Improvements in cardiorespiratory fitness (CRF) are associated with better health outcomes. The Chester step test (CST) is used to assess the changes in CRF following a protocol-driven cardiovascular prevention and rehabilitation programme (CPRP) entitled MyAction. CRF expressed as predicted VO2max, can be influenced by physiological adaptations and/or retest familiarity-efficiency. Therefore, we employed an index ratio between oxygen uptake and heart rate (O2 pulse) to determine if the improvement in CRF is related to a true physiological adaptation.
In total, 169 patients, mean age 66.8 ± 7.3 years attended a 12-week MyAction CPRP. All were assessed using the CST on the initial and end-of-programme assessment. O2 pulse was estimated from the CST and was calculated by dividing VO2 into the exercise heart rate multiplied by 100.
Following the CPRP, VO2max increased by 2.8 ml/kg/min. These changes were associated with an overall increase in O2 pulse by 0.6 ml/beat (p≤0.001) and a 4.1 beats/min (p≤0.001) reduction in the exercise heart rate response on the CST.
In conclusion, O2 pulse provides transparency on the physiological adaptations following a CPRP and can be used to help patients recognise the benefits of exercise training. For example, the average patient increased his/her O2 pulse by 0.6 ml/beats and saved 4–7 heart-beats on the CST.
Introduction
In the UK, it is recommended that patients participating in the exercise component of a cardiovascular prevention and rehabilitation programme (CPRP) should undergo a baseline assessment of their cardiorespiratory fitness (CRF).1,2 The rationale behind this assessment is to measure programme outcomes, risk stratification and provide information for physical activity advice. In the UK, many CPRP use the Chester step test (CST), incremental shuttle walk test (ISWT), or the six-minute walk test (6MWT) to assess the changes in CRF following an exercise intervention.2 The choice of exercise test is usually dependent on the patient’s physical activity habits, comorbidities and the availability of equipment and space.2 These tests are normally carried out using standardised protocols with predetermined end points, such as 70% of age predicted heart rate reserve max, symptom-limited and or a score of 14 on the Borg 6–20 ratings of perceived exertion (RPE) scale.2
There are several advantages to using these simple functional capacity tests as they require minimal equipment and represent activities of daily living. As a main outcome measure, these tests typically report improvements in CRF as a change in distance (ISWT, 6MWT), workload (CST) and/or predicted VO2max (CST, ISWT). In order to achieve an accurate change in performance, previous studies have recommended using a practice test to eliminate the learning effect.3,4 The learning effect can count towards a 8–28% improvement in walking performance on the 6MWT and ISWT, respectively.5,6 However, in the clinical setting it is not always practical or cost-effective to perform a practice test. To overcome this limitation, Buckley et al.6 have recommended using the heart rate walking speed index during the ISWT and 6MWT in order to tease out the true physiological adaptations that are associated with regular exercise training. In spite of this, there is a paucity of data that provide an index, which measures the physiology adaptations in patients performing the CST. Therefore, we employed a simple index ratio between oxygen uptake (VO2) and heart rate (O2 pulse) to determine if the improvement in exercise performance following a CPRP is related to a true physiological adaptation.
Materials and methods
This was a retrospective service evaluation study, designed to establish a change in predicted VO2max, submaximal O2 pulse and heart rate (HR) following the Westminster MyAction programme. The Westminster MyAction programme is an innovative nurse-led multi-disciplinary community-based CPRP, which provides integrated care to those with established cardiovascular disease (coronary heart disease, peripheral arterial disease, transient ischaemic attack), as well as those identified to be at high multi-factorial risk (QRisk2 >15%7) through the NHS Health Checks programme. The programme was founded on the principles of the successful EUROACTION (Nurse-Coordinated Multidisciplinary, Family-based Cardiovascular Disease Prevention Programme) cluster randomised-controlled trial.8
The Westminster MyAction programme receives referrals from general practitioner (GP) practices, cardiology clinics and on discharge from cardiology wards. Patients referred to the Westminster MyAction programme attend an initial assessment (IA) and end-of-programme (EOP) assessment following a 12-week exercise and educational programme. During the assessments, the patients were assessed by a cardiac specialist nurse, dietitian and an exercise specialist (figure 1). Following the assessment, a consultant cardiologist led on the prescribing and up-titration of the patient’s medication. Data were collected on patients between September 2009 and March 2014. The present study’s exclusion criteria can be seen in box 1.

