Further investigations for pulmonary hypertension
Further investigations confirm the diagnosis of PH, its functional and haemodynamic severity, and determine its cause. These investigations include exercise testing, arterial blood gas measurement, and various types of heart and lung imaging. Arriving at the final diagnosis will require the integration of results from multiple imaging investigations. It is recommended that this process is carried out at a multidisciplinary meeting between physicians and radiologists with experience in the various forms of imaging. This is standard practice at PH centres.
Exercise testing
The rationale for exercise testing is that in PH exercise induces symptoms. The six-minute walk test (6MWT) and bicycle ergometry cardiopulmonary exercise testing (CPET) objectively evaluate the exercise capacity in patients with PH. The 6MWT is a measure of submaximal exercise capacity and in severe PH the patient is limited by cardiac output; CPET measures maximal exercise capacity. The distance covered in a 6MWT has been used as a primary end point in randomised clinical trials to evaluate the effects of treatment in PAH.
The six-minute walk test
The main elements in how to carry out a 6MWT are shown in table 4. The distance walked is related to stride length and hence patient height. It is also related to age, psychological factors and other concurrent diseases such as those affecting the musculoskeletal system.
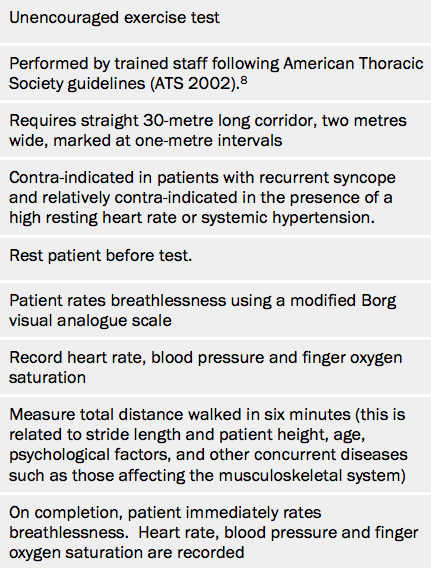
It is not clear how 6MWT distances can be corrected for these individual patient-related factors and so its results should be interpreted according to patient circumstances. While a young and otherwise normal person should walk well in excess of 500 metres, an elderly person who is otherwise frail may walk considerably less. Despite this limitation, the baseline 6MWT distance is of prognostic value.
The 6MWT is one of the most commonly used investigations in PH and is repeated routinely at each follow-up visit.9 Patients whose blood pressure falls on exercise have a worse prognosis than those who increase their systemic blood pressure. Careful note needs to be taken of blood pressure response to exercise in advising patients about exercise prescription in everyday life.
Cardiopulmonary exercise testing (CPET)
CPET assesses the function of the cardiopulmonary, circulatory and skeletal muscle unit. It requires highly trained staff to ensure reproducible results. Gas exchange and ventilation are recorded continuously during this test. Findings in PAH, which become more marked as the disease worsens, include reduction of oxygen uptake at the anaerobic threshold and at peak exercise, peak work rate, peak heart rate and ventilator efficiency. In idiopathic PAH, peak oxygen uptake and peak systolic arterial pressure during exercise predict prognosis.10,11 This test is increasingly used by PH centres since it helps to define the extent of exercise limitation and the mechanism of limitation. It may be helpful in serial follow-up.
Learning point:
- Baseline six-minute walk test distance has been shown to correlate with survival in pulmonary hypertension
Arterial blood gases
Arterial blood gases are measured in room air. Typically, in PAH, arterial oxygen tension is normal or reduced and arterial carbon dioxide tension is also decreased. By contrast, arterial carbon dioxide tends to be normal or raised in lung disease.
Heart and lung imaging
There are a number of possible investigations that can be carried out with imaging, although results must be interpreted in an integrated fashion, together with the results of other investigations.
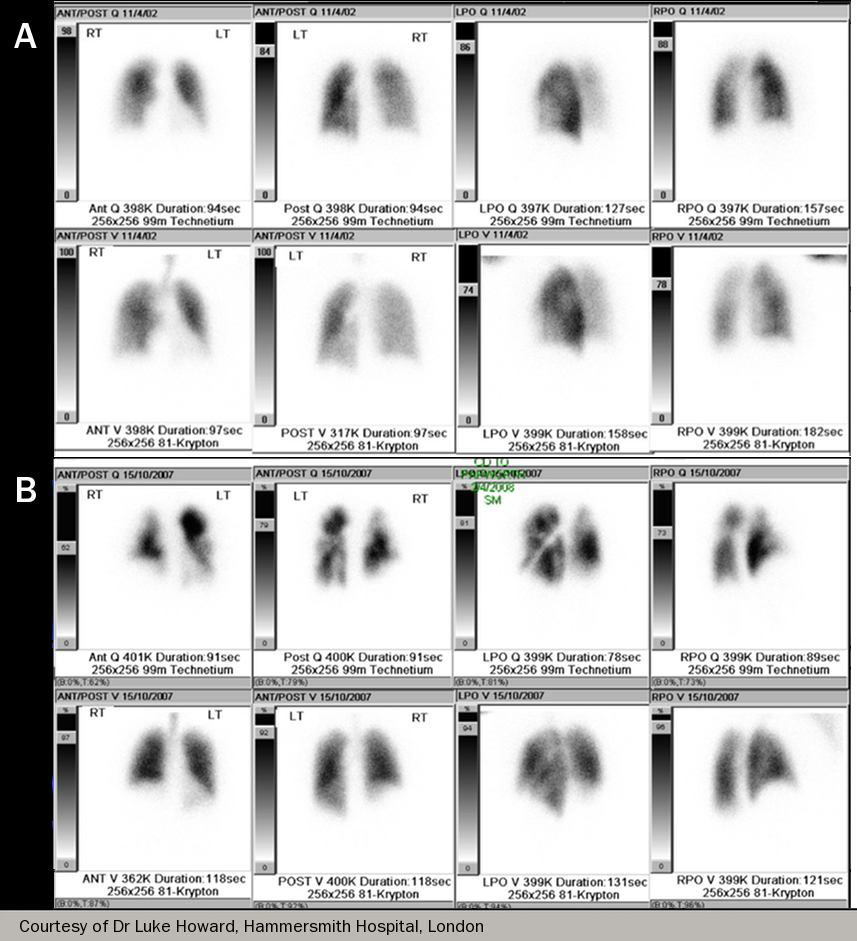
The ventilation perfusion scan
It is very important to exclude chronic thromboembolic disease in patients presenting with PH. About a half of patients with CTEPH do not have a history of stepwise deterioration associated with acute pulmonary embolism.
The ventilation/perfusion scan has a higher sensitivity than computerised tomography (CT) for detecting CTEPH: a normal ventilation/perfusion scan effectively excludes CTEPH, with a sensitivity of 90–100% and a specificity of 94–100%12 (see figure 7).
CT scanning is limited by its inability to image small vessels and hence distal thrombus. This is quite different from acute PE, where CT scanning is the imaging of choice for diagnosis.
Learning point:
- The ventilation/perfusion scan is the best investigation to detect CTEPH in unexplained pulmonary hypertension