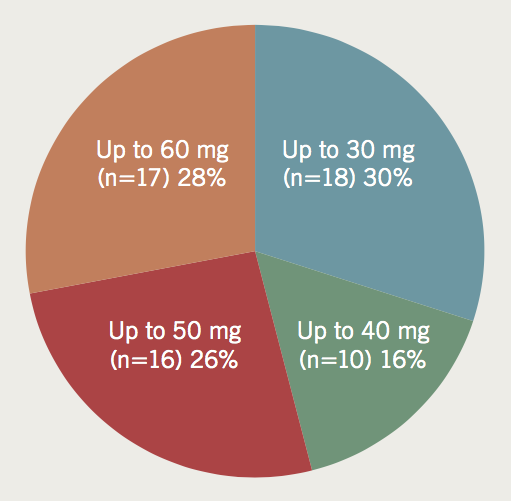
To examine the current practice of British Society of Cardiovascular Imaging (BSCI) members in the administration of beta blockers in computed tomography (CT) coronary angiography (CTCA) a 10-point online questionnaire was emailed to all registered members of the British Society of Cardiovascular Imaging. There were 61 respondents: 75% give intravenous (IV) metoprolol in the CT department, the rest a combination of oral and/or IV dosing. Over 50% were happy to administer 50 mg or more. No serious complications related to drug administration had been seen by 82%. Of the remaining 18%, half (six reports) documented severe hypotension and two reported a death. No physical observations were taken by 25%, at any point. Another 27% checked blood pressure before the scan only, 17% measured blood pressure before the scan and immediately after and 28% measured before the scan and after with a delay.
In conclusion, among BSCI members, there is no uniform strategy regarding the route or dose of beta blocker administration, or if, when and what physical observations should be performed. Several severe adverse events have been documented, including two deaths. This, however, is in the context of the large volume of CTCAs performed nationally, and so, despite some doses of beta blocker exceeding British National Formulary recommendations, this appears safe.
Introduction
Even with modern high spatial and temporal resolution scanners, image quality obtained during computed tomography (CT) coronary angiography (CTCA) remains highly dependent on stable, regular, low heart rates. To achieve this pre-scan oral and/or intravenous beta blockade is widely used. Anecdotal and published reports suggest a wide variation in the route of administration and quantities of beta blocker used, particularly the intravenous route.1-7 Doses used are commonly far in excess of that recommended by the British National Formulary (BNF)8 to achieve adequate heart rate reduction. This study examines the current CTCA-related practice surrounding the administration of beta blockers in the UK, and the evidence for their usage in this setting.
Materials and methods
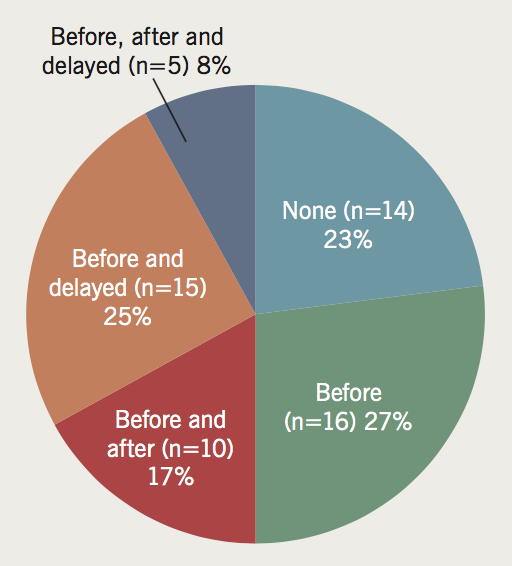
A 10-point online questionnaire (table 1) was emailed to the British Society of Cardiovascular Imaging (BSCI) in December 2013 who then forwarded this to all their registered members. BSCI members make up the majority of CTCA practitioners in the UK making them a highly representative sample.
The questionnaire was created and data gathered using the SurveyMonkey online tool.9 The questions included: numbers of scans performed per centre, who supervises the scan, knowledge of pharmacokinetics, drug administration and contraindications, aimed for target heart rates, reports of serious complications and physical observations taken during CTCA. Seven questions allowed a single response only, while the others allowed multiple responses and free text comments. In the multiple-response questions some deliberately incorrect options were offered.
