Refractory angina (RA) describes those patients with persistence of symptoms despite optimal conventional strategies. It is often associated with a maladaptive psychological response, resulting in significant burden on hospital services. This observational study sought to assess the short- and long-term impact of psychotherapy on quality of life, mood and symptoms.
Between 2011 and 2012, consecutive attendees to a specialised RA service were recruited. Intervention consisted of a course of cognitive-behavioural therapy allied with an education programme. Outcome measures were collated pre-intervention, one month and two years post-intervention. Validated questionnaires were utilised for scoring assessments: SF-36 (Short-Form 36) for quality of life, HADS (Hospital Anxiety and Depression Scale) for anxiety/depression, and SAQ (Seattle Angina Questionnaire) for functional assessment.
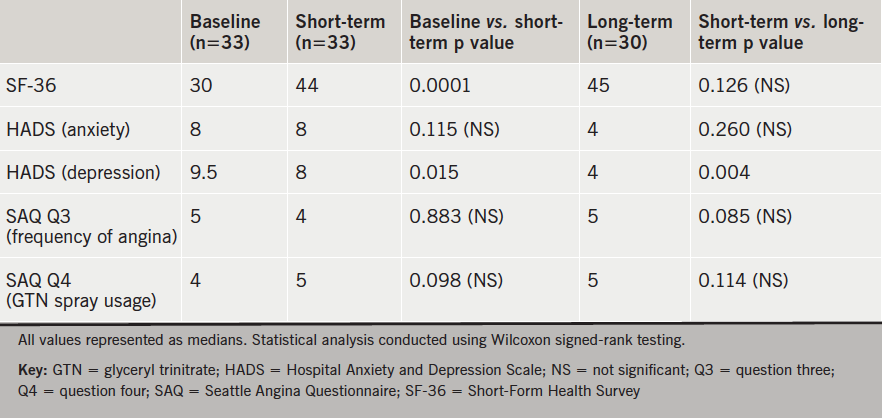
There were 33 patients included. Median SF-36 scores increased and this effect remained in the long term. Levels of depression reduced, and improved further at subsequent review. Frequency of angina was comparable, both short and long term. Usage of glyceryl trinitrate (GTN) spray was similar at one-month follow-up and at two years.
In conclusion, a short course of psychotherapy appears to improve quality of life and mood in patients with RA, and is achieved independent of symptom control. Further research is warranted so that the debilitating morbidity associated with this disorder can be abrogated.
Introduction
Angina results from myocardial ischaemia as a consequence of mismatch between supply and demand.1 Most cases are secondary to atherosclerotic disease of coronary arteries.2 Conventional therapy to manage such patients has relied on pharmacotherapy and revascularisation strategies. Pharmacological options routinely include aspirin, statin, rate-limiting therapy, such as beta blocker or calcium-channel antagonist, and vasodilators, such as isosorbide mononitrate and nicorandil. Revascularisation may be through percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG).3
Chronic, refractory angina constitutes a particular subset of patients that have persistence of symptoms, despite targeting of modifiable risk factors, optimal pharmacotherapy as tolerated and revascularisation when anatomically feasible.4 The condition affects in excess of 5% of patients with angina, and results in significant public health burden.5 The most contemporary data on prognosis in these cohorts estimate a mortality rate of approximately 30% after nine years.6 Symptoms are typified by chronic, disabling chest pain secondary to myocardial ischaemia. This is commonly aligned with a maladaptive psychological response to their disorder. As a consequence, there is greater utilisation of medical services including frequent hospital admissions with recurrent and sustained pain.7 This results in predictable compromise on health-related quality of life, co-existent with a high incidence of anxiety and depression.8 Its economic burden has been found to be comparable with other prevalent conditions such as chronic, non-cancerous pain.9
Management options for such patients are rather limited. Focus of care has traditionally centred on dose optimisation of established pharmacotherapy and use of adjunct therapy such as ranolazine and/or ivabradine.10 Further therapeutic strategies offered in specialised centres include enhanced external counter-pulsation (EECP), coronary sinus reducer, transcutaneous electrical nerve stimulation (TENS) and stellate ganglion block.11 However, a structured pathway of care to address the maladaptive psychological responses in these cohorts appears to be lacking and is often neglected.
