Acute coronary syndromes
As discussed in module 1, while platelets are of primary importance in initiating arterial thromboses, both platelets and the clotting cascade are closely linked, so that both are involved in the formation of all clots. Accordingly, although antiplatelet agents are of central importance in the management of acute coronary syndromes (see module 2), anticoagulants are also used in this critical situation to further suppress thrombus formation.
The specialist management of acute coronary syndromes will not be discussed further here: readers are referred to excellent guidelines from the European Society for Cardiology (ESC), and NICE. As discussed above, options are low molecular weight heparin or fondaparinux, with the evidence from OASIS-5 perhaps favouring fondaparinux. UFH or bivalirudin are options for patients undergoing PCI; fondaparinux is not recommended in patients with ST-elevation MI undergoing primary PCI after an excess of procedure-related complications was noted in the OASIS-6 trial.3,12,13
Atrial fibrillation
One of the main risks in AF is cardioembolic stroke. Overall, AF brings a 5% risk of stroke per year but not all patients have the same risk. Risk can be greatly reduced by anticoagulation but as anticoagulation carries a risk of bleeding, it is important to have some means of identifying which patients will, on balance, benefit from anticoagulation – i.e. in which patients does the benefit of anticoagulation outweigh the risks.
Risk assessment
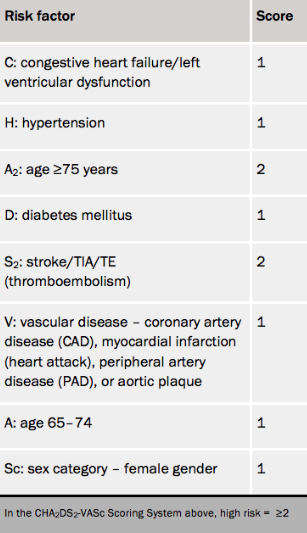
The CHA2DS2-VASc score14 is currently the most widely used tool for estimating stroke risk in AF (see table 3), and is the scoring system recommended by both the ESC and NICE in their recent guidelines.15,16 It represents a refinement of the previous CHADS2 system, particularly in that it defines a group of genuinely low risk patients (score 0 out of 9) who seem to have a very low risk of stroke, and whom the risk of anticoagulation is probably not justified. Annual stroke risk in a large Swedish validation cohort study was 0.2% (score 0) to 12.2% (score 9).17

Both ESC and NICE guidelines advise anticoagulation (in the absence of a contraindication) in patients with a score of 2 or more, and suggest considering it even in patients with a score of 1 (unless the only risk factor is female sex).
An assessment of bleeding risk should also be undertaken before advising on anticoagulation. Probably the most widely used is the HAS-BLED score (see table 4) – this is recommended by both NICE and ESC guidelines, but it is worth remembering that it was designed, and validated, using cohorts of patients taking vitamin K antagonists:
ESC guidelines advise caution with anticoagulation with a score of 3 or more (bleeding risk approximately 3.7 per 100 patient years). However, each case should be considered individually, with a full discussion of risks and benefits, and taking into account each patient’s perspective. Importantly, several of these factors are correctable, and attention should be paid to this to ensure anticoagulation can be offered more safely.
Web-based calculators are available which can be used to calculate both CHA2DS2-VASc and HAS-BLED scores.
Choice of anticoagulation in AF
Aspirin does reduce stroke risk to a small extent in AF (approximately 20%), but is much less effective than warfarin (approximately 70% risk reduction). Moreover, there is a growing body of evidence that the inferior efficacy of aspirin is not compensated for by a lower bleeding risk, especially in elderly patients.19,20 Aspirin is therefore not recommended as stroke prevention in current guidelines, except in patients who refuse anticoagulation.