Submaximal exercise test

Patients were assessed at IA and EOP using the CST, which consists of five, two-minute stages with a total test duration lasting 10 minutes. All patients were familiarised with stepping up and down on the CST and it was conducted using a standardised protocol9 on a step height of 15, 20 or 25 cm. HR, O2 pulse using predicted oxygen uptake and RPE were recorded after each minute and the CST was stopped if either the HR exceeded 70% of HR reserve max, or the patient reported an RPE of >14 or reported symptoms of chest pain or dizziness. O2 pulse provides an index for stroke volume/cardiac efficacy,10 and was calculated by dividing VO2 uptake (ml/kg/min) by HR. In order to make the mathematical manipulations of the study easier, all results related to the O2 pulse were multiplied by 100 and expressed in ml/beat. This calculation is consistent with previous studies.11
Prediction of VO2max
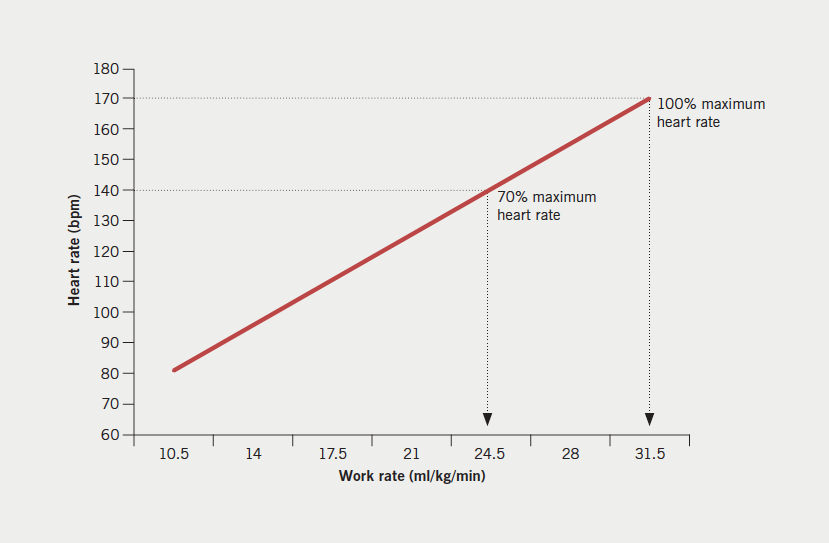
The prediction of VO2max was based on the linear relationship between HR and VO2 consumption and the ‘line of best fit’, was drawn through the submaximal HR responses recorded on each stage of the CST, up to a level which equals the participant’s age estimated HR max (220 – age). At this point, a vertical line was dropped down to the x-axis of the graph, which represents the estimated VO2max.9 The VO2 was expressed in ml/kg/min and an example is presented in figure 2.
Training protocol
The patients attended a community or hospital-based supervised exercise training session once per week for up to 12 weeks and they were encouraged to take part in a home exercise programme or exercise DVD two to three times per week. The supervised exercise training programme consisted of a 15-minute warm-up, 24 minutes of circuit interval training – comprised of aerobic and low-intensity resistance exercises, and a 10-minute cool-down. During the training programme, the patients exercised at an intensity range of between 40 and 70% of their age predicted HR reserve max and/or an RPE of 11–14, as recommended by the Association of Chartered Physiotherapists in Cardiac Rehabilitation (ACPICR).2 Over the 12 weeks, the exercise programme was progressed on the basis of increasing the duration of time spent on the aerobic exercise stations and decreasing the time spent on the resistance exercise stations until 24 minutes of continuous aerobic exercise was achieved.
Statistical analysis

clinical history (n=169)
All data were assessed for parametric assumptions prior to statistical analysis using Stata version 13.0. Data are expressed as mean ± standard deviation (SD). Paired t-tests are conducted on each variable and no correction has been made for multiple hypothesis testing, as this was a retrospective service evaluation study design. A subgroup analysis was carried out on each variable (predicted VO2max, submaximal O2 pulse and HR) on a 15 cm and 20 cm step height. However, it should be noted that due to small numbers, data were not analysed separately on patients achieving stage 5 on the CST or in those taking part on a 25 cm step height.
Results
The final analysis included 169 patients, 59% were Caucasian, 110 were men and 59 were women with mean age 66.8 ± 7.3 years. Out of the 169 patients, 127 patients were stratified as high multi-factorial risk (mean risk score 26.2% ± 8), 20 patients had type 2 diabetes and 28 patients had established cardiovascular disease. The patients attended 12.3 ± 2.9 exercise sessions and 94 (56%), 68 (40%) and seven patients (4%) took part in the CST on a 15, 20 and 25 cm step height, respectively. Demographic variables can be seen in table 1.