Bradford Royal Infirmary provides a focused service to manage patients with refractory angina (BRAS). A component of this involves a short psychological intervention composed of a course of pragmatic rehabilitation based on a combination of cognitive-behavioural therapy (CBT) and an education programme.12 It is delivered over four weekly sessions, with each lasting two hours. These are delivered by a Clinical Nurse Specialist and Clinical Psychologist working in partnership. This study aimed to investigate its short-term and long-term impact on quality of life, mood and symptoms.
Method
Recruitment of patients for the initial study was obtained from consecutive attendees to BRAS between September 2011 and November 2012. Verbal, informed consent was obtained in all cases. Outcome measures of interest included quality of life, levels of anxiety/depression, angina frequency and use of glyceryl trinitrate (GTN) spray. Well-established and validated survey questionnaires were used for quantitative scoring assessments.
The Short-Form Health Survey (SF-36) provides a measure of health status and quality of life.13 It consists of eight scale scores, each carrying equal weight. Areas covered include vitality, physical functioning, bodily pain, general health perceptions, physical, emotional and social role functioning, and mental health. A score of 0 constitutes maximum disability, with 100 equivalent to no disability. The Hospital Anxiety and Depression Scale (HADS) was utilised to assess for levels of anxiety and depression.14 It incorporates a seven-item scale for each, with scoring from 0–3. Therefore, a person can score between 0 and 21 for both, and a cut-off of 8/21 is generally utilised for diagnostic purposes.15 The Seattle Angina Questionnaire (SAQ) is utilised commonly as a functional status measure of coronary artery disease.16 Two specific questions were adapted to assess for frequency of angina (Question 3) and usage of GTN spray (Question 4). Questionnaires were completed immediately pre- and one-month post-intervention via phone consultation with a co-author, who had no direct involvement with delivery of the CBT programme. In November 2014, after a two-year duration, the same questionnaires were utilised on the cohort by a different co-author to assess long-term effects on the outcome measures. Collation and analysis of data were performed in an identical fashion to the earlier study.
Data analysis was conducted by a different co-author to enhance internal validity. Information was collated using Microsoft Excel 2012. Statistical analyses were performed using Minitab 16. Non-parametric data were compared using Wilcoxon signed-rank testing and presented as medians. Statistical significance was defined by p<0.05.
Results
There were 33 patients recruited for the initial study: 76% (25/33) were male with 24% (8/33) female. Median age was 63 years (inter-quartile range of 9 years).
Results are summarised in table 1. During short-term follow-up, median SF-36 scores for quality of life increased (30 vs. 44; p=0.0001). Levels of anxiety (8 vs. 8; p=0.115) were similar but depression (9.5 vs. 8; p=0.015) decreased. Question 3 of the SAQ was adapted to explore frequency of angina symptoms (“over the past four weeks, on average, how many times per day have you had chest pain, chest tightness, or angina?”). Values showed no statistically significant difference (5 vs. 4; p=0.883). Question 4 of the SAQ was adapted to assess frequency of GTN spray usage (“over the past four weeks, on average, how many times per day have you had to take GTN [nitroglycerin tablets or spray] for your chest pain, chest tightness or angina?”). No change was noted pre- and post-intervention (4 vs. 5; p=0.098).
questionnaires in patients with chronic, refractory angina
Over the course of a two-year duration, three patients in the cohort underwent revascularisation and were, therefore, excluded from follow-up evaluation. Therefore, 30 patients were eligible (83% male [25/30] and 17% female [5/30]). Responses from questionnaires were directly compared with those obtained from short-term follow-up. SF-36 scores for quality of life appeared similar (45 vs. 44; p=0.126). Levels of anxiety (4 vs. 8; p=0.26) and depression (4 vs. 8; p=0.004) were improved. There appeared to be no statistically significant difference in frequency of angina (5 vs. 4; p=0.085) or usage of GTN spray (5 vs. 5; p=0.114).
Discussion
Refractory angina is a chronic disease with significant associated morbidity. Traditional management strategies have relied upon pharmacological therapy to try and alleviate ischaemic symptoms. However, the condition has strong associations with a maladaptive psychological response predominantly driven by fear, with frequent utilisation of hospital services. A structured approach that targets the psychological burden of this disorder is commonly not available across the UK.