Responses to questions were transferred to Microsoft Excel as absolute numbers. Percentages were calculated fusing Excel’s built-in programming and formatting capabilities. Free text comments were analysed for content and are reported verbatim.
Results
The questionnaire was returned by 61 respondents: 60 completed the full survey, with one respondent not answering the question regarding physical observations. The number of questionnaires sent out by the BSCI to members was 235 (26% response rate). It must be noted that the denominator represents individual members, not cardiac CT centres, and, therefore, the representation of national current practice is likely to be much higher.
Responses to questions
Q1: Roughly how many cardiac CT scans does your department perform a year?
Two (3%) respondents are performing less than 100, 16 (27%) perform 100–300, 24 (39%) perform 300–500 and 19 (31%) perform over 500 scans per year.
Q2: Who supervises the scans?
Of respondents, 30 (49%) work in centres where radiologists and cardiologists jointly supervise scans; of the rest, 24 (39%) are radiologists only and seven (12%) cardiologists only.
Q3: How are beta blockers usually administered?
Of respondents, 46 (75%) administer metoprolol intravenous (IV) only (40 on the CT table and six in the preparation room). The remaining 15 (25%) use oral beta blockers, topping up with more oral dosing (on attendance or an hour before the scan) or IV beta blocker on the table.
Q4: What would usually prevent you from administering IV beta blocker?
Practically all responders (59 of 61, 97%) stated that severe asthma (e.g. intensive therapy unit [ITU] admission in the last 12 months) was a contraindication but only four (7%) said that any asthma history would stop them using beta blockers. Concurrent verapamil therapy would deter beta blocker administration for 38 (62%). Heart block and poor left ventricular (LV) function were stated by 27 (44%) and 25 (41%), respectively. Other calcium channel blockers and pulmonary hypertension were indicated by 11 (18%). Ten (16%) respondents stated hypoglycaemia as a contraindication.
