Confirmation of conditions that constitute a differential diagnosis of PH
Echocardiography can provide confirmation of conditions – pulmonary valve stenosis and pericardial constriction – that constitute a differential diagnosis of PH.
Echocardiography is used to estimate the severity of right ventricular dysfunction. (We have seen earlier that this is used to estimate PAP, based on the peak velocity of the TRV jet, which enables sPAP to be calculated, taking into account estimated RAP). The final diagnosis of pulmonary hypertension, however, can only be made by cardiac catheterisation since pressure can only be estimated from echocardiography. The right ventricle is more compliant than the left: with increased pressure loading, the interventricular septum may flatten or bulge into the left ventricular cavity. Right ventricular remodeling and hypertrophy occur, and lead to deterioration in systolic and diastolic function, which determine exercise capacity, symptoms and prognosis. Dilatation of the right ventricle also leads to tricuspid annular dilatation and tricuspid regurgitation. In turn, the cardiac output can become progressively impaired.
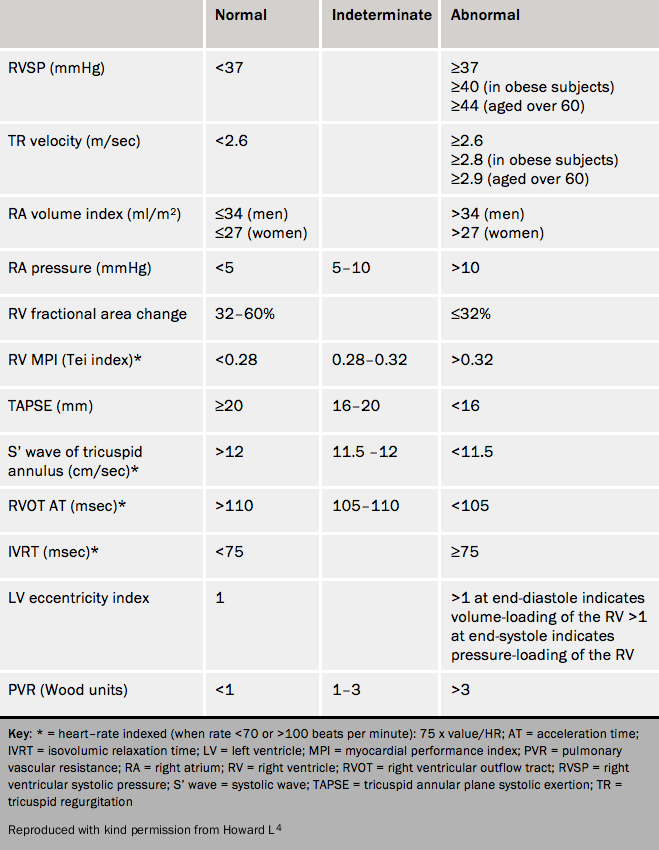
Table 3 shows normal values for the right ventricle and pulmonary circulation.
Measures of function such as the “Tei index” or myocardial performance index, an index of right ventricular systolic and diastolic function (isovolumic contraction and relaxation times divided by ejection time), predicts an adverse outcome.5 Echocardiography can use the combination of two-dimensional and Doppler imaging to measure stroke volume, cardiac output and pulmonary vascular resistance. Echocardiographic findings have been shown to correlate with prognosis and mortality (see below).
Exercise echocardiography has not found a role in routine clinical practice. It is technically challenging to undertake and to interpret.
Learning point:
- Echocardiography is an important non-invasive method of choice in seeking a diagnosis of pulmonary hypertension, but is not definitive
Haematology and biochemistry
Blood tests should be undertaken to determine potential causes of breathlessness, heart failure and PH. All PH patients should have routine haematology, biochemistry and thyroid function tests. These may include:
- full blood count
- renal function
- liver function
- thyroid function
- autoimmune screen, including antinuclear antibodies, anti-centromere antibodies, double-stranded DNA, U1-RNP
- C-reactive protein
- protein electrophoresis
- anti-cardiolipin antibodies
- hepatitis serology in PAH
- HIV in PAH
- haemoglobin electrophoresis (in chronic haemolytic anaemia)
- thrombophilia screen (including anti-phospholipid antibodies and lupus anticoagulant, protein S, protein C, factor VIII)
- NT pro-BNP and troponin I
Some serum biomarkers correlate with survival in idiopathic PAH, and may be of use during serial follow-up. Brain natriuretic peptide (BNP) and N-terminal (NT)-proBNP are independent predictors of survival; proBNP appears to correlate with right ventricular enlargement and dysfunction.6,7 Other biomarkers, when raised, that are indicative of a poor prognosis include uric acid and cardiac troponins.
In patients who present with acute deterioration, investigations should include blood tests (full blood count, urea and electrolytes, liver function tests, thyroid function, C-reactive protein and troponin), mid-stream urine culture, blood cultures and arterial blood gases.
Liver function tests are often abnormal due to hepatic congestion. Renal function may be compromised by pre-renal failure. An autoimmune screen should be performed to search for CTDs. It is not uncommon to find mildly raised anti-nuclear antibodies in idiopathic PAH.
Learning point
- Serology can help to determine the cause of pulmonary hypertension; and biomarkers its prognosis
