Counselling patients initiated on warfarin and NOACs
 Due to their unpredictable pharmacokinetics and narrow therapeutic windows, routine coagulation monitoring using INR is essential for vitamin K antagonist anticoagulants. NOACs demonstrate predictable and stable pharmacokinetics and do not require routine coagulation monitoring.
Due to their unpredictable pharmacokinetics and narrow therapeutic windows, routine coagulation monitoring using INR is essential for vitamin K antagonist anticoagulants. NOACs demonstrate predictable and stable pharmacokinetics and do not require routine coagulation monitoring.
The need for regular monitoring must be explained to the patient. The INR can define how quickly the blood clots in relation to someone who is not on warfarin, i.e. a value of three indicates that it will take three times longer for someone’s blood to clot in comparison to someone not on warfarin. The patient will appreciate that too low an INR (INR <2) will not give the full benefit of preventing strokes, whereas too high an INR (INR >4) can put the patient at risk of bleeding heavily should they cut themselves, or bruising badly if they fall.
 When patients first start taking warfarin, they will attend the anticoagulant clinic frequently, as they adjust their dosage to an appropriate level. Most people find that once they are established on warfarin their INR is fairly stable, and they need only attend the clinic every six to 12 weeks.
When patients first start taking warfarin, they will attend the anticoagulant clinic frequently, as they adjust their dosage to an appropriate level. Most people find that once they are established on warfarin their INR is fairly stable, and they need only attend the clinic every six to 12 weeks.
There are multiple factors that can influence the efficacy of warfarin, including: liver function; age; concomitant medicines; dietary intake of leafy vegetables; and alcohol. As such, the required dose of warfarin needs to be tailored to each individual and may change from time to time, for example when drinking more alcohol, going on holiday, or taking a course of antibiotics.
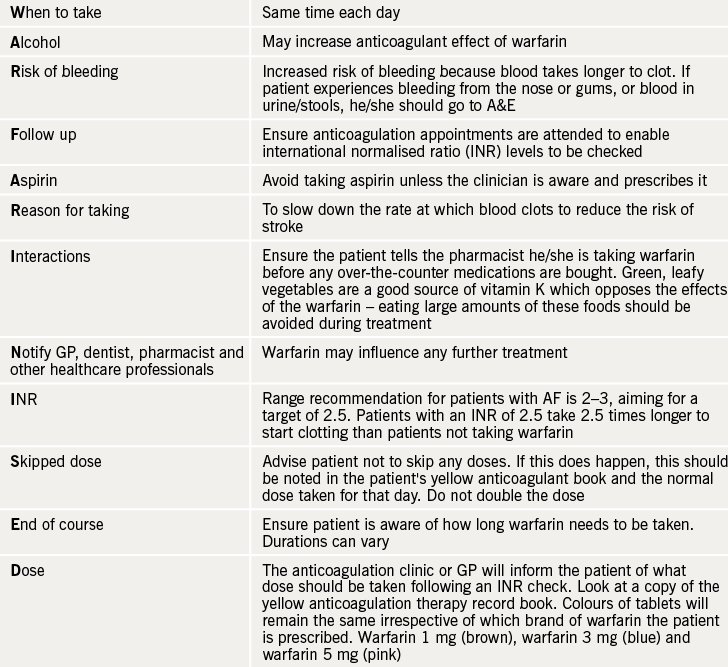
WARFARINISED (see table 1) is a good acronym to remember the important counselling points for patients starting therapy with warfarin.
Considerations for use of NOACs
The NOACs are covered in previous modules (modules 3 and 4). In October 2011 the European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) recommended an update to the product information for dabigatran following reports of increased bleeding and bleeding fatalities in the elderly and those with poor renal function. The recommended updated product information includes advice that renal function should be assessed in all patients before starting treatment (dabigatran is 85% renally metabolised). During treatment, renal function should be assessed at least yearly in patients over 75 years of age and in those with known renal impairment. It should also be assessed whenever a decline in function is suspected.
Rivaroxaban, apixaban, and the newer edoxaban, are renally metabolised to a lesser extent, but caution (e.g. dose reduction) and, as appropriate, close monitoring in patients with moderate-to-severe renal impairment should still be applied.
The newer antiplatelet agents (ticagrelor and prasugrel) are more potent than clopidogrel, but are associated with increased bleeding rates, while the NOACs range from being non-inferior to superior to warfarin, and offer the benefit of less intracranial haemorrhage with variable major bleed rates (ranging from equivalent to less bleeding versus warfarin). Refer to the latest British National Formulary and Summaries of Product Characteristics (SPCs)3,4 for side effects, cautions, contraindications and interactions.
Note that for dabigatran and rivaroxaban, indigestion is a known adverse effect and, as such, patients should be counselled and gastric protection considered as appropriate. All of the newer agents have a shorter half-life than warfarin, such that the drug concentration (and, thus, anticoagulant effect) would decline soon after one or more doses are missed. If the patient misses a dose of rivaroxaban or edoxaban, it is recommended that they take it as soon as possible. However, not more than one tablet in a single day should be taken to make up for a missed dose. For dabigatran, patients should immediately take the missed dose unless the next is due within six hours, in which case it should be discounted. For apixaban, if a dose is missed, the patient should take it immediately and then continue with twice daily intake as before.
Lastly, ensure patients receive their respective anticoagulant alert card and carry it with them at all times, to present to any relevant healthcare professional who is managing their care.