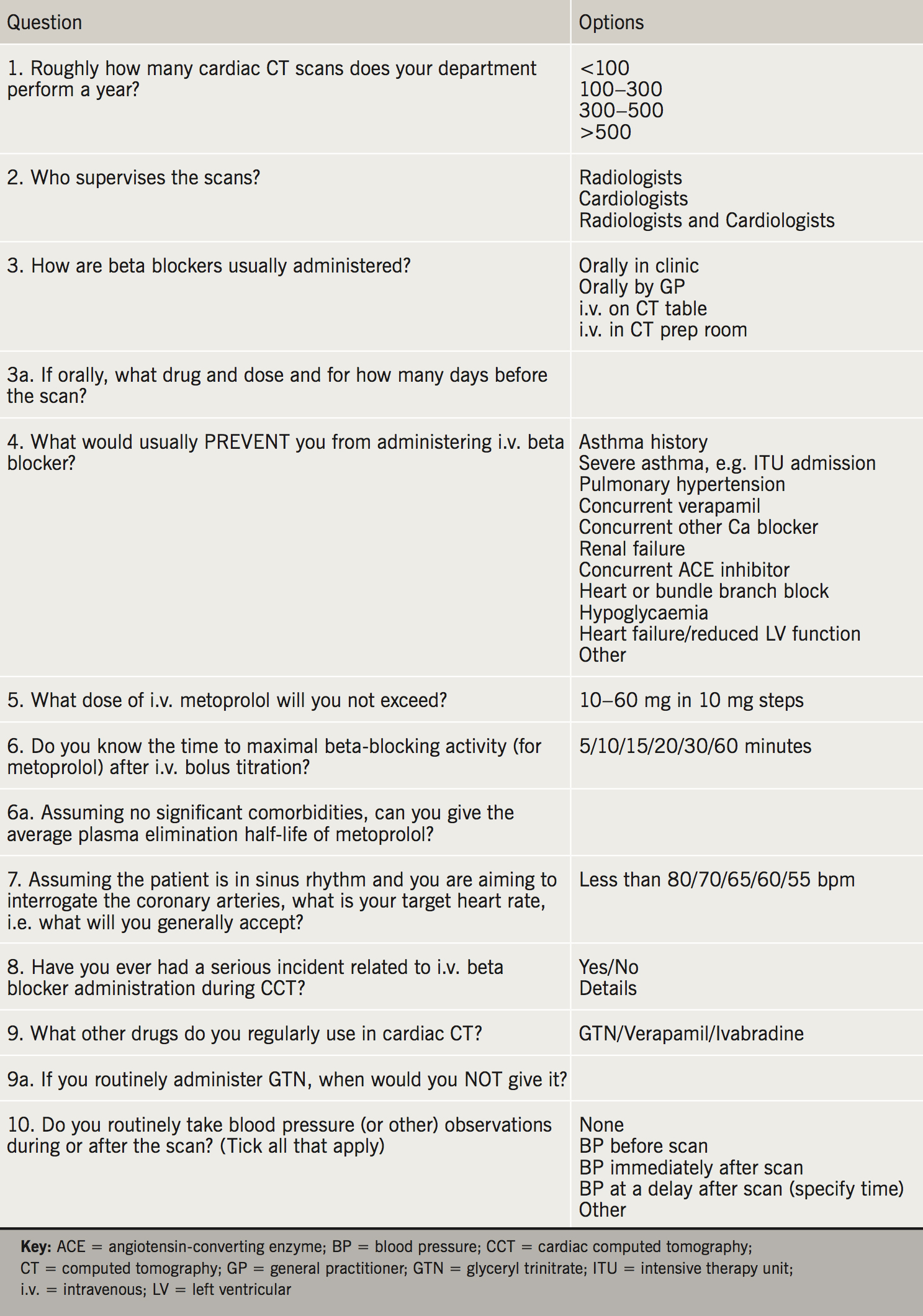
Q5: What dose of IV metoprolol will you not exceed?
Of respondents, 18 (30%) were prepared to administer up to 30 mg, another 10 (16%) up to 40 mg, another 16 (26%) up to 50 mg and a further 17 (28%) up to 60 mg (figure 1).
Q6: Do you know the time to maximal beta blocking activity (for metoprolol) after IV bolus titration? [Correct answer = 20 minutes]
Over half (36 respondents, 59%) thought it was less than 10 minutes, nine (15%) thought 15 minutes and 13 (21%) thought 20 minutes. The remaining three (5%) respondents indicated 30 minutes or more.
Q6a: Assuming no significant comorbidities, do you know the average plasma elimination half-life of metoprolol? [Correct answer = three to four hours]
Of 34 respondents, four (12%) didn’t know. Seven (21%) said up to 30 minutes, four (12%) said two to three hours and 14 (41%) said three to four hours. The remaining five (15%) thought that it was between six and eight hours.
Q7: Assuming the patient is in sinus rhythm and you are aiming to interrogate the coronary arteries, what is your target heart rate, i.e. what will you generally accept?
Four (7%) stated 55 beats per minute (bpm) or less, another 37 (61%) less than 60 bpm, 14 (23%) less than 65 bpm and two (4%) less than 80 bpm (four other respondents gave qualitative answers).
Q8: Have you ever had a serious incident related to IV beta blocker administration during cardiac CT?
No serious complications was stated by 50 respondents. The remaining 11 (18%) reported the following:
- “Cardiovascular collapse of one patient [who] had an ejection fraction of <15% but this was not stated on the form. Patient went to ITU and survived. One other patient had severe aortic stenosis [that was also] not stated on the form.”
- “Severe hypotension when administered in a patient who had received oral verapamil that day.”
- “Death in one patient with pulmonary hypertension, given beta blockers, GTN [glyceryl trinitrate] and IV contrast.”
- “Severe heart failure requiring inotrope support in a patient with heart failure given oral beta blockers.”
- “Severe hypoglycaemia in one patient given oral beta blockers.”
