Investigation and diagnosis
The diagnosis generally requires evidence of bloodstream infection and involvement of the heart and can be aided by the Duke clinical criteria8,9 (see table 1 and figure 2). Endocarditis is definite with two major or with one major and three minor or with five minor criteria. Possible endocarditis is defined by one major and one minor or no major and three minor criteria.
Table 1. Definitions of the terms used in the European Society of Cardiology 2015 modified criteria for the diagnosis of infective endocarditis
This table can be viewed as table 14 in Habib9
Figure 3. European Society of Cardiology 2015 algorithm for diagnosis of infective endocarditis
This table can be viewed as figure 3 in Habib9
Unless the patient is severely ill, three blood culture sets should be taken at different times before starting treatment with antimicrobials. Ask whether antimicrobials have been given by the GP before admission because the most common cause of culture negative endocarditis is prior treatment. Look for other sources of sepsis by culturing sputum and urine and requesting a chest X-ray, as clinically indicated.
A full blood count may show a high white cell count and a low haemoglobin usually with the normochromic normocytic pattern of chronic disease. A C reactive protein level is a useful marker of disease activity. The creatinine level should be measured and eGFR calculated since renal dysfunction may complicate IE (as a result of glomerulonephritis, renal emboli, aminoglycoside toxicity or low cardiac output).
Streptococcus bovis group infections are associated with gastrointestinal pathology in up to one half of cases, including benign polyps, inflammatory bowel disease and malignancy. Bowel investigation will be necessary but should not hold up cardiac surgery if indicated.
Management
IE is uncommon and best looked after by a specialist team.10,12 This is a prominent change in the new ESC guidance.9 At a cardiac centre this consists of a cardiologist specialising in valve disease, infection specialist and/or microbiologist, cardiac surgeon, and echocardiographer. This may be difficult at a small hospital in which case there should be close links with the cardiac centre. This approach has been shown to improve one year mortality from 18.5% to 8.2%.13,14
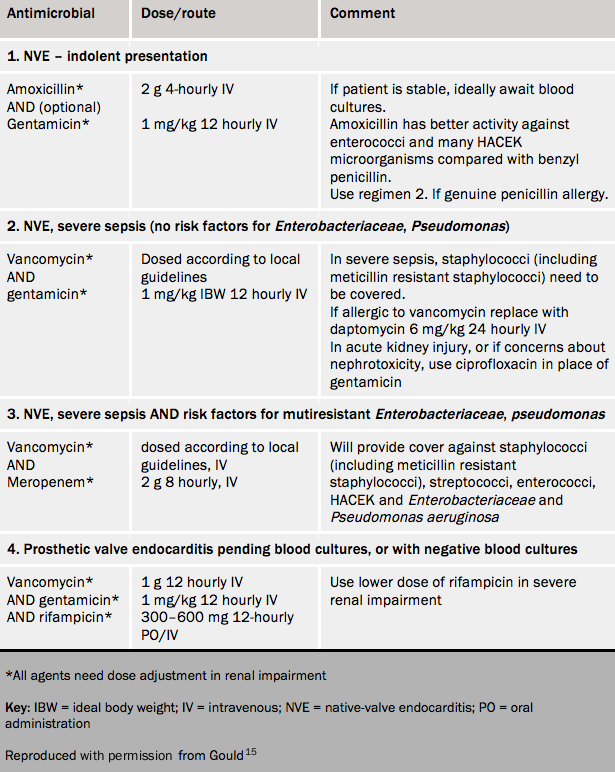
Initial treatment is with antimicrobials. Whenever possible wait for blood culture results; antimicrobial regimens should ideally target the causative organism. If the patient is critically ill and requires emergency surgery, then one dose should still be given beforehand. A scheme for initial empirical antimicrobial therapy is given in table 2.
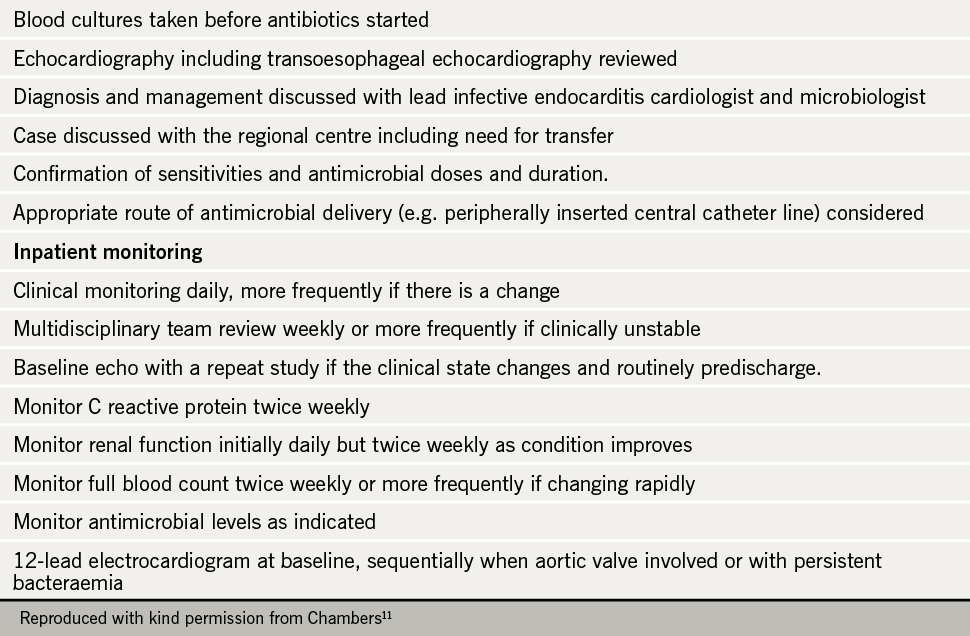
Monitoring of the patient is summarised in table 3.11
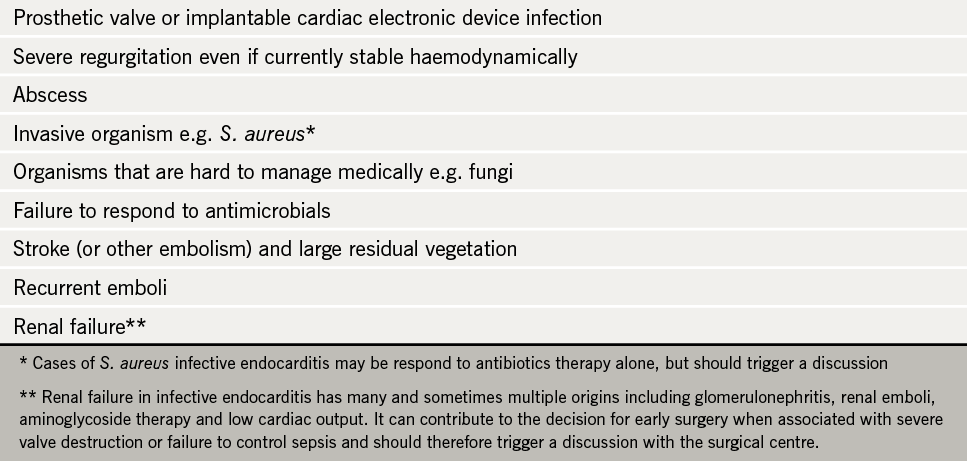
Every case should be discussed with the endocarditis team at the local cardiothoracic centre. All cases of complicated endocarditis should be transferred early (see table 4).