Introduction
This module will look at the process of haemostasis: the formation and removal of a healthy clot. This will then enable us to understand one of the consequences inappropriate activation of haemostatic mechanisms – arterial and venous thrombosis.
The physiology of haemostasis – how blood clots
The ability of blood to clot, for example in response to injury, is vital – without it, even the smallest cut could lead to fatal haemorrhage. But excessive activation of clotting mechanisms, or clots in the wrong places, can be equally disastrous. A thorough understanding of the physiological mechanisms which lead to blood clotting is essential for going on to understand what happens when things go wrong – and how we can intervene pharmacologically when they do.
Virchow’s triad
Over 150 years ago, the German physician, Rudolf Virchow (figure 1) recognised that a change in any one of three factors could lead to formation of a blood clot (thrombogenesis):
- blood flow
- the vessel wall
- constituents of the blood.
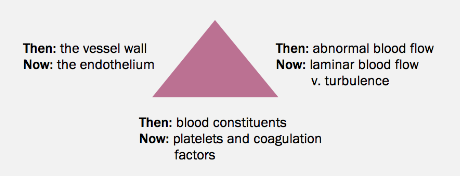
This has been modified by modern understanding (figure 2) of the endothelium and its function, of blood flow characteristics (rheology, including loss of laminar flow and development of turbulence), and a full understanding of blood constituents (coagulation factors and platelets).
In health, clotting is most often the result of changes in the vessel wall due to injury. Changes in blood flow (such as in atrial fibrillation) or blood constituents (such as in inherited thrombophilias) become more important when we consider pathological clotting.
The blood vessel wall
The endothelium is a highly dynamic organ with roles in inflammation (mediating the passage of leukocytes into the tissues), in blood pressure control (by the release of nitric oxide and endothelin), and in haemostasis. In terms of haemostasis, endothelial cells express and release a selection of molecules that promote thrombosis, and others that counter thrombosis (table 1). These factors are in balance; in the healthy state, the balance is in favour of suppression of coagulation, to keep blood flowing freely through the vessel. When endothelial cells are activated – by injury or inflammation – the balance is shifted and procoagulant factors are favoured.
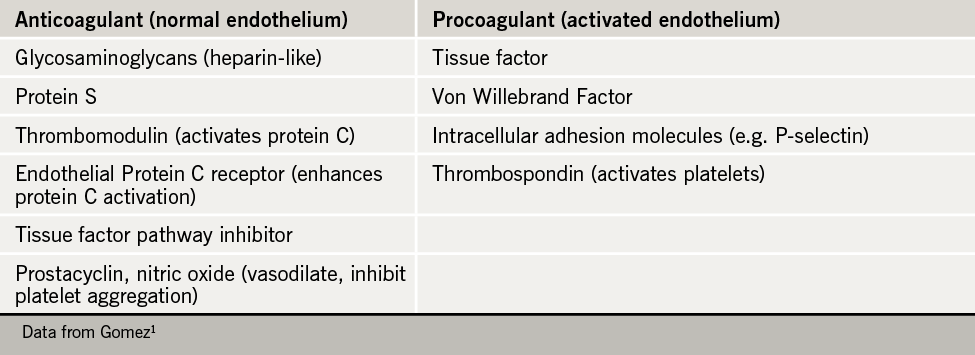
There is evidence that cardiovascular risk factors exert at least some of their pro-thrombotic effect by inducing endothelial activation2.
Blood constituents – platelets and the coagulation cascade
In response to injury, platelets and coagulation factors act simultaneously and synergistically to seal the hole and secure haemostasis.
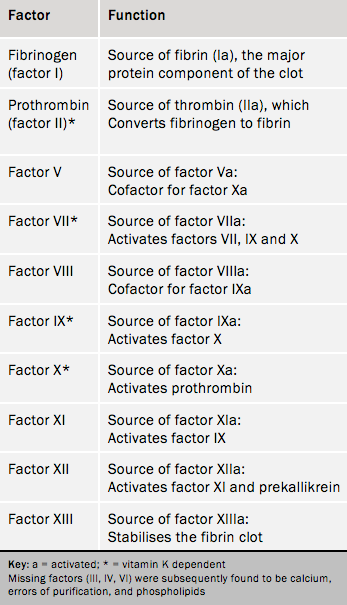
Coagulation factors
Coagulation factors are a collection of mostly liver-produced proteins, some of which rely on vitamin K for their synthesis. Many are zymogens: inactive precursors of an enzyme that, once activated, themselves act on another zymogen. Several factors have names (such as prothrombin); others are denoted by Roman numerals, such as factor V. The ‘resting or inactive’ form is denoted by the simple factor number, but if activated carries the notation ‘a’, an example being factor Va. Table 2 lists the coagulation factors.