- “One death. Consultant cardiologist present. Went to coroners.”
- “Symptomatic complete heart block. Happy to deal with this and organised for overnight monitoring.”
- “Hypotension in patient also on digoxin and diltiazem. Dealt with and referred for admission/observation.”
- “Extreme bradycardia requiring [resuscitation] team assistance.”
Q9: What other drugs do you regularly use in cardiac CT?
GTN regularly used by 46 (75%) respondents, two (3%) use verapamil and 11 (17%) use ivabradine.
Q9a: If you routinely administer GTN, when would you not give it?
Of 28 responses, 13 (46%) and six (21%) listed aortic stenosis and hypotension, respectively. There were three replies each (11%) for patient refusal, hypersensitivity and concurrent phosphodiesterase inhibitor use.
Q10: Do you routinely take blood pressure (or other) observations during or after the scan?
Of 60 respondents, 14 (23%) took no blood pressure (BP) or pulse measurements at all, at any point (figure 2). Only 17 (28%) took a delayed measurement post-scan. In the six comments where the delay time was noted, this was between 10 and 30 minutes.
Discussion
Number of scans
Current BSCI guidelines state only that at least 100 CTCA examinations should be performed each year to maintain personal accreditation.10 Our data have found that only 3% of respondents are performing less than the required 100 scans per year. (At our site we have seen a dramatic increase in requests in the last few years, not least since the publication of the National Institute for Health and Care Excellence [NICE] CG95 in 2010 and more especially since its 2016 revision.)11 Therefore, we are confident that conclusions drawn from the data obtained are from the context of experienced CTCA performing centres.
Supervising personnel
The current BSCI service specification (2012) regarding scan supervision, states that, “it remains the responsibility of individual clinicians to ensure that they are suitably trained and competent to provide the service that is offered” and “that at least one member of the workforce (for any given session) should be trained and certified in advanced life support [if heart rate reducing drugs are used]”. Half of respondents supervise scans jointly (radiologists and cardiologists working together) with the rest having one or the other. The authors would like to point out that the service specification document also recommends a combined, synergistic radiology/cardiology approach to the reporting of cardiac CT scans,12 with the radiologists assisting the cardiologists by reporting on lung and other parenchymal findings.
Beta blocker administration
Route of administration
Several different protocols for beta blocker administration have been published and include oral only (2.5–150 mg), staggered dosing (50–100 mg), a combination of oral and IV medication and finally IV only (2.5–70 mg).1-7 In our survey, three quarters of respondents use IV beta blocker, usually on the CT table with the rest employing various oral dosage schedules, frequently with IV beta blocker top-up.
Contraindications
- Nearly all respondents (97%) stated severe asthma, e.g. ITU admission, as a contraindication that would prevent them from using a beta blocker. There are multiple statements in the medical literature stating any asthma history is a relative or absolute contraindication to beta blocker administration, or advising at least extreme caution. Anecdotal and published statements suggest that in cases of non-severe asthma, some practitioners do choose to give IV beta blockers but up to a limited maximum dose (10 mg and 15 mg have been quoted as values for this).7 With only 7% of respondents unwilling to proceed with beta blockers in cases of any asthma history, it seems likely that the rest (93%) are using some form of beta blocker dosing schedule, reduced dose or otherwise.
- Of respondents, 62% viewed concurrent administration of verapamil as a contraindication, thereby, suggesting that 38% do not. The British Hypertensive Society advises extreme caution when co-administering beta blocker and rate-limiting calcium channel blockers (verapamil and diltiazem) because of the risk of heart block and potentially fatal bradyarrhythmias.13 Furthermore, the BNF recommends concurrent administration of verapamil and beta blockers be avoided because of the risk of asystole, severe hypotension and heart failure.8
- Five respondents listed renal failure as a contraindication, whereas the BNF counsels caution and reduced dosage only. In fact, the lipid soluble beta blockers, such as metoprolol, labetolol, pindolol and propanolol, are typically metabolised by the liver. It is the water soluble beta blockers such as atenolol that are renally excreted. (The metoprolol manufacturer data sheet does not state that dose be reduced for renal impairment.)14
In the authors’ experience it is ignorance of severe aortic stenosis, heart failure or asthma (which may be known but not divulged on the request card or not revealed by the patient) that most often causes a CTCA practitioner to experience problems. Therefore, referring clinicians should be encouraged to include all relevant information on request (as the standards document recommends) and that all patients be assessed by an appropriate staff member prior to beta blocker administration. Specific questions should be asked about verapamil treatment, heart block, valvular heart disease, heart failure and asthma, summarised in table 1. An electronic order communications system at our institution prompts the referrer to divulge information about asthma and contraindications to beta blockade, but these are variably completed, a concern given the potential implications.