Bradford Royal Infirmary offers a specialised service (BRAS) to address these deficiencies. The four foundation sessions are run sequentially on a weekly basis. The focus of these sessions are to help patients develop more effective coping strategies, primarily based on a greater understanding of what angina is, and by dealing with the many misconceptions that patients have developed. Furthermore, patients engage with the concept that management is not solely limited to pharmacotherapy and revascularisation, but also involves a fundamental alteration in thought processes involved with symptom recognition and interpretation. Particular emphasis is placed on lifestyle alterations including pacing, setting of realistic goals, relaxation exercises, energy conservation and sleep quality enhancement. A rigorous underpinning in social, cognitive and behavioural theories is critical to achieve success. Sessions are run in small groups, providing an informal forum to share and engage with experiences of others to achieve a collective goal of more effective self-management of this chronic condition.
Previous studies assessing the benefits of psychotherapy have been largely positive. A meta-analysis by McGillion et al. pooled the results of seven randomised-controlled trials of self-management programmes for chronic angina, including refractory angina.17 Results from 949 participants suggested that intervention resulted in approximately three fewer episodes of angina per week, accompanied by a reduction in usage of GTN spray. Of note, there was heterogeneity in methodology and sampling, which limited external validity. In a cohort of 271 patients, Moore et al. demonstrated a statistically significant reduction in frequency of hospital admissions (2.40 to 1.78 per annum) and duration of admission (15.4 to 10.3 days), with an effect that was immediate and sustained.18
Results from our study largely corroborate these findings. Short-term follow-up data suggest that psychotherapy is effective in improving patients’ quality of life and mood with comparable levels of anxiety and reduced severity of depression. Interestingly, however, this appears to be achieved independent of improvement in angina frequency or GTN spray usage. Long-term follow-up after a two-year duration demonstrates that improvement in quality of life and mood is sustained, and again, this is not correlated with alterations in symptoms. One may hypothesise from this that education and psychotherapy has beneficial effects in altering a patient’s perception of their chronic disease, with subsequent positive impact on quality of life and mood.
Limitations
Our study does have intrinsic limitations. The relatively small sample size in our study limits extrapolation of findings, and may account for the non-statistically significant differences with some comparisons. Information on background medical therapy, left ventricular function and ischaemic burden was not consistently available and, therefore, could not be included in our analysis, albeit of clear relevance in enhancing external generalisability. Additionally, we were unable to access data relating to adjunct non-pharmacological therapy during the period of study (TENS or EECP, for example), which could clearly act as a potential confounder. The rationale behind correlating responses to survey questionnaires via telephone was to ensure that answers were not processed, with the hope that this would reflect their true perceptions at that given time. However, one could legitimately argue that patients may have experienced indirect coercion through such means, and this would result in manipulation of attained responses.
Conclusion
In conclusion, this study provides an impression that education and psychotherapy, in the context of patients with chronic, refractory angina, may be of use in alleviating perception of symptoms, with resultant impact on quality of life and mood. Despite its intrinsic limitations, results provide an impetus to explore this area of management further using larger-scale, multi-centre trials. This would be of pertinence in enabling a focused, systematic strategy to manage patients with refractory angina and improve the chronic, debilitating morbidity that is associated with the disorder.
Contributions
PAP, PAS and MK were involved with initial study design. ST and ST conducted the CBT sessions. MK collated data for short-term follow-up. YC collected the data for long-term follow-up. PAP wrote the manuscript as primary author and performed statistical analysis. PAS supervised the study and revised the article. All authors have approved the final version prior to formal submission.
Conflict of interest
None declared.
Funding
There are no external or internal sources of funding to declare.
Editors’ note
See also the editorial by Wright and De Silva on pages 45–6 of this issue. Also of interest, Tinson et al. on pages 61–4 of this issue.
