioprotective benefits of long-term CR, further investigations are needed.
Changes in lifestyle as feature and aim of long-term CR
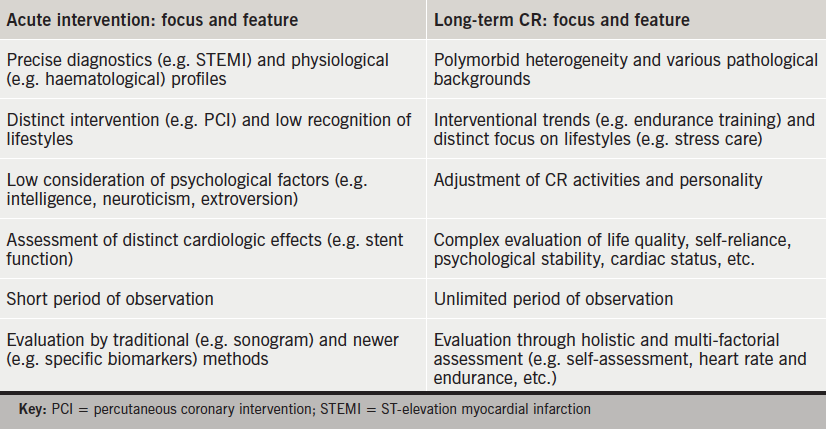
The crucial question of this study is, whether or not the programme offered by the Austrian Heart Association is decisive for lifestyle changes in the perception of the participants? This issue refers also to complementary profiles of acute cardiological interventions and features of long-term CR (table 1).
INTERHEART parameters, questionnaire, and data generation
Those INTERHEART factors that depend directly on an individual’s behaviour were taken as reference for the decisive parameters of our study. The corresponding questionnaire was designed for this study as follows:
- Seven items referring to physical activity, smoking, body mass index (BMI)/obesity, stress, eating habits, sugar/awareness of diabetes risks. As not directly manageable through behavioural changes, lipids and arterial hypertension were not included.
- Previous informal piloting among people attending phase 4 was used to estimate the validity and comprehensibility of the items. Equidistant scales (0, 1, … 10) are assumed to yield interval scale data. Still further research is needed to provide fully validated tools to investigate behavioural changes in cardiac patients.
- Considering the advanced age of participants the questionnaire was easy to understand and to handle. Patients should not get stressed or require individual help for answering.
Questions were formulated as follows:
- Did the ÖHV decisively contribute to changes in my lifestyle for better health?
- Because of my participation in ÖHV activities I have … (following the single behavioural parameters).
- Rank between 0 and 10, “0” meaning “not at all”, “10” meaning “absolutely”.
If participants thought an item not applicable, they could leave it blank.
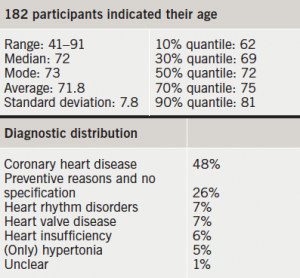
During a two-month period in spring 2014, members participating in various activities of the Austrian Heart Association in the Austrian federate states of Carinthia, Lower Austria, Salzburg, Tyrol and Vienna, were asked to complete the questionnaire. The profile of the participants is shown in table 2.
Results
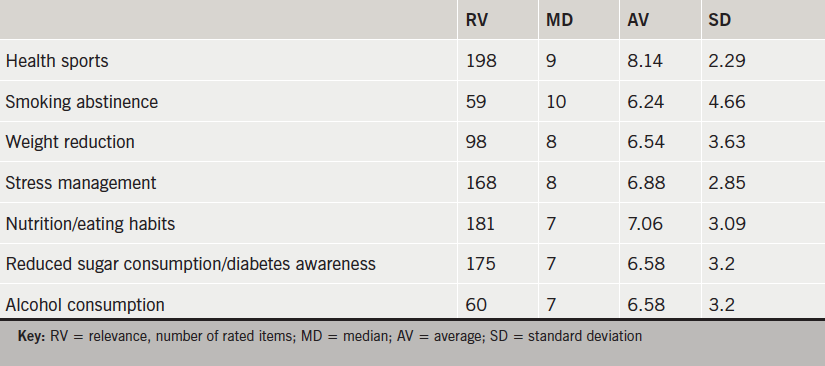
The results are shown in table 3. On the background of the features of the ÖHV phase 4 programme interpretation of these numerical results suggests:
- People attending phase 4 programmes perceive that the programmes have high influence on health sports motivation and sustainability.