Maximum dosage
Published data reveal a wide range of intravenous IV metoprolol dosages. In our survey, over half of respondents were willing to administer 40–60 mg with only a third unwilling to exceed 30 mg. (One respondent stated that the highest dose they had given was 100 mg oral metoprolol followed by a further 80 mg IV). The BNF recommends a maximum IV dose of 15 mg for any indications, administered at no more than 5 mg every two minutes. Despite this, the standards document reports that a few centres administer up to 50 mg of IV metoprolol with no reported adverse effects,16 suggesting to practitioners that this is safe practice. (Of note, outside cardiac CT, a study of pain relief following IV metoprolol in patients with acute myocardial infarction [MI] saw doses of up to 180 mg administered over 70 minutes.)15
Thus, a paradigm seems to have developed that, despite the cautious BNF dosing advice, IV beta blockers are very safe and, indeed, one respondent replied that he/she had performed over 10,000 studies with no adverse effects at all. Furthermore, two recent publications describe administration of up to 70 mg of IV metoprolol with a low rate of major complications in one (0.44%),5 and no adverse clinical events at all in the other.7 Meanwhile, in this survey, we have learnt of one in five respondents having experienced some kind of serious untoward event, two deaths and several hospital admissions, some to ITU. Any death related to high CTCA-related metoprolol dosage, if genuinely attributable, is clearly concerning. The legal ramifications when a patient comes to harm after the administration of up to five times the maximum dose recommended by the BNF are unknown. However, the concurrent administration of intravenous contrast is a confounding variable and, given the very large numbers of patients receiving sizeable IV beta blocker doses during CTCA nationwide, with few published untoward effects or adverse events, high-dose beta blocker dosage may indeed be ‘safe’. The authors have contacted the BNF editorial team on several occasions asking for mechanisms to consider re-evaluating their advice on IV metoprolol doses but have not, as yet, received a reply. Nonetheless, cardiac CT training programmes might like to consider the assessment of advanced or even basic competencies in life support as suggested by the new cardiac CT standards document, published jointly by Royal College of Radiologists, BSCI and Royal College of Physicians.10,16
Pharmacokinetics
The widely accepted time to maximal activity for IV metoprolol when administered over a 10-minute period is 20 minutes.17,18 Well over half (59%) of respondents stated that the maximal time was 10 minutes or less. Metoprolol is a cardioselective beta1-antagonist that becomes less cardioselective at higher doses. It is metabolised by the liver and has a dose-related half-life of 3–4 hours. Of those that replied, only a quarter stated this time correctly with 32% either not knowing at all or stating 30 minutes or less. One respondent mentioned genetic liver enzyme variations, which can increase the half-life by a further six hours. Absence of the CYP2D6 hepatic pathway (in 8% Caucasians, 2% others) causes a several-fold increase and prolongation of metoprolol plasma concentration. Other causes of hepatic impairment will also affect the half-life and elimination of metoprolol.18
Clinicians performing this examination have a duty to know about the pharmacokinetics of the drugs they are administering to ensure optimal safety for their patients.
Target heart rate
The standards document states a heart rate of less than 65 bpm should be achieved for all scans, provided it is safe and practical to do so.16 Of our respondents, 91% aimed to achieve less than 65 bpm, although the majority were aiming for values even less than this. It will be interesting to see how these figures change, if at all, as the new generation of high-specification scanners become more widely available.
