Introduction
Module 1 introduced the physiology and pathology of thrombosis: how platelets and soluble coagulation proteins come together to minimise blood loss in the formation of a clot. Ideally, this process (haemostasis) is highly regulated to ensure that clots develop only under defined circumstances and only in appropriate anatomical locations. However, failure to correctly regulate haemostasis can lead to inappropriate thrombus formation.
According the National Institute for Health and Care Excellence (NICE), each year in the UK almost a quarter of a million people have a first ischaemic stroke or myocardial infarction (MI). In the UK, over 1.4 million people have had a heart attack, and 900,000 are living with the effect of stroke. About 20% of the UK population aged 55–75 years (850,000 people) have lower extremity peripheral artery disease, while 16% of people with cardiovascular disease have multi-vascular disease. We have seen in module 1 that when thrombosis occurs in an artery, it usually does so at a point where the vessel is affected by atherosclerosis, and under conditions of high shear. This means that platelets take a lead role in the initiation of arterial thrombosis, and therefore that inhibition of platelet function is central to the treatment and prevention of arterial thrombotic events. It is worth noting that each of the four major risk factors for cardiovascular disease (smoking, dyslipidaemia, diabetes and hypertension) has been independently associated with increased platelet activity.
The platelet
An understanding of platelet structure and the process of platelet activation is helpful when considering the various ways in which platelets can be suppressed pharmacologically. We have looked at these in some detail in module 1 – a summary, with an emphasis on the main pharmacological targets, is presented below.
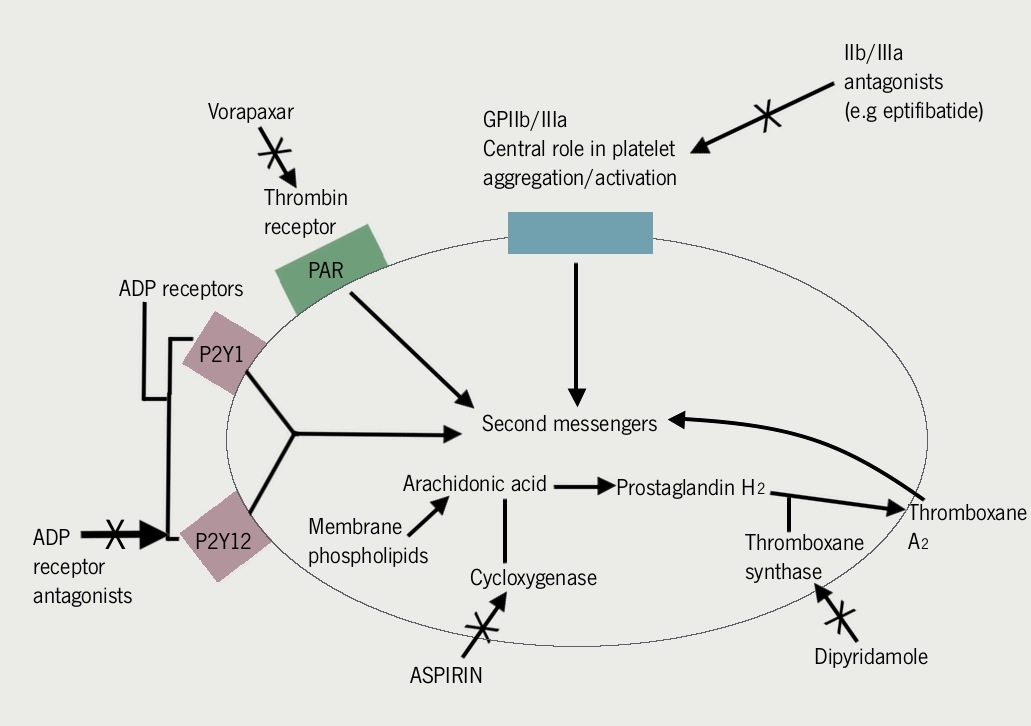
At present, inhibitors of platelet function can be broadly grouped into three according to their mechanism of action:
- Inhibitors of the metabolism of the cell
- Adenosine diphosphate (ADP) receptor blockers.
- Inhibitors of platelet–platelet interactions.
Metabolic inhibitors
There are two major drugs in this class, aspirin and dipyridamole, and both are taken orally. Aspirin is actually three drugs for the price of one, with analgesic, antipyrexial and anti-inflammatory activity, the latter accounting for its effect on the platelet.
Aspirin
Aspirin passively crosses the membrane and irreversibly inhibits cyclooxygenase by acetylation of the amino acids adjacent to the active site. The cyclooxygenase enzyme performs the rate-limiting step in synthesis of thromboxane A2 from arachidonic acid (see figure 1).