Introduction
The management of valve disease can be divided into three main steps:
(1) Detection.
(2) Planned management including surveillance.
(3) Appropriate surgery or percutaneous intervention.
There is broad agreement that limitations exist at all levels. This module discusses these and the evidence for methods of improving care.
Detection
The prevalence of moderate or severe heart valve disease using echocardiographic screening of populations is 2.5%.1 This compares with 1.8% using echocardiography only when clinically indicated. Severe aortic stenosis causes approximately one unexpected death at the time of major non-cardiac surgery per Trust per year in the UK.2
Community screening by echocardiography can increase detection rates by a factor of up to 10,3 but this includes mild disease. While detecting mild rheumatic disease leads to important secondary prophylaxis, the gain is less evident for other types of disease since there is no proven means of reducing the rate of progression. There is, however, some evidence for the need to control modifiable risk factors.4 A proportion of patients progress to severe disease in five years5 making it clinically appropriate to recommend surveillance to allow optimal timing of surgery.
Medical management and surveillance
Limitations
The initial management of patients with valve disease is usually conservative.6,7 Meticulous follow-up at an interval appropriate to the level of valve disease is then vital. However accepted management guidelines are not followed adequately. In a Canadian study8 the rate of adherence to American Heart Association (AHA) guidelines varied between only 2% and 30% and adherence is also limited in the USA, Europe9 and the UK.10
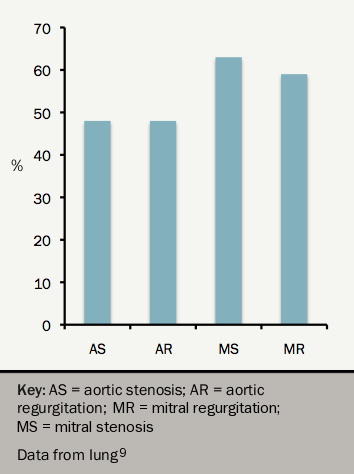
As a result, patients are often referred for surgery too late. In the EuroHeart Survey,9 around one half with valve disease were in NYHA Class III or IV at the time of surgery (see figure 1).
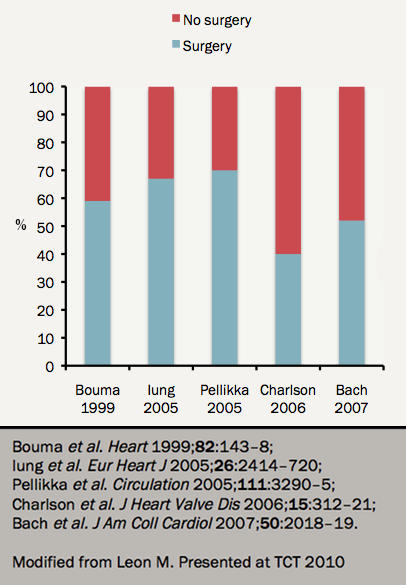
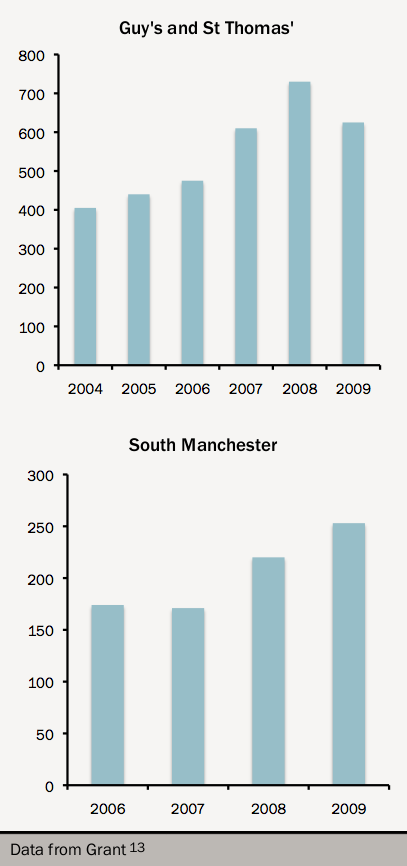
At least one third (range 30–60%) of elderly patients with severe aortic stenosis are not referred for surgery at all even when clinically indicated11,12 (see figure 2). The development of a percutaneous valve programme leads to increased rates of conventional surgery13 suggesting that there were clinically inappropriate perceptual barriers to referral (see figure 3).
Patients with normally-functioning replacement valves should be assessed clinically every year,6,7 but may not require regular echocardiography. In practice, these patients are often discharged to their primary physician.