Serious incidents
Themes from the incidents reported in this survey suggest that significant LV impairment or concomitant severe valvular pathology may be important contributors. Clinicians should be aware of these comorbidities and take exceptional care when administering IV beta blockers in these settings. Concomitant atrioventricular (AV) nodal blocking agents that the patients are already taking (e.g. verapamil or digoxin) may also have been contributory in several cases. We note only 62% of clinicians said that current verapamil therapy would deter them from giving beta blockers and this potentially harmful interaction may need further highlighting. The well-recognised complication of bradycardia and heart block was documented twice, but both patients appear to have been successfully managed through this. Interestingly, despite the widespread concern about the induction of an asthma attack by beta blockers, no such events were reported. This seems to suggest that the practice of 97% of the respondents to only withhold beta blocker from patients with severe asthma may be safe.
Other drugs employed
The majority of respondents to this question (75%) use sublingual GTN. Unfortunately, only 28 respondents answered our question on what would cause them not to administer GTN and each of them only gave a single answer to this. Despite all the answers being correct as per the BNF19 (aortic stenosis, hypotension, hypersensitivity, concurrent phosphodiesterase inhibitor use), little conclusion can be made on the BSCI member’s knowledge of GTN contraindications due to the poor question response. (Data sheet and BNF contraindications for GTN also include: raised intracranial pressure, anaemia, closed angle glaucoma, cerebrovascular disease, hepatic and renal impairment. Its use is also cautioned in any condition where adequate preload is important for maintaining cardiac output; such as hypertrophic cardiomyopathy, pericardial constriction and severe mitral stenosis.)
Physical observations
Just under a quarter (23%) of respondents took no BP measurements at any point during patient attendance. After IV administration some studies advise a 30-minute observation period after the scan,2,3 but only 28% of respondents reported any post-scan measurements and only two stated a delay of 30 minutes. The new standards document makes reference to review of patients prior to discharge from the department, which seems sensible given the large doses of beta blockers employed.
Limitations
This is a survey, and as such relies on anecdotal evidence rather than controlled trial data. It is also difficult to gauge the number of centres responding, as opposed to individual members, given the anonymous nature of the survey. Nevertheless, we feel this represents a useful and informative insight into contemporary cardiac CT practice in the UK.
Conclusion
Among BSCI members there is no uniform strategy regarding the route or dose of beta blocker administration. There is also no consensus on what physical observations should be performed and their timing. A wide variation in the knowledge base surrounding the pharmacokinetics of beta blocker has been highlighted with potential for patient harm and drug interactions. Several severe adverse events have occurred after the administration of beta blockers, including two deaths. But given the tens of thousands of CTCAs being performed in the UK annually (38,455 in 2015 alone)20 it would appear that, overall, this represents a very small proportion, despite doses of IV metoprolol considerably in excess of that recommended by the BNF. Nevertheless, despite its apparent safety, the authors’ would like to reaffirm the existence of the standards documents released by the BSCI, Royal College of Radiologists and Royal College of Physicians, which provides advice on how these scans and the use of metoprolol should be approached, and to encourage its adoption among clinicians supervising CTCA studies.
Acknowledgement
The authors would like to acknowledge the assistance of the British Society of Cardiovascular Imaging in the collection of our data, through the distribution of our survey among its members.
Conflict of interest
None declared.