Changes in CST performance
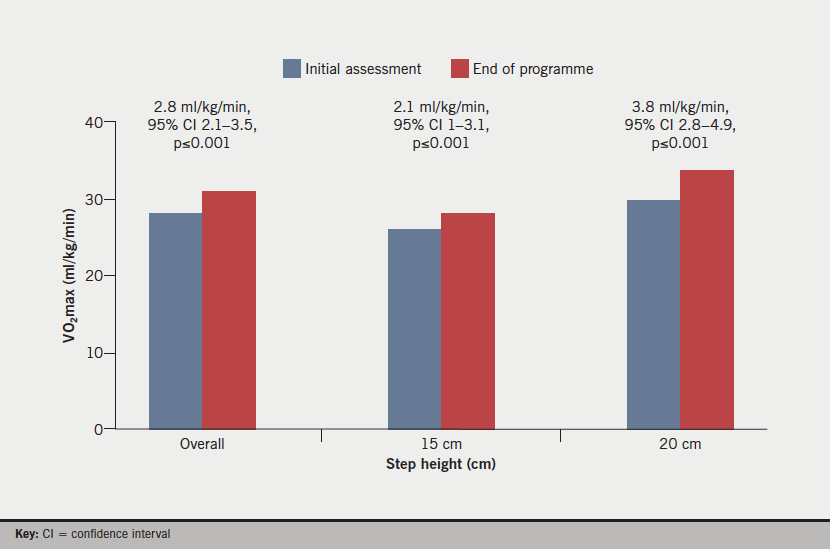
At the EOP assessment, the overall CST time increased from 346 ± 91 seconds to 402 ± 94 (55 seconds, 95% confidence interval [CI] 45 to 65, p≤0.001). The predicted VO2max across the three step heights increased from 28 ± 5.95 ml/kg/min at IA to 30.8 ± 6.65 ml/kg/min at EOP (2.8 ml/kg/min, 95% CI 2.1 to 3.5, p≤0.001). A subgroup analysis demonstrated that patients taking part in a 15 cm step height significantly increased their predicted VO2max from 25.9 ± 5.25 ml/kg/min at IA to 28 ± 5.25 ml/kg/min at EOP assessment (2.1 ml/kg/min, 95% CI 1 to 3.1, p≤0.001) and patients taking part in a 20 cm step height increased their predicted VO2max from 29.7 ± 5.6 ml/kg/min at IA to 33.6 ± 5.6 ml/kg/min at EOP assessment (3.8 ml/kg/min, 95% CI 2.8 to 4.9, p≤0.001) (figure 3).
Changes in predicted O2 pulse
Overall, O2 pulse increased from 14.2 ml/beat to 14.8 ml/beat (0.6 ml/min, 95% CI 0.5 to 0.7, p≤0.001) at the EOP with the largest change occurring at stage 4, with a mean increase of 1.2 ml/beat (95% CI 0.4 to 1.9, p≤0.007). On a 15 cm step height, O2 pulse significantly increased at EOP assessment from 13.2 ± 2.8 ml/beat to 13.6 ± 2.7 ml/beat (0.4 ml/beat, 95% CI 0.3 to 0.6, p≤0.001) and from 14.9 ± 2.4 ml/beat to 15.6 ± 2.8 ml/beat (0.7 ml/beat, 95% CI 0.5 to 0.9, p≤0.001) on a 20 cm step height. Table 2 demonstrates the overall changes in O2 pulse.

Changes in submaximal heart rate
Overall HR on average decreased by 4.1 bpm (95% CI –5.0 to –3.2, p≤0.001) with smaller reductions at stage 1 (–3.1 bpm, 95% CI –4.5 to –1.8, p≤0.001) and larger reductions at stage 4 (–7.3 bpm, 95% CI –11.9 to –2.7, p≤0.004). In the subgroup analysis, HR on average decreased by –2.8 bpm (95% CI –1 to –4.6, p≤0.001) on stage 1 with a larger reduction of 7.2 bpm at stage 4 (95% CI –0.8 to –15, p≤0.03) on a 15 cm step height. These trends were similar for a 20 cm step height with smaller reductions in HR at stage 1 (–3.3 bpm, 95% CI –1.1 to –5.6, p≤0.001) and larger reductions at stage 4 (–6.5 bpm, 95% CI –1.5 to –14.7, p≤0.04).