Key messages
- Refractory angina is often associated with a maladaptive psychological response to symptoms, resulting in a significant burden on hospital services
- A short course of psychotherapy appears to improve quality of life, levels of anxiety and depression and this benefit is preserved long-term. Frequency of symptoms appears unchanged
- Further research in this field appears to be warranted so that the significant morbidity associated with this chronic disorder can be negated
References
1. Mukherjee D, Bhatt D, Roe MT. Direct myocardial revascularization and angiogenesis. How many patients might be eligible? Am J Cardiol 1999;84:598–600. http://dx.doi.org/10.1016/S0002-9149(99)00387-2
2. Farb A, Tang AL, Burke AP et al. Sudden coronary death. Frequency of active coronary lesions, inactive coronary lesions, and myocardial infarction. Circulation 1995;92:1701–09. http://dx.doi.org/10.1161/01.CIR.92.7.1701
3. Mehta SR, Yusuf S, Peters RJ et al. Effects of pretreatment with clopidogrel and aspirin followed by long-term therapy in patients undergoing percutaneous coronary intervention: the PCI-CURE study. Lancet 2001;358:527–33. http://dx.doi.org/10.1016/S0140-6736(01)05701-4
4. Kim M, Kini A, Sharma SK. Refractory angina pectoris: mechanism and therapeutic options. J Am Coll Cardiol 2002;39:923–34. http://dx.doi.org/10.1016/S0735-1097(02)01716-3
5. Banai S, Ben Muvhar S, Parikh KH et al. Coronary sinus reducer stent for the treatment of chronic refractory angina pectoris. J Am Coll Cardiol 2007;49:1783–9. http://dx.doi.org/10.1016/j.jacc.2007.01.061
6. Henry TD, Satran D, Hodges S et al. Long-term survival in patients with refractory angina. Eur Heart J 2013;34:2683–8. http://dx.doi.org/10.1093/eurheartj/eht165
7. Moore RKG, Groves DG, Bridson JD et al. A brief cognitive-behavioural intervention reduces hospital admissions in refractory angina patients. J Pain Symptom Manage 2007;33:310–16. http://dx.doi.org/10.1016/j.jpainsymman.2006.10.009
8. Furze G, Lewin R, Murberg T et al. Does it matter what patients think? The relationship between changes in patients’ beliefs about angina and their psychological and functional status. J Psychosom Res 2005;59:323–9. http://dx.doi.org/10.1016/j.jpsychores.2005.06.071
9. McGillion M, Croxford R, Watt-Watson J et al. Cost of illness for chronic stable angina patients enrolled in a self-management education trial. Can J Cardiol 2008;24:759–64. http://dx.doi.org/10.1016/S0828-282X(08)70680-9
10. Kim M, Kini A, Sharma SK. Refractory angina pectoris: mechanism and therapeutic options. J Am Coll Cardiol 2002;39:923–34. http://dx.doi.org/10.1016/S0735-1097(02)01716-3
11. Mannheimer C, Carlsson CA, Emanuelson H. The effects of transcutaneous electrical stimulation in patients with severe angina pectoris. Circulation 1985;71:308–16.
12. Wright C, Towlerton G, Fox K. Optimal treatment for complex coronary artery disease and refractory angina. Br J Cardiol 2006;13:306–08.
13. RAND Health. 36-Item Short Form Survey from the RAND Medical Outcomes Study. Available from: https://www.rand.org/health/surveys_tools/mos/mos_core_36item.html [accessed on 6 May 2015].
14. Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand 1983;67:361–70. http://dx.doi.org/10.1111/j.1600-0447.1983.tb09716.x
15. Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J Psychosom Res 2002;52:69–77. http://dx.doi.org/10.1016/S0022-3999(01)00296-3
16. Spertus JA, Winder JA, Dewhurst TA et al. Development and evaluation of the Seattle Angina Questionnaire: a new functional status measure for coronary artery disease. J Am Coll Cardiol 1995;25:333–41. http://dx.doi.org/10.1016/0735-1097(94)00397-9
17. McGillion M, Arthur H, Victor JC et al. Effectiveness of psychoeducational interventions for improving symptoms, health-related quality of life, and psychological well being in patients with stable angina. Curr Cardiol Rev 2008;4:1–11. http://dx.doi.org/10.2174/157340308783565393
18. Moore RK, Groves DG, Bridson JD et al. A brief cognitive-behavioral intervention reduces hospital admissions in refractory angina patients. Pain Symptom Manage 2007;33:310–16. http://dx.doi.org/10.1016/j.jpainsymman.2006.10.009
