The chest X-ray

The chest X-ray may be abnormal (see figure 3) at the time of diagnosis in 80–90% of patients with idiopathic PAH (IPAH).
The findings may include central pulmonary arterial dilatation and sometimes decreased peripheral blood vessels. These signs may be missed on “routine” chest X-ray when they are borderline. Enlargement of the right atrium and right ventricle may also be seen.
The chest radiograph may show lung disease such as chronic obstructive pulmonary disease (COPD) or other interstitial lung disease; or indicate left heart disease such as valvular abnormalities. In both these cases, the chest X-ray helps to provide a more accurate diagnosis of the cause of PH. In chronic thromboembolic pulmonary hypertension (CTEPH), the Westermark sign may be observed (dilatation of pulmonary vessels proximal to the embolus with collapse of the distal vessels).
The degree of pulmonary hypertension does not correlate with the extent of abnormalities on the chest X-ray. A normal chest X-ray does not exclude significant pulmonary hypertension.
Learning point
- Most patients with idiopathic pulmonary arterial hypertension have abnormalities on chest radiography at diagnosis
Pulmonary function tests
Normal lung function does not preclude pulmonary hypertension.1 Lung function tests should include forced expiratory volume in one second (FEV1), forced vital capacity (FVC), total lung capacity (TLC), functional reserve capacity (FRC), residual volume (RV), transfer factor of the lung for carbon monoxide (TLCO), diffusion capacity of the lung for carbon monoxide (DLCO), and rate of carbon monoxide transfer (KCO). Patients with PAH usually have decreased DLCO and mildly restricted lung volumes. Lung function tests should be interpreted in conjunction with CT findings.
Learning point:
- Normal lung function does not preclude pulmonary hypertension
Echocardiography
Echocardiography is used to determine the likelihood of PH being present and its underlying cardiac causes. Echocardiography cannot definitively make a diagnosis of PH: this is achieved at cardiac catheterisation. The patient requires a full diagnostic study and the sonographer should search for all available evidence of PH (see figure 4). It is a useful non-invasive investigation when PH is suspected.

With the kind permission of Dr Luke Howard, Hammersmith Hospital, London
Identification of findings suggestive of PH
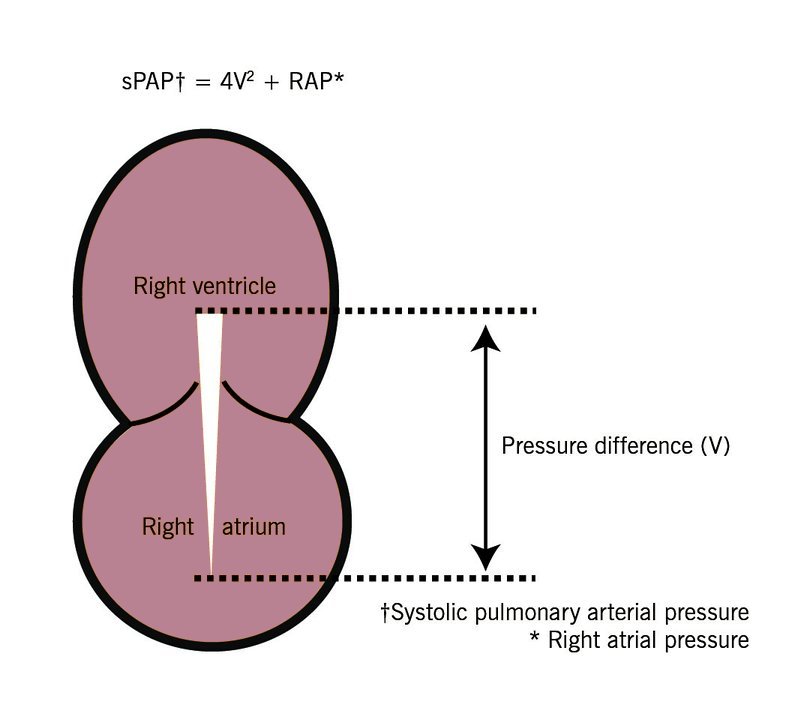
Doppler ultrasound is used to estimate systolic pulmonary arterial pressure (sPAP) based on the peak velocity of the tricuspid regurgitation jet (TRV) and the right atrial pressure. This relationship is described in the modified Bernouilli equation in the absence of pulmonary valve stenosis (see figure 5):
Estimated sPAP = 4V2 + RAP
where V = peak velocity of tricuspid regurgitation measured by continuous wave Doppler ultrasound; RAP = right arterial pressure