- The programmes support stress reduction/competence of stress management and changes in eating habits.
- Participants in this study did not perceive that attendance at phase 4 contributed considerably to changes in smoking behaviour, alcohol and sugar consumption or weight reduction.
- A few unsolicited comments by some participants highlight the importance of experienced social inclusion, regained self-confidence and life-activity, empathetic talks and psychological support.
Discussion
Optimised long-term CR and secondary prevention has to be based on an individually shaped balance between lifestyle, pharmacological treatment, socio-cultural welfare, and the experience of well-being. This requires close collaboration between medical cardiology, long-term CR, and adequate social conditions.
The high influence of long-term CR programmes on patients requires compatibility with the most recent cardiologic guidelines (e.g. sports cardiology, psycho-cardiology) and holistic rehabilitative medicine. The specific quality (e.g. empathic understanding) of heart support groups is of high potential for psychological rebalancing. Research on best practice of collaboration between the CR phases has to be internationally intensified. Long-term CR programmes are not only cost-efficient, but also of high individual and medical economic benefit27.
Acknowledgements
I would like to thank my colleagues RM Dejaco, F Fink, H Kiener, F Radl, D Schiffrer, H Schulter and R Weißsteiner for the standardised and objective generation of empirical data.
Support
No financial support, no funding.
Conflict of interest
None declared.
Key messages
- Long-term cardiac rehabilitation management is important for cardioprotective lifestyle modification
- Physical fitness, stress management, psychological stability and life quality are improved
References
1. Willmer KA, Waite M. Long-term benefits of cardiac rehabilitation: a five-year follow-up of community-based phase 4 programmes. Br J Cardiol 2009;16:73–7. Available from: https://bjcardio.co.uk/2009/03/long-term-benefits-of-cardiac-rehabilitation-a-five-year-follow-up-of-community-based-phase-4-programmes/#
2. Campbell NC, Grimshaw JM, Ritchie LD et al. Outpatient cardiac rehabilitation: are the potential benefits being realised? J R Coll Physicians Lond 1996;30:514–19.
3. Harris DE, Record NB. Cardiac rehabilitation in community settings. J Cardiopulm Rehabil 2003;23:250–9. http://dx.doi.org/10.1097/00008483-200307000-00001
4. Wenger N (ed). Cardiac Rehabilitation: Guide to Procedures for the Twenty-first Century. New York: Taylor & Francis, 2005.
5. Thomas RJ, King M, Lui K et al. AACVPR/ACC/AHA 2007 performance measures on cardiac rehabilitation for referral to and delivery of cardiac rehabilitation/secondary prevention services. Circulation 2007;116:1611–42. http://dx.doi.org/10.1016/j.jacc.2010.06.006
6. Thompson DR, Yu CM. Cardiac rehabilitation: China. In: Perk J, Gohlke H, Hellemans I et al. (eds). Cardiovascular Prevention and Rehabilitation. London: Springer, 2007;pp 48–51.
7. Austrian Heart Association. Website. http://www.herzverband.at/pages/herzlich-willkommen.php
8. WHO Regional Office for Europe. Needs and action priorities in cardiac rehabilitation and secondary prevention in patients with CHD. Document EUR/ICP/CVC 125 4328g. Geneva: WHO Regional Office for Europe, 1993.
