Outpatient parenteral antimicrobial therapy (OPAT) can be considered after the first two weeks of inpatient therapy if:
- The patient is stable and responding well to therapy; without signs of heart failure; without any indications for surgery; and without uncontrolled extra-cardiac foci of infection
- No renal impairment
- The patient is willing and home circumstances are suitable
- Daily visits from a nurse are feasible and physician review once or twice each week.
IE caused by any microorganism may be appropriate for OPAT. However, S. aureus is associated with high mortality and complications, and caution is therefore advised where this is the cause.
Patients who have valve replacement surgery for IE and are in hospital solely to complete a planned treatment course may be suitable for OPAT.
Criteria for surgery
Approximately 50% of IE patients require surgery in addition to antimicrobial therapy. Mortality can be reduced by early diagnosis and treatment, and early surgery once indicated.7,16,18
The accepted Class I criteria9 are:
- Failure to control sepsis. This includes organisms known to be unlikely to respond to antimicrobial therapy e.g. fungus.
- Severe valve destruction.
- Recurrent emboli despite appropriate antimicrobial therapy.
Some points:
- If there are large (>10 mm) and mobile vegetations in the presence of severe valve disease, early surgery should be considered (Class IIa).
- Native valve endocarditis with isolated very large vegetations (>30 mm) is now a Class IIa indication for surgery.9
- A cerebral event should not be a contraindication to early surgery if indicated.
- Deterioration despite appropriate antimicrobial therapy is an indication for surgery not further antimicrobials.
Outpatient follow-up
The acute episode does not end with discharge from hospital. There is a 10% risk of surgery within the first year after discharge and the relapse or recurrence rate is approximately 6%.9,17 There should be outpatient follow-up, usually at one, three, six and 12 months after discharge.9,10 This should occur within a specialist valve clinic.
Transthoracic and transoesophageal echocardiography
Echocardiography is key to the diagnosis of endocarditis and is indicated if there is a moderate or high clinical likelihood of endocarditis. It is not indicated as a fever screen because:
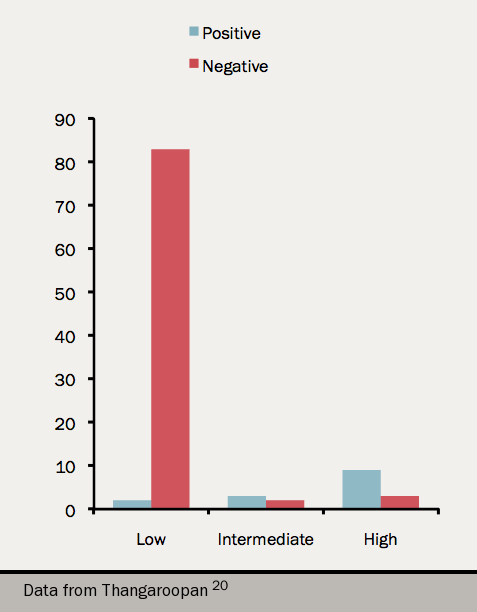
- The yield is very low19 (see figure 2)
- The positive predictive value declines because of the increased probability of incidental abnormalities or normal variants (Lambl’s excrescence, transverse sinus, calcific degeneration, myxomatous thickening) being detected and cause false positive scans
It may be difficult to phrase the report judiciously. Some example phrases covering the spectrum of suspicion are ‘an echogenic mass’:
- ‘typical of a vegetation’
- ‘consistent with a vegetation’
- ‘consistent but not diagnostic of a vegetation’
- ‘consistent with a vegetation but more in keeping with calcific degeneration (or another pathology)’
- ‘most consistent with calcific degeneration (or another pathology)’
Echocardiography may not be indicated routinely for hospital-acquired S aureus infection if sepsis settles quickly after removal of the responsible intravascular lines.