Key messages
- There is no uniform strategy for beta blocker administration (route/dose) or monitoring among British Society of Cardiovascular Imaging members
- The majority of beta blocker doses given exceed the British National Formulary recommendations
- There have been minimal adverse reactions due to higher than recommended doses
References
1. Maurer MH, Zimmermann E, Schlattmann P, Germershausen C, Hamm B, Dewey M. Indications, imaging technique, and reading of cardiac computed tomography: survey of clinical practice. Eur Radiol 2012;22:59–72. https://doi.org/10.1007/s00330-011-2239-7
2. McParland P, Nicol ED, Harden SP. Cardiac drugs used in cross-sectional cardiac imaging: what the radiologist needs to know. Clin Radiol 2010;65:677–84. https://doi.org/10.1016/j.crad.2010.04.002
3. Pannu HK, Alvarez W, Fishman EK. Beta-blockers for cardiac CT: a primer for the radiologist. AJR Am J Roentgenol 2006;186(6 suppl 2):S341–S345. https://doi.org/10.2214/AJR.04.1944
4. Sabarudin A, Sun Z. Beta-blocker administration protocol for prospectively ECG-triggered coronary CT angiography. World J Cardiol 2013;5:453–9. https://doi.org/10.4330/wjc.v5.i12.453
5. Kassamali R, Kim D, Patel H et al. Safety of an IV beta-adrenergic blockade protocol for heart rate optimisation before coronary CT angiography. AJR Am J Roentgenol 2014;203:759–62. https://doi.org/10.2214/AJR.13.11492
6. Roberts WT, Wright AR, Timmis JB, Timmis AD. Safety and efficacy of a rate control protocol for cardiac CT. Br J Radiol 2009;82:267–71. https://doi.org/10.1259/bjr/24574758
7. Raju VM, Gosling OE, Morgan-Hughes G et al. High-dose intravenous metoprolol usage for reducing heart rate at CT coronary angiography: efficacy and safety. Clin Radiol 2014;69:739–44. https://doi.org/10.1016/j.crad.2014.03.003
8. British National Formulary. Metoprolol tartrate. Available at: https://bnf.nice.org.uk/drug/metoprolol-tartrate.html
9. SurveyMonkey Inc. SurveyMonkey: free online survey software & questionnaire tool. Available at: https://www.surveymonkey.com/
10. British Society of Cardiovascular Imaging. Recommended standards in ECG gated cardiac CT training: British Society of Cardiac Imaging (BSCI). Available at: http://www.bsci.org.uk/education-accreditation/accreditation
11. National Institute for Health and Care Excellence. Chest pain of recent onset. CG95. London: NICE, 2010. Available from: https://www.nice.org.uk/guidance/CG95
12. British Society of Cardiovascular Imaging. CT coronary angiography service specification from the British Society of Cardiovascular Imaging (BSCI). May 2012:1–15. Available at: http://www.bsci.org.uk/standards-guidelines/ct-coronary-angiography-service-specification
13. British Hypertension Society. Beta-adrenoceptor antagonists (beta-blockers). Available at: http://www.bhsoc.org/pdfs/therapeutics/Beta-adrenoceptor%20Antagonists%20(Beta-Blockers).pdf
14. Drugs.com. Metoprolol. Available at: https://www.drugs.com/pro/metoprolol.html
15. Everts B, Karlson B, Herlitz J, Abdon N-J, Hedner T. Effects and pharmacokinetics of high dose metoprolol on chest pain in patients with suspected or definite acute myocardial infarction. Eur J Clin Pharmacol 1997;53:23–31. https://doi.org/10.1007/s002280050332
16. Royal College of Radiologists. Standards of practice of CTCA in adult patients. London: Royal College of Radiologists, 2014. Available from: http://www.rcr.ac.uk/docs/radiology/pdf/BFCR14(16)_CTCA.pdf
17. Novartis. Lopressor® metoprolol tartrate injection, USP. Available at: http://www.pharma.us.novartis.com/product/pi/pdf/lopressor.pdf
18. Lochan R, Silke B, Taylor S. Speed of onset of pharmacodynamic activity of propranolol, practolol, oxprenolol and metoprolol after intravenous infection in man. Br J Clin Pharmacol 1981;12:721–4. https://doi.org/10.1111/j.1365-2125.1981.tb01295.x
19. British National Formulary. Glyceryl trinitrate. Available at: https://bnf.nice.org.uk/drug/glyceryl-trinitrate.html
20. British Society of Cardiovascular Imaging. The challenge of national CT Coronary Angiography (CTCA) provision in response to NICE CG95 update 2016. London: British Society of Cardiovascular Imaging, 2016. Available from: http://www.bsci.org.uk/images/Documents/2016_BSCI_BSCCT_response_to_NICE_CG95.pdf