9. Jackson AM, Gregory S, McKinstry B. Self-help groups for patients with coronary heart disease as a resource for rehabilitation and secondary prevention – what is the evidence? Heart Lung 2009;38:192–200. http://dx.doi.org/10.1016/j.hrtlng.2009.01.009
10. Angus LH, Gray HG. Phase IV cardiac rehabilitation: a comparison of exercise intensity levels and ratings of perceived exertion between cardiac and non-cardiac participants. Br J Cardiol 2004;11:310–11. Available from: https://bjcardio.co.uk/2004/07/phase-4-cardiac-rehabilitation-a-comparison-of-exercise-intensity-levels-and-ratings-of-perceived-exertion-between-cardiac-and-non-cardiac-participants/
11. Yusuf S, Hawken S, Ounpuu S et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet 2004;364:937–52. http://dx.doi.org/10.1016/S0140-6736(04)17018-9
12. Boersma E, Pieper KS, Steyerberg EW et al. Predictors of outcomes in patients with acute coronary syndromes without persistent ST-segment elevation. Results from an international trial of 9461 patients. The PURSUIT investigators. Circulation 2000;101:2557–67. http://dx.doi.org/10.1161/01.CIR.101.22.2557
13. Kernis SJ, Harjai KJ, Stone GW et al. The incidence, predictors, and outcomes of early reinfarction after primary angioplasty for acute myocardial infarction. J Am Coll Cardiol 2003;42:1173–7. http://dx.doi.org/10.1016/S0735-1097(03)00920-3
14. Eagle KA, Lim MJ, Dabbous OH et al. A validated prediction model for all forms of acute coronary syndrome: estimating the risk of 6-month postdischarge death in an international registry. JAMA 2004;291:2727–33. http://dx.doi.org/10.1001/jama.291.22.2727
15. Fox KA, Dabbous OH, Goldberg RJ et al. Prediction of risk of death and myocardial infarction in the six months after presentation with acute coronary syndrome: prospective multinational observation study (GRACE). BMJ 2006;333:1091–4. http://dx.doi.org/10.1136/bmj.38985.646481.55
16. Luo JG, Yang M, Han L et al. Validity of the GRACE score for 6-month death or reinfarction after presentation with acute myocardial infarction in patients 80 years of age and older. Coron Artery Dis 2013;24:537–41. http://dx.doi.org/10.1097/MCA.0000000000000023
17. Califf RM, Pieper KS, Lee KL et al. Prediction of 1-year survival after thrombolysis for acute myocardial infarction in the global utilization of streptokinase and TPA for occluded coronary arteries trial. Circulation 2000;101:2231–8. http://dx.doi.org/10.1161/01.CIR.101.19.2231
18. Maluenda G, Delhaye C, Gaglia Jr MA et al. A novel percutaneous coronary intervention risk score to predict one-year mortality. Am J Cardiol 2010;106:641–5. http://dx.doi.org/10.1016/j.amjcard.2010.04.011
19. Granger CB, Goldberg RJ, Dabbous O. Predictors of hospital mortality in the global registry of acute coronary events. Arch Intern Med 2003;163:2345–53. http://dx.doi.org/10.1001/archinte.163.19.2345
20. Singh M, Holmes DR, Lennon RJ et al. Development and validation of risk adjustment models for long-term mortality and myocardial infarction following percutaneous coronary interventions. Circ Cardiovasc Interv 2010;3:423–30. http://dx.doi.org/10.1161/CIRCINTERVENTIONS.109.924308
21. Cupples LA, Gagnon DR, Wong ND et al. Preexisting cardiovascular conditions and long-term prognosis after initial myocardial infarction: The Framingham Study. Am Heart J 1993;125:863–72. http://dx.doi.org/10.1016/0002-8703(93)90182-9
22. Kannel WB, Sorlie P, McNamara PM. Prognosis after initial myocardial infarction: the Framingham study. Am J Cardiol 1979;44:53–9. http://dx.doi.org/10.1016/0002-9149(79)90250-9
23. Martin CA, Thompson PL, Armstrong BK et al. Long-term prognosis after recovery from myocardial infarction: a nine year follow-up of the Perth Coronary Register. Circulation 1983;68:961–9. http://dx.doi.org/10.1161/01.CIR.68.5.961
24. Haskell WL. Cardiovascular disease prevention and lifestyle interventions: effectiveness and efficacy. J Cardiovasc Nurs 2003;18:245–55. http://dx.doi.org/10.1097/00005082-200309000-00003
25. Leon AS, Franklin BA, Costa F. Cardiac rehabilitation and secondary prevention of coronary heart disease: an American Heart Association scientific statement from the Council on Clinical Cardiology. Circulation 2005;111:369–76. http://dx.doi.org/10.1161/01.CIR.0000151788.08740.5C
26. Brookes L. INTERHEART: a global case-control study of risk factors for acute myocardial infarction. Medscape Sep 21, 2004. Available from: http://www.medscape.com/viewarticle/489738
27. Mampuya WM. Cardiac rehabilitation past, present and future: an overview. Cardiovasc Diagn Ther 2012;2:38–49. http://dx.doi.org/10.3978/j.issn.2223-3652.2012.01.02

