Thoracic CT scanning
Features of pulmonary arterial hypertension that may be seen at CT13 are central pulmonary artery dilatation, abrupt narrowing or tapering of peripheral pulmonary vessels, right ventricular hypertrophy, right ventricular and atrial enlargement, dilated bronchial arteries, and a mosaic pattern of attenuation due to variable lung perfusion (see figure 8). Pulmonary venous hypertension may result from pulmonary veno-occlusive disease, pulmonary venous compression by extrinsic lesions (e.g., mediastinal fibrosis), left-sided cardiac disease, or pulmonary vein stenosis. Its histologic hallmarks include venous intimal cellular proliferation, medial hypertrophy, and thickening of the internal elastic lamina; capillary congestion and proliferation; interlobular septal thickening; lymphatic dilatation; and, sometimes, venous infarction and vascular changes characteristic of pulmonary arterial hypertension. CT scans in patients with pulmonary venous hypertension show pulmonary interstitial and alveolar edema with signs of pulmonary arterial hypertension. High-resolution CT with standard axial and angiographic acquisitions is useful for identifying underlying disorders and differentiating among the various causes of secondary pulmonary hypertension.13
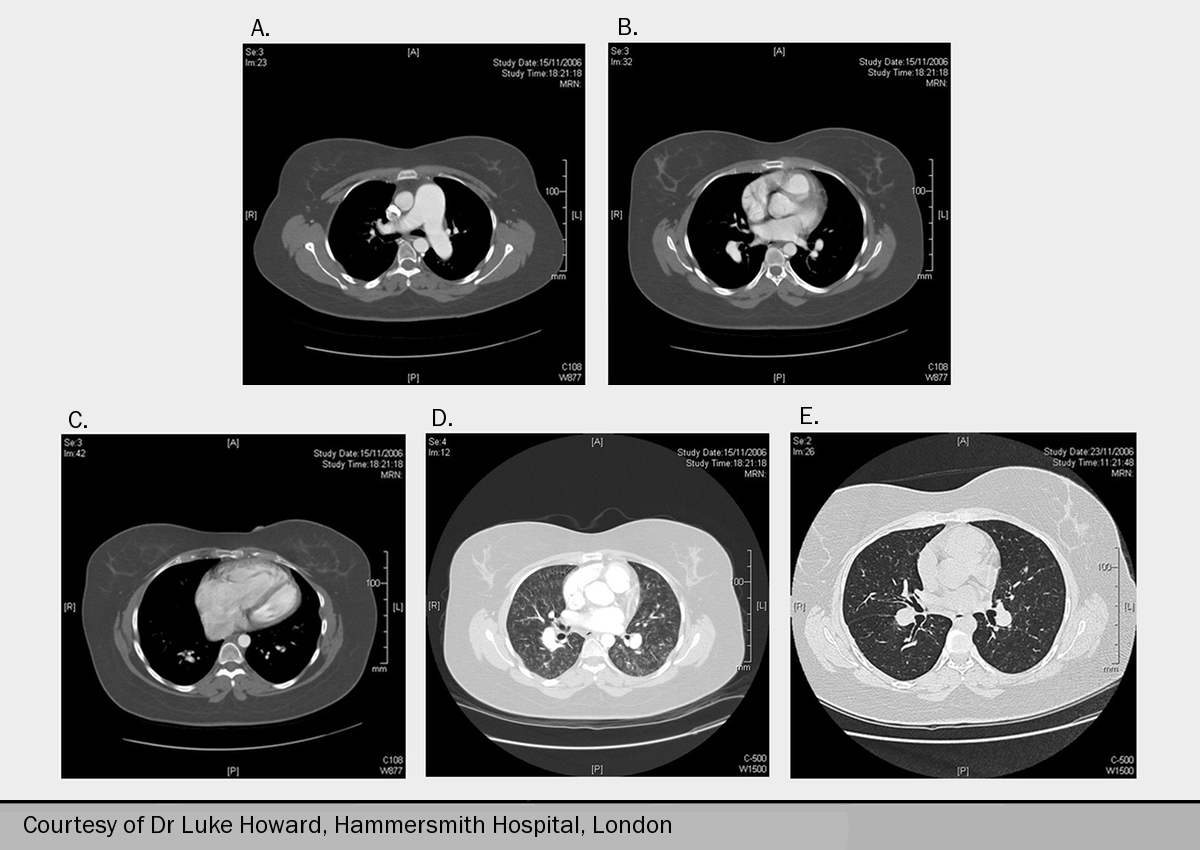
While ventilation perfusion scanning is most sensitive for the detection of thromboembolic disease, CT angiography is one investigation used to determine the presence of surgically accessible CTEPH. This is detected by sudden changes in vessel diameter caused by bands and webs, filling defects and pulmonary artery occlusions. Hypertrophy of the bronchial circulation may also be observed, and this is usually most marked in CTEPH. Lung windows in CTEPH often show a mosaic attenuation pattern of underperfused and normally perfused lung. While this pattern is suggestive of CTEPH, it is not diagnostic.
