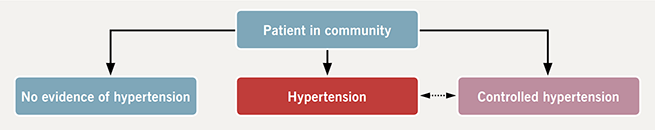
We believe that controlled systemic hypertension should be considered as an important clinical entity (figure 1). We know that cardiovascular risks increase with rising blood pressure, each 2 mmHg increase in systolic blood pressure is associated with a 7% and 10% rise in mortality from ischaemic heart disease and stroke, respectively.1 However, the converse proposition would also seem to be true. Meta-analyses have found significant reductions in stroke and coronary events associated with blood pressure control,2 even in grade 1 hypertension. Furthermore, large studies such as SPRINT (Systolic Blood Pressure Intervention Trial)3 have shown that patients with tighter blood pressure control (mean systolic 121.4 mmHg) have significantly lower rates of major cardiovascular events and heart failure in addition to reduced mortality compared with the standard therapy cohort (mean systolic 136.2 mmHg). With reduction of blood pressure the associated risks are reduced.
Clinical significance
Controlled hypertension is likely clinically significant. Patients often receive prognostication or treatment upon the basis of a diagnosis of systemic hypertension. This is built upon the assumption that the patient risk profile is determined by a once proven diagnosis of systemic hypertension. However, if patients are successfully treated for their systemic hypertension they may in fact move from a higher risk group towards a lower risk group. This could result in some patients ultimately receiving inappropriate treatments.
For example, consider a relatively young male patient suffering from atrial fibrillation. He has a CHADS2VASC score of 1 based solely upon a diagnosis of systemic hypertension and is receiving formal anticoagulation. It is possible that a subsequent diagnosis of controlled hypertension might permit withdrawal of formal anticoagulation. We read with interest that hypertension can be a common reason for cancelling surgery.4 The label of controlled hypertension (meaning control over the medium rather than short term), when applied to those patients in whom blood pressure is sufficiently well controlled for their intervention, might permit more operations to proceed. The key idea here is that a diagnosis of controlled hypertension should apply to those patients who respond to antihypertensive treatment. Their overall management should consider the potential marginal contribution of blood pressure to their risk profile, which may be closer to that of the general population. Further research is merited here to formalise criteria.
Conflict of interest
None declared.
References
1. National Institute for Health and Care Excellence. Hypertension in adults: diagnosis and management. London: NICE, 2011. Available from: https://www.nice.org.uk/guidance/cg127
2. Thomopoulos C, Parati G, Zanchetti A. Effects of blood pressure lowering on outcome incidence in hypertension: 2. Effects at different baseline and achieved blood pressure levels-overview and meta-analyses of randomized trials. J Hypertens 2014;32:2296–304. https://doi.org/10.1097/HJH.0000000000000379
3. The Sprint Research Group. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med 2015;373:2103–16. https://doi.org/10.1056/NEJMoa1511939
4. Anderson S, Beckett N, Pichel A, McCormack T. Optimising BP measurement and treatment before elective surgery: taking the pressure off. Br J Cardiol 2017;24:11–12. https://doi.org/10.5837/bjc.2017.005

