
The Ross Procedure (see figure 1110) consists of substituting the patient’s own pulmonary valve for the diseased aortic valve. Usually a homograft is then implanted in the pulmonary position. The rationale for such a complex procedure is that a living valve with good durability is placed in the important aortic side while the replacement valve is placed in the low pressure right side. The procedure has a relatively high early complication rate but good long-term results. There is evidence that the autograft grows which is particularly important for avoiding repeated surgery in children. It may also be relatively resistant to infection.
Who has which valve?
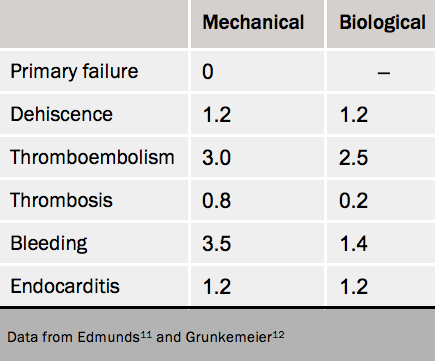
There is no ideal replacement valve and all can have complications. Table 211,12 shows objective performance criteria (OPC) for complication rates.
Biological valves have the advantage of
– not needing treatment with warfarin,
but the disadvantage of:
– primary failure
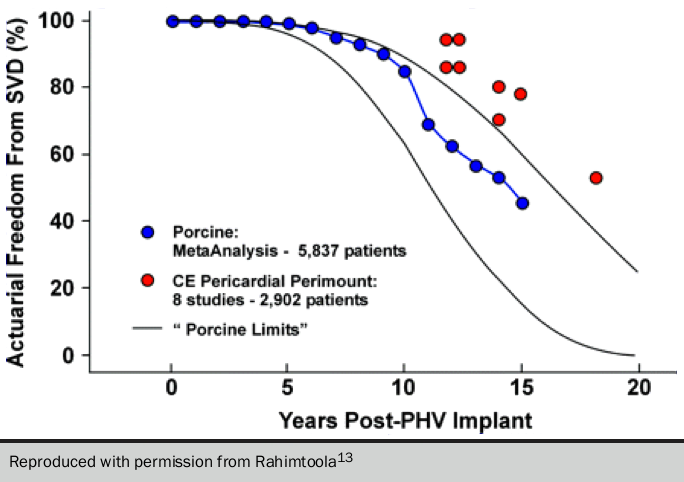
beginning after about seven years in the aortic position and five years in the mitral position.9 A diagram of failure rates is shown in figure 12.13
By contrast mechanical valves effectively have no primary failure, but patients need anticoagulation to prevent thrombosis and thrombembolism which makes the patient prone to bleeding. In general, a biological valve is used in the aortic position for patients aged >65 years and a mechanical valve for age <60 years.13 In between 60 and 65 years, the choice depends on individual patient factors including their own preference. Exceptions are the younger person unwilling or unable to take anticoagulants in whom a Ross procedure or homograft are alternatives. Decisions concerning type of valve must be shared with the patient.14
In patients not suitable for mitral valve repair, a mechanical valve is usually implanted below the age of 65 years, and a biological valve above the age of 70 years. Individual factors must again be applied in the range 65 to 70 years. Improvements in life expectancy mean that many patients with biological valves are beginning to live long enough to require consideration of re-do surgery and these may be suitable for a TAVI.
Some specific situations are outside these general rules. Some surgeons preferentially use a biological valve in a woman considering childbirth in order to avoid the need for warfarin. However, this necessitates further surgery after a short duration, long enough to complete the family.
We recommend the following short review:
How a prosthesis in aortic valve replacement is chosen
Chan KM John, Nawaz M Asghar, Punjabi Prakash P
e-journal of the ESC Council for Cardiology Practice. Vol9 N°35 28 Jun 2011
The following review also addresses choice of valve in women of childbearing age:
Sliwa K, Johnson MR, Zilla P, Roos-Hesselink JW. Management of valvular disease in pregnancy: a global perspective. Europ Heart J 2015;36:1078–89. http://dx.doi.org/10.1093/eurheartj/ehv050