Lung windows provide detailed information about the lung parenchyma, allowing the diagnosis of disease of the lung and interstitium. The presence of lung disease needs to be interpreted in the light of lung function tests.

Lung windows may also show features of pulmonary oedema. Pulmonary veno-occlusive disease (figure 9) or pulmonary capillary haemangiomatosis should be suspected in the absence of left heart disease, and in particular of raised left atrial pressure. They share the common CT features of interlobular septal thickening, ground glass opacification, mediastinal lymphadenopathy and pleural effusions.14 Although these diagnoses are rare, they are important because treatment with disease-targeted therapy for PAH may be hazardous. In addition, undertaking a vasoreactivity study at the time of cardiac catheterisation might also result in clinically important pulmonary oedema.
Most cases of PH are associated with enlargement of the pulmonary arteries. The main pulmonary artery is normally less than the diameter of the adjacent aorta. Fluid in the superior pericardial recess is also a sensitive sign of pulmonary hypertension.
Selective pulmonary angiography
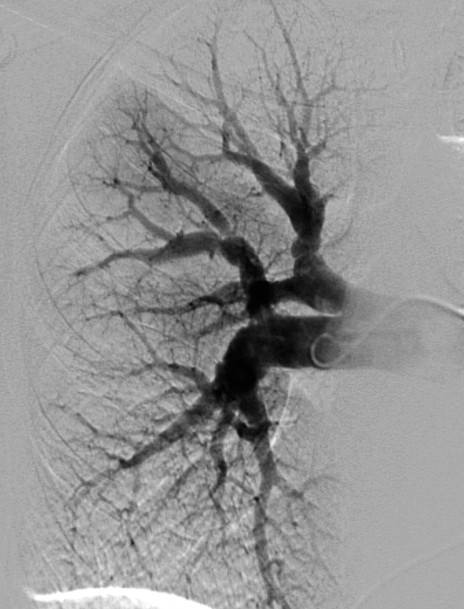
This investigation should be carried out in selected patients only. It is indicated for the assessment of operability of patients with CTEPH (figure 10), and also when results from CT pulmonary angiography and ventilation perfusion scanning are discordant about the diagnosis of CTEPH. In this situation, selective pulmonary angiography is the gold standard investigation. It must be carried out by an experienced operator who can obtain high-quality diagnostic images. It should not be performed in the cardiac catheterisation laboratory using a coronary set since the field size is too small to obtain satisfactory diagnostic images.
Cardiac magnetic resonance imaging
Cardiac magnetic resonance imaging is indicated in selected patients in the following situations:
- In patients with CTEPH, magnetic resonance pulmonary angiography may be used in surgical planning. Although it is not yet considered the gold standard above selective pulmonary angiography, some surgeons are prepared to accept one or other of these investigations.
- To help in the evaluation of certain congenital heart defects, which have been demonstrated at echocardiography
- Further evaluation of other echocardiographic findings such as cardiomyopathies or previous myocardial infarction
- Evaluation of right and left ventricular function, including stroke volume, cardiac output, ejection fraction and ventricular mass. These measurements can be achieved accurately
It can evaluate the size and function of the right ventricle and can assess blood flow, stroke volume, cardiac output and distensibility of the pulmonary artery. Since there is low inter-observer variability, it may be a good follow-up tool, although this is yet to be demonstrated prospectively. Right ventricular function is an indicator of prognosis in pulmonary arterial hypertension.
A decreased stroke volume, increased right ventricular end-diastolic volume and decreased left ventricular end-diastolic volume are associated with a poor prognosis.15 The role of cardiac MRI in the serial follow-up of patients with PH remains to be validated.

An example of contrast-enhanced MR angiography is shown in figure 11.
Learning point:
- Cardiac MRI reliably assesses right ventricular function
Abdominal ultrasound
Abdominal ultrasound is used to assess portal hypertension and liver disease, although it cannot definitively exclude portal hypertension. Where there is doubt, portal vein pressure can be assessed at cardiac catheterisation.
Lung biopsy
Lung biopsy carries a high mortality risk in pulmonary hypertension, and is contra-indicated. Lung biopsy which is undertaken for breathlessness of uncertain cause in the absence of pulmonary hypertension may rarely show pulmonary veno-occlusive disease (PVOD) and pulmonary capillary haemangiomatosis (PCH). In the presence of pulmonary hypertension, lung biopsy should not be undertaken even when these diagnoses are suspected.
According to the ESC 2009 guidelines,2 lung biopsy in patients is discouraged as a routine procedure not only because it entails a substantial risk of morbidity and mortality but also because the results carry a low risk of altering either the diagnosis or the treatment strategy.
Learning point:
- Lung biopsy carries substantial risk in PH patients, and is contra-indicated
