Value of a specialist valve clinic
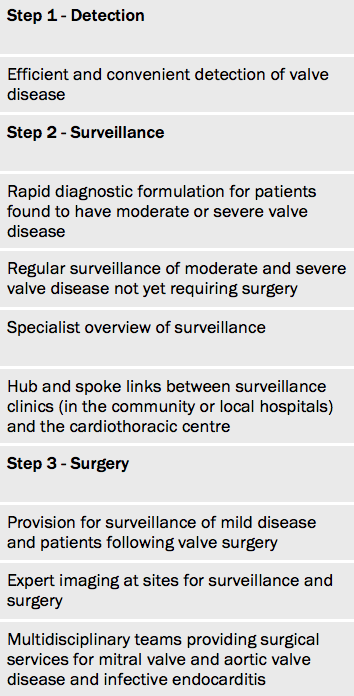
Specialist clinics (see table 1) are seen as best-practice14,16 and allow:
- More accurate diagnostic formulation.
- Better application of national and international guidelines (92%) compared with a general cardiology clinic (41%)10 (see figure 4).
- Earlier detection of symptom-onset. Patients with severe aortic stenosis16 followed in a valve clinic had a delay of 88 days compared with 351 days in a general clinic.
- Appropriate timing of referral to surgery.
- Improved survival. Patients with severe degenerative mitral regurgitation who receive inadequate surveillance17 have a higher mortality than those with moderate regurgitation, but survival is excellent if they are instead managed in a valve clinic.18
- Referral to the correct surgeon.
- Reduction of medical outpatient appointments with devolved sonographer or nurse-led surveillance clinics. This frees the cardiologist to spend more time with patients in whom clinical decisions are required.
Surgery
Limited access
Access to surgery remains variable and limited worldwide. In India valve operations are performed at a rate of 1.8 per 100,000 population compared with 28 per 100,000 in the Netherlands.19 In Brazil only 11,000 operations are performed each year, and 80% of those needing surgery remain on a waiting list.20
There is also variability of access to surgery in industrially developed countries.11 The causes of this variance have not been explored but may partly reflect the activity of community physicians.
Mitral valve repair
Early repair in asymptomatic patients with degenerative disease is increasingly recommended.6 However patients suitable for repair frequently undergo valve replacement instead. This is a serious problem. The operative mortality for mitral valve replacement for asymptomatic patients in the UK is 6.2% compared with 0.6% for mitral valve repair, albeit in unmatched patients.21
The EuroHeart Survey9 found that 50% of patients with mitral regurgitation underwent replacement rather than repair. Similarly the mean repair rate in the US between 2005 and 2007 was 41% (range 0 to 100%).22 In the UK, rates of repair for degenerative mitral valve disease vary in different centres from 0 to 98%21 and 25% of asymptomatic patients undergo mitral valve replacement instead of repair.
Hospital volume

A retrospective review23 addressed the effect of hospital volume for 13,614 patients having elective surgery in the USA. The volume of mitral valve procedures per institution varied widely from an average 22 cases in the lowest quartile to 394 cases per year in the highest quartile. Unadjusted mortality rates were 3% in the lowest-volume quartile and only 1% in the highest-volume quartile.
However only a small proportion of the variability in mortality was statistically accounted for by volume while a greater proportion was accounted for by whether the patient had a repair rather than replacement. The rates of mitral valve repair increased from 48% in the lowest-volume quartile to 77% in the highest-volume quartile (P<0.0001). There was also a gradient in the use of biological replacement valves occurring in approximately 59% of replacements in the low-volume compared with 75% in the high-volume quartile (P<0.0002).