Discussion
The aim of this study was to apply the O2 pulse ratio to determine if the improvement in exercise performance on the CST is related to a true physiology adaptation following the Westminster MyAction programme. The results of this study demonstrated that the performance on the CST increased by 16%, with a subsequent increase in predicted VO2max across the three step heights from 28 ± 5.95 ml/kg/min to 30.8 ± 6.65 ml/kg/min (2.8 ml/kg/min, 95% CI 2.1 to 3.5, p≤0.001) at the EOP assessment. The O2 pulse significantly increased from 14.2 ml/min to 14.8 ml/min (0.6 ml/min, 95% CI 0.5 to 0.7, p≤0.001) at the EOP assessment demonstrating that a true physiological adaptation had occurred following the exercise sessions.
One of the main mechanisms that contributed towards both the improvement in predicted VO2max and O2 pulse in this study was related to the reduction in the submaximal HR response on each stage of the CST (table 3). A reduction in the submaximal HR is a classical physiological training adaptation and is suggestive of an adjustment in the autonomic balance between parasympathetic and sympathetic nervous activity, resulting in the proficiency of the myocardium to accomplish a similar cardiac output at a lower myocardial oxygen demand.12-14 These favourable adaptations also allow for a greater ventricular filling time,15 enhanced coronary perfusion,16 and a lower rate pressure product.17 Such changes have been associated with a reduction in myocardial ischaemia and lower risk of arrhythmias.13,17

The magnitude of the reduction in the submaximal HR response appears to be dependent on the exercise training intensity and volume. In the present study, patients attended a supervised exercise session once per week for up to 12 weeks and they were encouraged to participate in a home exercise programme two to three times per week. During the supervised exercise sessions, patients worked between 40% and 70% of their age-predicted HR reserve max and/or a RPE of 11–14 on the Borg 6–20 scale.18 Working at this intensity resulted in an overall submaximal HR reduction of –4.1 bpm (95% CI –5.0 to –3.2, p≤0.001) with larger reductions at stage 4 of around 7.3 bpm (95% CI –11.9 to –2.7, p≤0.004). There were insufficient numbers to calculate a meaningful reduction in submaximal HR at stage 5. However, one patient who completed stage 5 on a 25 cm step height achieved a 24 bpm reduction in their submaximal HR response after completing the MyAction programme. In support of these findings, a recent randomised-controlled trial of 140 patients with an abdominal aortic aneurysm, demonstrated a 7–14 bpm reduction in their submaximal HR response during exercise testing following a high exercise volume (1,999 ± 1,030 kcal/week energy expenditure) and a high intensity (98.8% of HR training zone) exercise programme.14
Despite the positive outcomes of the present study, it is important to acknowledge the main study limitations. The majority of the patients (75%) were stratified as high multi-factorial risk, therefore, limiting the applicability of the results to programmes only offering cardiovascular prevention and rehabilitation to those with established cardiovascular disease. The second limitation is that the data were collected from clinical practice with no control group and it needs to be verified in a randomised prospective study design. The third limitation is related to O2 pulse, which is normally measured through direct gas analysis during maximal cardiopulmonary exercise testing. In the present study, O2 pulse was estimated from the predicted VO2 on each stage of the CST. Such predictions in VO2 using metabolic calculations are open to considerable individual variability, especially in patients with known heart disease.19,20 In addition, extrinsic variables, such as room temperature, were not controlled, which could potentially influence the HR response during the CST. Future research is needed to control for these variables and should also confirm what difference would be clinically meaningful to the patient.
Acknowledgement
The authors would like to acknowledge the support of Paul Bassett, Imperial College London, for his help with the statistical analysis.
Conflict of interest
None declared.
Key messages
- This service analysis demonstrates that the Westminster MyAction cardiovascular prevention and rehabilitation programme favourably influenced predicted VO2max and submaximal O2 pulse
- An increase in predicted VO2 and submaximal O2 pulse appears to be driven by a reduction in the submaximal heart rate response across 4 stages of the Chester step test (CST) at three different step heights
- Patients following a 12-week structured exercise programme consisting of a supervised exercise session and a home programme performed two to three times per week can expect to save up to seven heart beats on the CST, which could potentially reduce myocardial ischaemia and lower risk of arrhythmias during exercise
References
1. British Association for Cardiovascular Prevention and Rehabilitation. The BACPR standards and core components for cardiovascular disease prevention and rehabilitation. London: BACPR, 2012. Available from: http://www.bacpr.com/resources/8BZ_BACPR_Standards_and_Core_Components_2012.pdf [accessed May 2016].
2. Association of Chartered Physiotherapists in Cardiac Rehabilitation. Standards for physical activity and exercise in the cardiac population. ACPICR, 2014. Available from: http://acpicr.com/publications
3. Guyatt GH, Pugsley SO, Sullivan MJ et al. Effect of encouragement on walking test performance. Thorax 1984;39:818–22. https://doi.org/10.1136/thx.39.11.818
4. Jolly K, Taylor RS, Lip GY, Singh S; BRUM Steering Committee. Reproducibility and safety of the incremental shuttle walking test for cardiac rehabilitation. Int J Cardiol 2008;125:144–5. https://doi.org/10.1016/j.ijcard.2007.01.037
5. Bellet RN, Adams L, Morris NR. The 6-minute walk test in outpatient cardiac rehabilitation: validity, reliability and responsiveness – a systematic review. Physiotherapy 2012;98:277–86. https://doi.org/10.1016/j.physio.2011.11.003
6. Buckley JP, Reardon M, Innes G, Morris M. Using a heart rate walking speed index to report truer physiological changes when using walking performance tests in cardiac rehabilitation. J Cardiopulmon Rehabil Prevent 2010;30:346–7. https://doi.org/10.1097/HCR.0b013e3181f3a88f
7. Hippisley-Cox J, Coupland C, Vinogradova Y et al. Predicting cardiovascular risk in England and Wales: prospective derivation and validation of QRISK2. BMJ 2008;336:a332. https://doi.org/10.1136/bmj.39609.449676.25
8. Wood DA, Kotseva K, Connolly S et al. Nurse-coordinated multidisciplinary, family-based cardiovascular disease prevention programme (EUROACTION) for patients with coronary heart disease and asymptomatic individuals at high risk of cardiovascular disease: a paired, cluster-randomised controlled trial. Lancet 2008;371:1999–2012. https://doi.org/10.1016/S0140-6736(08)60868-5
9. Sykes K. Chester Step Test; Resource Pack (Version 3). Cheshire, UK: Chester College of Higher Education, 1998.
10. Wasserman K, Hansen J, Sietsema K et al. Principles of Exercise Testing and Interpretation: Including Pathophysiology and Clinical Applications. 5th revised edition. London: Lippincott Williams and Wilkins, 2011.
11. Oliveira RB, Myers J, Soares de Arau CG. Long-term stability of the oxygen pulse curve during maximal exercise. Clinics 2011;66:203–09. https://doi.org/10.1590/S1807-59322011000200004
12. Ehsani AA, Martin WH 3rd, Heath GW, Coyle EF. Cardiac effects of prolonged and intense exercise training in patients with coronary artery disease. Am J Cardiol 1982;50:246–54. https://doi.org/10.1016/0002-9149(82)90173-4
13. Malfatto G, Facchini M, Bragato R et al. Short and long term effects of exercise training on the tonic autonomic modulation of heart rate variability after myocardial infarction. Eur Heart J 1996;17:532–8. https://doi.org/10.1093/oxfordjournals.eurheartj.a014905
14. Myers J, McElrath M, Jaffe A et al. A randomized trial of exercise training in abdominal aortic aneurysm disease. Med Sci Sports Exerc 2014;46:2–9. https://doi.org/10.1249/MSS.0b013e3182a088b8
15. Belardinelli R, Georgiou D, Cianci G et al. Exercise training improves left ventricular diastolic filling in patients with dilated cardiomyopathy. Circulation 1995;91:2775–84. https://doi.org/10.1161/01.CIR.91.11.2775
16. Redwood DR, Rosing DR, Epstein SE. Circulatory and symptomatic effects of physical training in patients with coronary-artery disease and angina pectoris. N Engl J Med 1972;286:959–65. https://doi.org/10.1056/NEJM197205042861801
17. May GA, Nagle FJ. Changes in rate-pressure product with physical training of individuals with coronary artery disease. Phys Ther 1984;64:1361–6. Available from: http://ptjournal.apta.org/content/64/9/1361.long
18. Borg G. Borg’s Perceived Exertion and Pain Scales. Leeds: Human Kinetics, 2008.
19. Byrne NM, Hills AP, Hunter GR et al. Metabolic equivalent: one size does not fit all. J Appl Physiol 2005;99:1112–19. https://doi.org/10.1152/japplphysiol.00023.2004
20. Woolf-May K, Ferrett D. Metabolic equivalents during the 10-m shuttle walking test for post-myocardial infarction patients. Br J Sports Med 2008;42:36–41. https://doi.org/10.1136/bjsm.2006.034116
